Volume 2, Issue 1 (Continuously Updated 2019)
Func Disabil J 2019, 2(1): 54-63 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Saneii S H, Karamali Esmaili S. Rehabilitation in Autism Spectrum Disorder: A Look at Current Occupational Therapy Services in Iran. Func Disabil J 2019; 2 (1) :54-63
URL: http://fdj.iums.ac.ir/article-1-73-en.html
URL: http://fdj.iums.ac.ir/article-1-73-en.html
1- Assistant Professor, Department of Basic Sciences in Rehabilitation, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran
2- Assistant Professor, Department of Occupational Therapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran ,esmaeili.s@iums.ac.ir
2- Assistant Professor, Department of Occupational Therapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran ,
Full-Text [PDF 308 kb]
(1643 Downloads)
| Abstract (HTML) (3513 Views)
In order to achieve therapeutic goals in people with ASD, there are many therapeutic approaches in Occupational therapy (OT), including sensory, developmental, cognitive, social, intensive behavioral, and family-centered interventions (Case-Smith & Arbesman, 2008; Dammann, Althoff, Hope, & Ausderau, 2017; Miller-Kuhaneck, 2015). The studies of OT in ASD has different issues such as sensory integration (Pfeiffer, Koenig, Kinnealey et al., 2011), social skills training (Asher, 2014), somatosensory stimulation (Hodgetts & Hodgetts, 2007), floor-time (Dionne & Martini, 2011), family routines (Bagatell, Cram, Alvarez, & Loehle, 2014; Joosten & Safe, 2014), participation in everyday life (Ashburner, Rodger, Ziviani, & Hinder, 2015), play (Henning, Cordier, Wilkes‐Gillan, & Falkmer, 2016), use of technology (Wilkes‐Gillan & Joosten, 2016), and cognitive orientation to occupational performance (Rodger & Brandenburg, 2009). There are also OT studies that show the overall practice of therapists in ASD; for example Case-Smith and Arbesman (2008) reviewed OT interventions in ASD. Some studies like Watling et al. (1999) and Case-Smith and Miller (1999) in the USA, Kadar et al. (2012), and Ashburner et al. (2014) in Australia also examined the work conditions, interventions, and assessments used by Occupational therapists. The results of these studies indicate that the focus of assessments and interventions of American and Australian therapists is on sensory issues; they reported competency in the treatment of sensory problems in ASD, and even expressed the need for further education. In the review above, it is clear that the concentration of OT studies in ASD includes a variety of issues, but in practice, the focus is on sensory issues. Studies that reflect the practice of therapists can help them rethink their performance. No information is available on the practice of Iranian occupational therapists in ASD. A number of factors including priorities of clients, work setting (clinic, home, and school), available resources, evidence of effectiveness of a method, the therapist's experience and knowledge may interfere in selecting therapeutic interventions (Case-Smith & Arbesman, 2008). Training after graduation is necessary to achieve competency in some of the approaches mentioned above; so that it depends on certain conditions, such as motivation, possibility to attend in the training courses, needs of the workplace, and so on. These conditions lead therapists not to use all approaches in the treatment of ASD. In addition, assessment is a prerequisite of treatment. The assessment of people with ASD requires availability of the specific assessment tools and the skills to implement them. The above-mentioned factors clarify the necessity of evaluating Iranian occupational therapists’ practice in ASD.
Accordingly, the purpose of this study was to investigate the current practice of occupational therapy and answer some questions about occupational therapists’ practice in ASD, including the age range of people with ASD who receive OT services, causes of OT discontinuation, perceived competency and source of knowledge of therapists, interventions, assessments, and therapeutic models used in working with people with ASD.
The assessment instrument was a researcher-made questionnaire. The items of the questionnaire were prepared according to the research questions and by reviewing the existing literature on OT in ASD. The face and content validity of the questionnaire was evaluated by 11 expert occupational therapists. After obtaining the expert opinions, 5 items were removed from the 20 initial items, which had a content validity ratio (CVR) of less than 0.62 (Lawshe, 1975). The content validity index (CVI) for each remaining item was greater than 0.79, with the mean of 90.66. Consequently, the final questionnaire had a good validity for the present study.
To describe the occupational therapists’ practice, central indices and dispersion were used. Chi-square, Pearson and Spearman correlation coefficients were used to describe and demonstrate quantitative and qualitative correlation between ground and independent variables with the OT practice.
The mean of minimum age of clients with ASD was 3.28 and the mean of maximum age was 10.22 years; so they were in childhood stage. The type of services provided by the therapists included 95% individual treatment, 73% assessment, 62% education, 52% consultation, and 23% group therapy.
The centers where the therapists worked with children with ASD included 103 outpatients, 28 home-visit, 26 exceptional schools, and 2 normal schools.
50.8% of the respondents reported that their competency to treat ASD is higher than average, and the rest reported moderate (45.2%), and lower than average (4%) competency.
The reasons for the discontinuation of OT were economic problems (79%), lack of cooperation of parents for going to OT (37.9%), lack of cooperation of the child with the therapist while doing therapeutic activities (14.5%), lack of expected change in the child (13.7%) and failure to reach the therapeutic goals (9.7%).
The source of knowledge for occupational therapists on ASD were classroom pamphlets, 53.2%, workshops, 51.6%, the internet, 62.9%, retraining courses, 31.5%, and books, 84.7%.
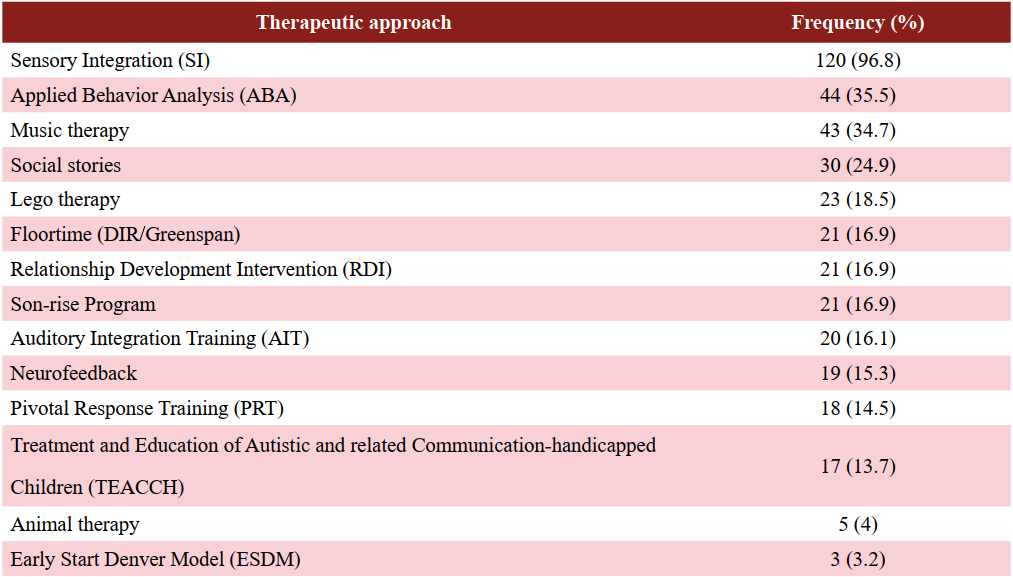
The OTs participating in this study were asked about the therapeutic areas that they were assessing and treating in children with ASD; the details are shown in Table 2.
Table2. The therapeutic areas were assessed and treated by occupational therapists in children with
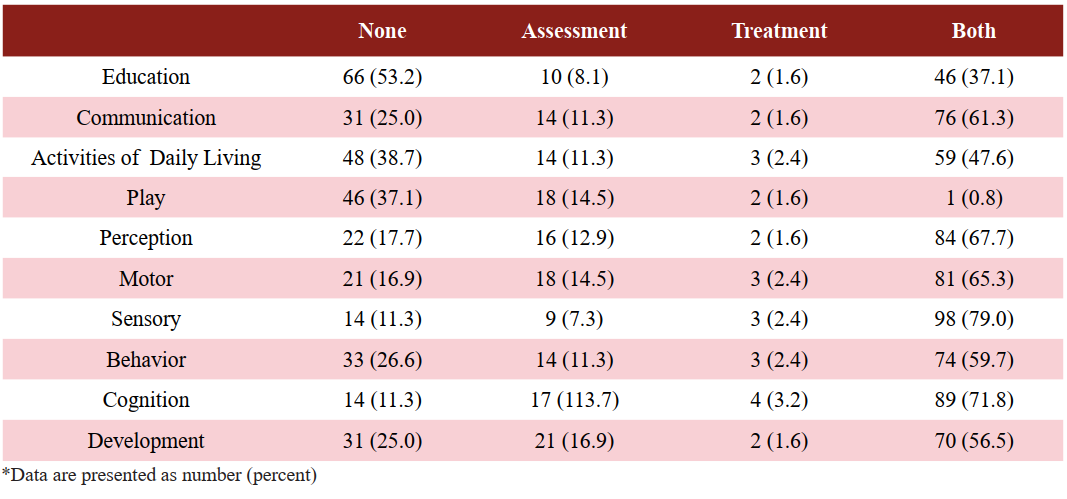
The therapeutic area on which respondents focused more than on other areas (both in the treatment and assessment) was the sensory area with 98 cases (79%) and the lowest of those was the educational area with 46 cases (37%).
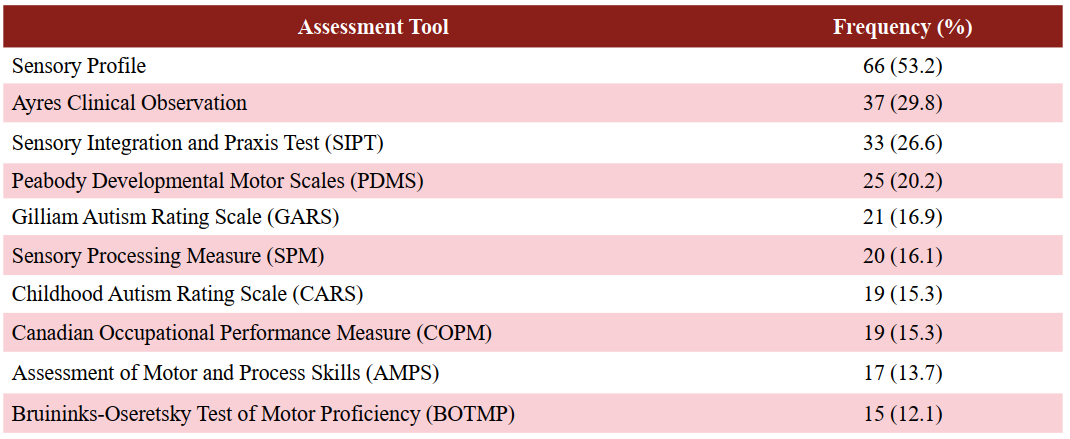
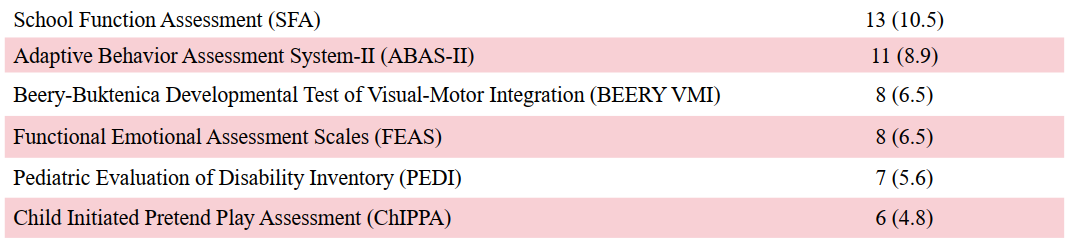
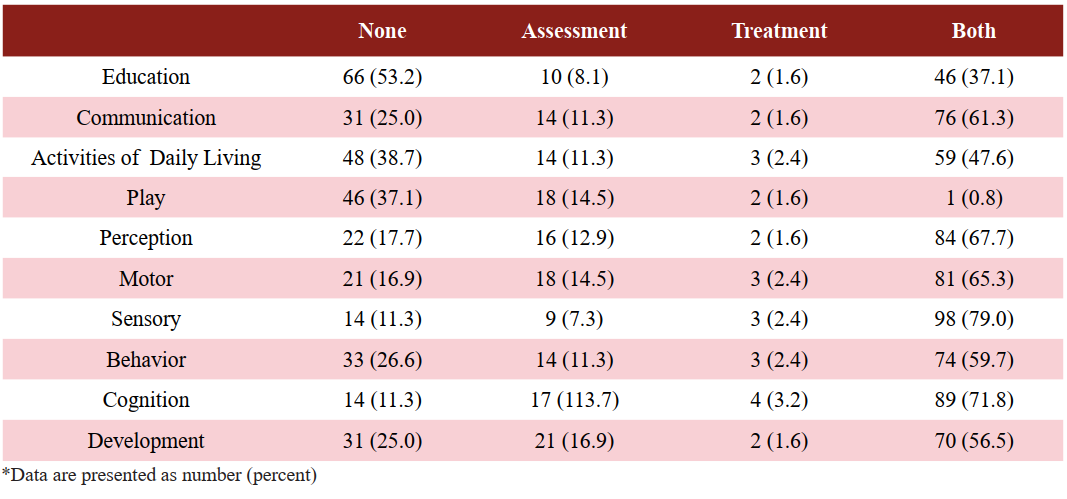
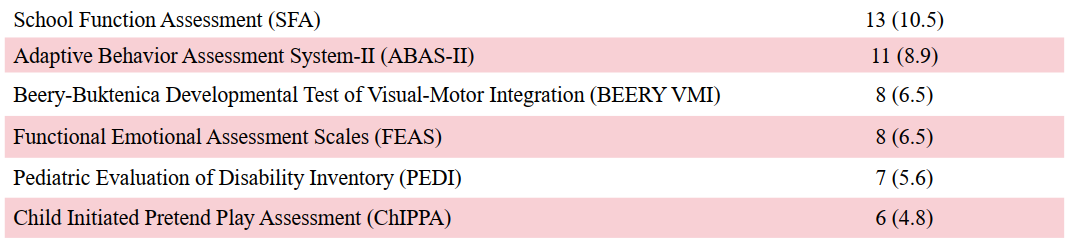
In terms of the type of assessments used by respondents, 103 respondents (83.1%) used observation of performance and 100 respondents (80.6%) used interviews. Each of the formal assessments is described in Table 3.
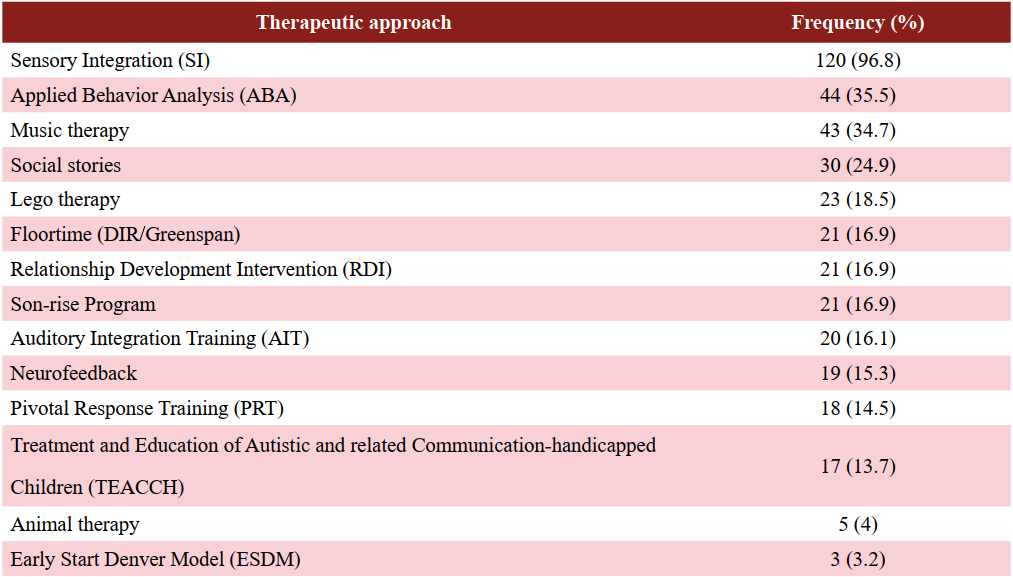
The approach used the most by therapists was the sensory integration approach (96.8%) whereas the least was the Denver approach (3.2%). Details are given in Table 4.
The review of the use of OT models showed that 44 therapists (35.5%) did not use any model in ASD. The remaining 64.5% of the therapists used some professional models, out of which the most common was the “cognitive orientation to occupational performance” model (COOP) (33.9%).
The Spearman correlation coefficient between work experience and perceived competency of the therapists was 0.132 (P=0.00), 0.154 between the level of education and perceived competency and 0.376 between the level of education and autism-specific experience was. It should be noted that only the last one was significant at 0.05 level. In addition, perceived competency was significantly correlated with providing consultation by the therapists for caregivers of people with ASD (r=0.256, P=0.004).
Only about half of the therapists (50.8%) perceived their competency to be above the average in treating ASD, and the rest perceived competency of the remaining therapists was moderate and below average. This level of competency was consistent with results of Ashburner et al. (2014) and was lower than that reported in the similar study conducted by Watling et al. (1999) that occupational therapists considered themselves in the treatment of ASD as 39% highly competent, 49% efficient, and 13% as expert. According to Cottrell (1990), low perceived competency might result in reduced willingness of the therapists to work with people with ASD.
Discontinuing OT could occur for various reasons. Attaining the therapeutic goals was the least frequent factor to stop OT. Family economic problems and their lack of cooperation to bring the child to the treatment sessions were the most important factors. These findings were in contrast to Watling et al.’s (1999) study, who reported the achievement of the treatment goals as the most important factor and the parents' request as the lowest factor in discontinuation of OT. According to Hock et al. (2015), the reason that the parents discontinued OT may be affected by perceptions on the burden of treatment on the family. The long process of OT, which is a process of non-medical treatment and non-insurance coverage in Iran, may be the reason for economic pressure on families. There are also several treatments for ASD. Based on the Bowker et al.’s (2011) study, families cannot usually follow several treatments at one time.
Books were the most scientific sources used by therapists. Only about half or less of the respondents had participated in workshops and retraining courses. However, more than half of them reported using the Internet. However, the web answers to questions are not guaranteed to be correct unless the therapist knows the strategies of evidence-based search. Kadar et al. (2012) found that a number of occupational therapists, working on ASD, did not go on with the science of the day and based on the OT philosophy, and instead used old approaches. Also, Myers (2017) suggested that the lack of use of scientific evidence in OT threatens the professional competency of these therapists. Undoubtedly, workshops and training courses on evidence-based search, advanced training and practical learning opportunities can play an important role in preparing the therapists to rehabilitate people with ASD and interact with other professionals.
As Tomchek and Koenig (2016) mentioned, findings of the present study showed that occupational therapists considered a wide range of therapeutic areas in assessing and rehabilitating individuals with ASD. The approaches that were used more than others in evaluation and treatment of ASD were sensory integration/processing, however, occupational areas such as education, activities of daily living and play had the least attention, respectively. In other studies consistent with the present study, such as Watling et al. (1999), Case-Smith and Miller (1999), Case-Smith and Arbesman (2008), Kadar et al. (2012), and Thompson-Hodgetts and Magill-Evans (2018), it was found that the greatest concern of the therapists in dealing with individuals with ASD was sensory issues. The fact is that few clinical trials have shown positive effects of the sensory integration approach on reducing the sensory-related behaviors (Pfeiffer et al., 2011) or social functioning and self-care (Schaaf et al., 2014) in children with ASD. The systematic review of Watling and Hauer (2015), Case-Smith et al. (2015), Weitlauf et al. (2017), and Ismael et al. (2018) showed a low or moderate effectiveness of sensory integration and sensory-based treatments on ASD even on the participation in activities of daily living that is the final goal of OT. When the therapists are trained and understand the impact of sensory approaches on experience, they are more likely to use these approaches (Thompson-Hodgetts & Magill-Evans, 2018).
In this study, the cognitive area after the sensory area was considered by therapists in the rehabilitation of ASD and, accordingly, the cognitive orientation to occupational performance (CO-OP) model was the most used model. Studies reported using the CO-OP model such as Rodger and Brandenburg (2009) and Rodger et al. (2008), who have shown the effect of this approach on children with ASD with no linguistic problems. Given the need for language abilities in the CO-OP model, most ASD clients of the OTs were likely to be high-functioning ASD.
The limitation of this study was that due to access to the required sample size, only the therapists who had experience in planning and implementing treatment for at least five ASD clients were selected. It was better to select occupational therapists who were in specialist centers for people with ASD and had experience in working with more clients with ASD. Examining therapists with a higher work experience with ASD could provide us with more accurate information. It is suggested that in future studies the therapists who are working in special centers for people with ASD be invited to participate in a similar study, so that more information will be available in details. Knowing the exact causes of discontinuing OT can help prevent it, therefore, research in this case is required. The present study identified the status of occupational therapy practice in using therapeutic approaches and models, but the process of clinical reasoning is a controversial issue that can determine why the therapists have used those approaches.
✅ Occupational therapists apply sensory and cognitive approaches in autism. Therapists should try to resolve the problems that exist for group therapy sessions. The use of sensory-based therapies and their impact on the participation in everyday life is controversial. Finding a solution to compensate for the high cost of occupational therapy for autism can make people more likely to receive occupational therapy services.
Full-Text: (6698 Views)
Background and Objectives: The progressive prevalence of Autism Spectrum Disorder and the high cost of its treatment suggest that health services should be purposefully provided to people with this disorder. Occupational therapists play a key role in the rehabilitation of autism. This study sought to monitor occupational therapy services provided to individuals with autism.
Materials and Methods: A survey about occupational therapy services for people with autism spectrum disorder was distributed to therapists. They completed a researcher-made questionnaire asking them about working conditions, knowledge sources, assessments, and interventions that have been used in autism. 225 questionnaires were distributed among occupational therapists who had the inclusion criteria.
Results: The number of the full-filled questionnaires was 124. The therapists worked more individual therapy (95%) than group sessions (23%). Household economic problems were reported as the most common cause of occupational therapy discontinuation. They focused more on sensory approaches and cognitive models. The education level of the therapist was significantly correlated with autism-specific experience (r=0.376, P=0.00). Of the respondents, 50.8% reported their competency to treat autism as higher than average. Perceived competency was significantly correlated with providing consultation by the therapists (r=0.256, P=0.004).
Conclusion: Occupational therapists apply sensory and cognitive approaches in autism. Therapists should try to resolve the problems that exist for group therapy sessions. The use of sensory-based therapies and their impact on the participation in everyday life is controversial. Finding a solution to compensate for the high cost of occupational therapy for autism can make people more likely to receive occupational therapy services.
Autism Spectrum Disorder (ASD) is a neurodevelopmental disorder characterized by sensory, perceptual, communicative, social, and play deficits (American Psychiatric Association, 2013). According to US statistics, the prevalence of ASD has risen from 1.25% in 2011-2013 to 24.2% in 2014 (Zablotsky, Black, Maenner et al., 2015). The prevalence of this disorder in Iran is lower than that in developed countries; the prevalence was 6.26 in 10,000 births in 5-year-old children in 2012 (Samadi, Mahmoodizadeh, & McConkey, 2012). ASD symptoms may range from very mild to very severe, covering all areas of development. The variety of symptoms has made it a complex disorder. Mental health professionals as a multidisciplinary teamwork can help people with ASD. Rehabilitation as a non-medical treatment can help these people along with medicine. Occupational therapists as rehabilitation practitioners, who are the members of the mental health team, are responsible of increasing individual’s participation in activities of daily living, education, work, play/leisure and social participation. These goals can be considered in relation to different settings such as clinics, home, school or community (Watling, Tomchek, & LaVesser, 2005).Materials and Methods: A survey about occupational therapy services for people with autism spectrum disorder was distributed to therapists. They completed a researcher-made questionnaire asking them about working conditions, knowledge sources, assessments, and interventions that have been used in autism. 225 questionnaires were distributed among occupational therapists who had the inclusion criteria.
Results: The number of the full-filled questionnaires was 124. The therapists worked more individual therapy (95%) than group sessions (23%). Household economic problems were reported as the most common cause of occupational therapy discontinuation. They focused more on sensory approaches and cognitive models. The education level of the therapist was significantly correlated with autism-specific experience (r=0.376, P=0.00). Of the respondents, 50.8% reported their competency to treat autism as higher than average. Perceived competency was significantly correlated with providing consultation by the therapists (r=0.256, P=0.004).
Conclusion: Occupational therapists apply sensory and cognitive approaches in autism. Therapists should try to resolve the problems that exist for group therapy sessions. The use of sensory-based therapies and their impact on the participation in everyday life is controversial. Finding a solution to compensate for the high cost of occupational therapy for autism can make people more likely to receive occupational therapy services.
Introduction
In order to achieve therapeutic goals in people with ASD, there are many therapeutic approaches in Occupational therapy (OT), including sensory, developmental, cognitive, social, intensive behavioral, and family-centered interventions (Case-Smith & Arbesman, 2008; Dammann, Althoff, Hope, & Ausderau, 2017; Miller-Kuhaneck, 2015). The studies of OT in ASD has different issues such as sensory integration (Pfeiffer, Koenig, Kinnealey et al., 2011), social skills training (Asher, 2014), somatosensory stimulation (Hodgetts & Hodgetts, 2007), floor-time (Dionne & Martini, 2011), family routines (Bagatell, Cram, Alvarez, & Loehle, 2014; Joosten & Safe, 2014), participation in everyday life (Ashburner, Rodger, Ziviani, & Hinder, 2015), play (Henning, Cordier, Wilkes‐Gillan, & Falkmer, 2016), use of technology (Wilkes‐Gillan & Joosten, 2016), and cognitive orientation to occupational performance (Rodger & Brandenburg, 2009). There are also OT studies that show the overall practice of therapists in ASD; for example Case-Smith and Arbesman (2008) reviewed OT interventions in ASD. Some studies like Watling et al. (1999) and Case-Smith and Miller (1999) in the USA, Kadar et al. (2012), and Ashburner et al. (2014) in Australia also examined the work conditions, interventions, and assessments used by Occupational therapists. The results of these studies indicate that the focus of assessments and interventions of American and Australian therapists is on sensory issues; they reported competency in the treatment of sensory problems in ASD, and even expressed the need for further education. In the review above, it is clear that the concentration of OT studies in ASD includes a variety of issues, but in practice, the focus is on sensory issues. Studies that reflect the practice of therapists can help them rethink their performance. No information is available on the practice of Iranian occupational therapists in ASD. A number of factors including priorities of clients, work setting (clinic, home, and school), available resources, evidence of effectiveness of a method, the therapist's experience and knowledge may interfere in selecting therapeutic interventions (Case-Smith & Arbesman, 2008). Training after graduation is necessary to achieve competency in some of the approaches mentioned above; so that it depends on certain conditions, such as motivation, possibility to attend in the training courses, needs of the workplace, and so on. These conditions lead therapists not to use all approaches in the treatment of ASD. In addition, assessment is a prerequisite of treatment. The assessment of people with ASD requires availability of the specific assessment tools and the skills to implement them. The above-mentioned factors clarify the necessity of evaluating Iranian occupational therapists’ practice in ASD.
Accordingly, the purpose of this study was to investigate the current practice of occupational therapy and answer some questions about occupational therapists’ practice in ASD, including the age range of people with ASD who receive OT services, causes of OT discontinuation, perceived competency and source of knowledge of therapists, interventions, assessments, and therapeutic models used in working with people with ASD.
Methods
This study was a cross-sectional research in 2018-2019. The study population included occupational therapists working in OT centers throughout Iran. Inclusion criteria were a history of at least three years of work experience in the field of mental disorders, as well as experience in treatment planning and implementation for at least five ASD diagnosed clients. The exclusion criteria were incomplete questionnaire. The participants were selected by convenient sampling from the OT Centers and conferences where therapists participated. They gave their consent to participate in the study. A total of 225 questionnaires were directly distributed to the therapists who met the inclusion criteria. Out of these, 143 questionnaires were returned. In the preliminary review, 19 invalid questionnaires were identified (Because these questionnaires were incomplete or they were found that the written information were not reliable). Finally, 124 questionnaires were valid for investigation. Out of these, 35 questionnaires were obtained from Tehran province and 89 were obtained from other provinces with a diverse distribution in the country.The assessment instrument was a researcher-made questionnaire. The items of the questionnaire were prepared according to the research questions and by reviewing the existing literature on OT in ASD. The face and content validity of the questionnaire was evaluated by 11 expert occupational therapists. After obtaining the expert opinions, 5 items were removed from the 20 initial items, which had a content validity ratio (CVR) of less than 0.62 (Lawshe, 1975). The content validity index (CVI) for each remaining item was greater than 0.79, with the mean of 90.66. Consequently, the final questionnaire had a good validity for the present study.
To describe the occupational therapists’ practice, central indices and dispersion were used. Chi-square, Pearson and Spearman correlation coefficients were used to describe and demonstrate quantitative and qualitative correlation between ground and independent variables with the OT practice.
Results
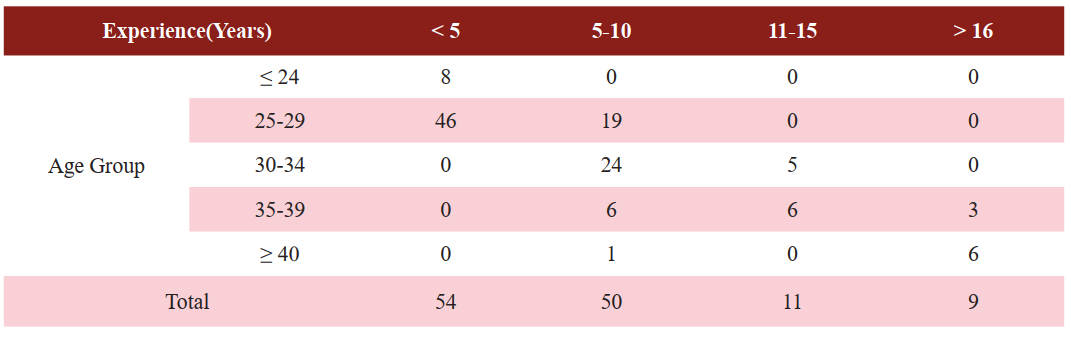
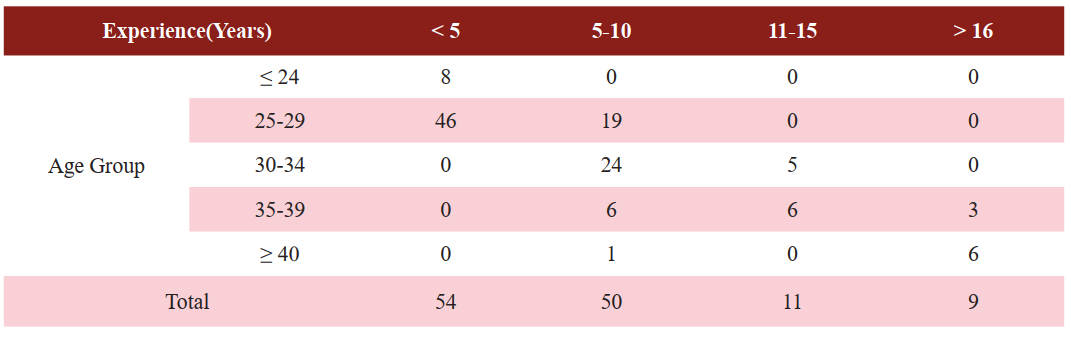
A total of 124 fully filled questionnaires were obtained. Of the occupational therapists who participated in this study, 88 (71%) were females and the rest (29%) were males. The mean age was 30±5.8, with a range of 23 to 52 years old. Out of these, 49.2% had bachelors, 42.7% masters, and 8.1% PhD degrees. The work experience of participants was 3-30 (mean=7). The Pearson correlation coefficient between the therapist's age and experience was very high (r=0.947) and significant. The frequency of experience in terms of age is represented in Table 1.Table1. The frequency of occupational therapists’ work experience in terms of age
The mean of minimum age of clients with ASD was 3.28 and the mean of maximum age was 10.22 years; so they were in childhood stage. The type of services provided by the therapists included 95% individual treatment, 73% assessment, 62% education, 52% consultation, and 23% group therapy.
The centers where the therapists worked with children with ASD included 103 outpatients, 28 home-visit, 26 exceptional schools, and 2 normal schools.
50.8% of the respondents reported that their competency to treat ASD is higher than average, and the rest reported moderate (45.2%), and lower than average (4%) competency.
The reasons for the discontinuation of OT were economic problems (79%), lack of cooperation of parents for going to OT (37.9%), lack of cooperation of the child with the therapist while doing therapeutic activities (14.5%), lack of expected change in the child (13.7%) and failure to reach the therapeutic goals (9.7%).
The source of knowledge for occupational therapists on ASD were classroom pamphlets, 53.2%, workshops, 51.6%, the internet, 62.9%, retraining courses, 31.5%, and books, 84.7%.
The OTs participating in this study were asked about the therapeutic areas that they were assessing and treating in children with ASD; the details are shown in Table 2.
Table2. The therapeutic areas were assessed and treated by occupational therapists in children with
autism spectrum disorder*
The therapeutic area on which respondents focused more than on other areas (both in the treatment and assessment) was the sensory area with 98 cases (79%) and the lowest of those was the educational area with 46 cases (37%).
In terms of the type of assessments used by respondents, 103 respondents (83.1%) used observation of performance and 100 respondents (80.6%) used interviews. Each of the formal assessments is described in Table 3.
Table3. Frequency of assessments were used by occupational therapists in autism spectrum disorder
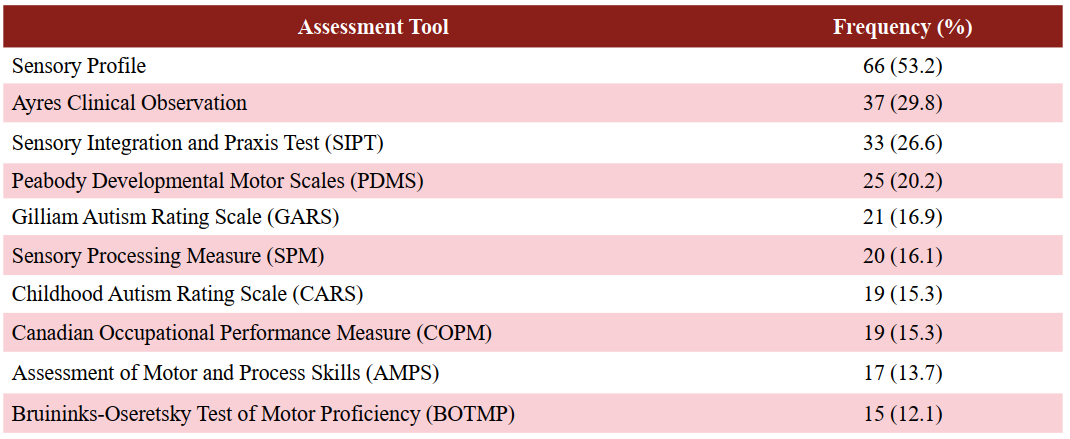
The approach used the most by therapists was the sensory integration approach (96.8%) whereas the least was the Denver approach (3.2%). Details are given in Table 4.
Table4. Treatment approaches used by occupational therapists in autism spectrum disorder
The review of the use of OT models showed that 44 therapists (35.5%) did not use any model in ASD. The remaining 64.5% of the therapists used some professional models, out of which the most common was the “cognitive orientation to occupational performance” model (COOP) (33.9%).
The Spearman correlation coefficient between work experience and perceived competency of the therapists was 0.132 (P=0.00), 0.154 between the level of education and perceived competency and 0.376 between the level of education and autism-specific experience was. It should be noted that only the last one was significant at 0.05 level. In addition, perceived competency was significantly correlated with providing consultation by the therapists for caregivers of people with ASD (r=0.256, P=0.004).
Discussion
The purpose of this study is to evaluate the practice of occupational therapists in rehabilitation of ASD. The results revealed that half of the therapists provided almost all of the services under study (assessment, counseling, family education, individual therapy, and group therapy) while others had experience in three or fewer of them. According to Watling et al. (2005), the therapists should provide a variety of services to individuals with ASD. Consistent with Watling et al. (1999), the most common type of service provided in OT was individual treatment, while group sessions were used least of all. As Epp (2008) stated, forming a group session is difficult especially in ASD in which the spectrum of the disorder varies from very mild to very severe, and the individuals who are selected to form a group must be similar in terms of the level of function. Consultation was the second service that was less used by respondents. Findings showed that the consultation had a relationship with the perceived competency of the therapist. Counseling is a person-to-person situation, which requires competency in scientific and communicative skills, so that the therapist should identify and analyze the existing and potential problems, find solutions to solve them, and prevent future problems (Jaffe, 2011).Only about half of the therapists (50.8%) perceived their competency to be above the average in treating ASD, and the rest perceived competency of the remaining therapists was moderate and below average. This level of competency was consistent with results of Ashburner et al. (2014) and was lower than that reported in the similar study conducted by Watling et al. (1999) that occupational therapists considered themselves in the treatment of ASD as 39% highly competent, 49% efficient, and 13% as expert. According to Cottrell (1990), low perceived competency might result in reduced willingness of the therapists to work with people with ASD.
Discontinuing OT could occur for various reasons. Attaining the therapeutic goals was the least frequent factor to stop OT. Family economic problems and their lack of cooperation to bring the child to the treatment sessions were the most important factors. These findings were in contrast to Watling et al.’s (1999) study, who reported the achievement of the treatment goals as the most important factor and the parents' request as the lowest factor in discontinuation of OT. According to Hock et al. (2015), the reason that the parents discontinued OT may be affected by perceptions on the burden of treatment on the family. The long process of OT, which is a process of non-medical treatment and non-insurance coverage in Iran, may be the reason for economic pressure on families. There are also several treatments for ASD. Based on the Bowker et al.’s (2011) study, families cannot usually follow several treatments at one time.
Books were the most scientific sources used by therapists. Only about half or less of the respondents had participated in workshops and retraining courses. However, more than half of them reported using the Internet. However, the web answers to questions are not guaranteed to be correct unless the therapist knows the strategies of evidence-based search. Kadar et al. (2012) found that a number of occupational therapists, working on ASD, did not go on with the science of the day and based on the OT philosophy, and instead used old approaches. Also, Myers (2017) suggested that the lack of use of scientific evidence in OT threatens the professional competency of these therapists. Undoubtedly, workshops and training courses on evidence-based search, advanced training and practical learning opportunities can play an important role in preparing the therapists to rehabilitate people with ASD and interact with other professionals.
As Tomchek and Koenig (2016) mentioned, findings of the present study showed that occupational therapists considered a wide range of therapeutic areas in assessing and rehabilitating individuals with ASD. The approaches that were used more than others in evaluation and treatment of ASD were sensory integration/processing, however, occupational areas such as education, activities of daily living and play had the least attention, respectively. In other studies consistent with the present study, such as Watling et al. (1999), Case-Smith and Miller (1999), Case-Smith and Arbesman (2008), Kadar et al. (2012), and Thompson-Hodgetts and Magill-Evans (2018), it was found that the greatest concern of the therapists in dealing with individuals with ASD was sensory issues. The fact is that few clinical trials have shown positive effects of the sensory integration approach on reducing the sensory-related behaviors (Pfeiffer et al., 2011) or social functioning and self-care (Schaaf et al., 2014) in children with ASD. The systematic review of Watling and Hauer (2015), Case-Smith et al. (2015), Weitlauf et al. (2017), and Ismael et al. (2018) showed a low or moderate effectiveness of sensory integration and sensory-based treatments on ASD even on the participation in activities of daily living that is the final goal of OT. When the therapists are trained and understand the impact of sensory approaches on experience, they are more likely to use these approaches (Thompson-Hodgetts & Magill-Evans, 2018).
In this study, the cognitive area after the sensory area was considered by therapists in the rehabilitation of ASD and, accordingly, the cognitive orientation to occupational performance (CO-OP) model was the most used model. Studies reported using the CO-OP model such as Rodger and Brandenburg (2009) and Rodger et al. (2008), who have shown the effect of this approach on children with ASD with no linguistic problems. Given the need for language abilities in the CO-OP model, most ASD clients of the OTs were likely to be high-functioning ASD.
The limitation of this study was that due to access to the required sample size, only the therapists who had experience in planning and implementing treatment for at least five ASD clients were selected. It was better to select occupational therapists who were in specialist centers for people with ASD and had experience in working with more clients with ASD. Examining therapists with a higher work experience with ASD could provide us with more accurate information. It is suggested that in future studies the therapists who are working in special centers for people with ASD be invited to participate in a similar study, so that more information will be available in details. Knowing the exact causes of discontinuing OT can help prevent it, therefore, research in this case is required. The present study identified the status of occupational therapy practice in using therapeutic approaches and models, but the process of clinical reasoning is a controversial issue that can determine why the therapists have used those approaches.
Conclusion
In rehabilitation of children with ASD, occupational therapists usually focus on individual treatment. However, it is also necessary to pay attention to counseling, group sessions and family therapy. Economic problems of Iranian families are one of the important factors in discontinuing OT for a child with ASD. The emphasis of occupational therapists in assessing and rehabilitating ASD is on the sensory area, whereas they should not forget their responsibility to facilitate participation of the individual with ASD in their life situations.Acknowledgements
This work was supported by a grant from Iran University of Medical Sciences (Grant number 96-04-32-32589). The authors gratefully acknowledge all occupational therapists who participated in this research, especially Yeghaneh Ghasemi and Zakieh Azarbash.Conflict of Interest
Authors declared no conflict of interest.
Subject:
Occupational Therapy
Received: 2019/04/16 | Accepted: 2019/05/29 | Published: 2020/01/12
Received: 2019/04/16 | Accepted: 2019/05/29 | Published: 2020/01/12
References
1. Ashburner, J., Rodger, S., Ziviani, J., & Hinder, E. (2015). Optimising Participation Of Children With Autism Spectrum Disorder Experiencing Sensory Challenges: A Clinical Reasoning Framework. Australian Occupational Therapy Journal, 62, 147.
2. Ashburner, J., Rodger, S., Ziviani, J., & Jones, J. (2014). Occupational therapy services for people with autism spectrum disorders: Current state of play, use of evidence and future learning priorities. Australian Occupational Therapy Journal, 61(2), 110-120. [DOI:10.1111/1440-1630.12083] [PMID]
3. Asher, A. (2014). Teaching social skills to people with autism Best practices in individualizing interventions. Canadian Journal of Occupational Therapy, 81(5), 329-329. [DOI:10.1177/0008417414559393]
4. American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (fifth ed.). Arlington VA: American Psychiatric Association. [DOI:10.1176/appi.books.9780890425596]
5. Bagatell, N. J., Cram, M., Alvarez, C. G., & Loehle, L. (2014). Routines of families with adolescents with autistic disorders: A comparison study: Étude comparative des routines des familles ayant des adolescents atteints de troubles autistiques. Canadian Journal of Occupational Therapy, 81(1), 62-67. [DOI:10.1177/0008417414520691] [PMID]
6. Bowker, A., D'Angelo, N. M., Hicks, R., & Wells, K. (2011). Treatments for autism: Parental choices and perceptions of change. Journal of Autism and Developmental Disorders, 41(10), 1373-1382. [DOI:10.1007/s10803-010-1164-y] [PMID]
7. Case-Smith, J., & Arbesman, M. (2008). Evidence-based review of interventions for autism used in or of relevance to occupational therapy. American Journal of Occupational Therapy, 62(4), 416-429. [DOI:10.5014/ajot.62.4.416] [PMID]
8. Case-Smith, J., & Miller, H. (1999). Occupational therapy with children with pervasive developmental disorders. American Journal of Occupational Therapy, 53(5), 506-513. [DOI:10.5014/ajot.53.5.506] [PMID]
9. Case-Smith, J., Weaver, L. L., & Fristad, M. A. (2015). A systematic review of sensory processing interventions for children with autism spectrum disorders. Autism, 19(2), 133-148. [DOI:10.1177/1362361313517762] [PMID]
10. Cottrell, R. F. (1990). Perceived competence among occupational therapists in mental health. American Journal of Occupational Therapy, 44(2), 118-124. [DOI:10.5014/ajot.44.2.118] [PMID]
11. Dammann, C., Althoff, C., Hope, S., & Ausderau, K. (2017). Parent-Mediated Interventions With Children With Autism Spectrum Disorder: A Systematic Review. American Journal of Occupational Therapy, 71(4_Supplement_1), 7111515226p1. [DOI:10.5014/ajot.2017.71S1-PO2175]
12. Dionne, M., & Martini, R. (2011). Floor time play with a child with autism: A single-subject study. Canadian Journal of Occupational Therapy, 78(3), 196-203. [DOI:10.2182/cjot.2011.78.3.8] [PMID]
13. Epp, K. M. (2008). Outcome-based evaluation of a social skills program using art therapy and group therapy for children on the autism spectrum. Children & Schools, 30(1), 27-36. [DOI:10.1093/cs/30.1.27]
14. Henning, B., Cordier, R., Wilkes‐Gillan, S., & Falkmer, T. (2016). A pilot play‐based intervention to improve the social play interactions of children with autism spectrum disorder and their typically developing playmates. Australian Occupational Therapy Journal, 63(4), 223-232. [DOI:10.1111/1440-1630.12285] [PMID]
15. Hock, R., Kinsman, A., & Ortaglia, A. (2015). Examining treatment adherence among parents of children with autism spectrum disorder. Disability and health journal, 8(3), 407-413. [DOI:10.1016/j.dhjo.2014.10.005] [PMID]
16. Hodgetts, S., & Hodgetts, W. (2007). Somatosensory stimulation interventions for children with autism: Literature review and clinical considerations. Canadian Journal of Occupational Therapy, 74(5), 393-400. [DOI:10.2182/cjot.07.013] [PMID]
17. Ismael, N., Lawson, L. M., & Hartwell, J. (2018). Relationship Between Sensory Processing and Participation in Daily Occupations for Children With Autism Spectrum Disorder: A Systematic Review of Studies That Used Dunn's Sensory Processing Framework. American Journal of Occupational Therapy, 72(3), 7203205030p7203205031-7203205030p7203205039. [DOI:10.5014/ajot.2018.024075] [PMID]
18. Jaffe, E. G., & Epstein, C. F. . (2011). Consultation: Collaborative interventions for change. In K. Jacobs & G. L. Mc-Cormack (Eds.), The occupational therapy manager (5th ed., pp. 521-545). Bethesda, MD: AOTA Press.
19. Joosten, A. V., & Safe, A. P. (2014). Management strategies of mothers of school‐age children with autism: Implications for practice. Australian Occupational Therapy Journal, 61(4), 249-258. [DOI:10.1111/1440-1630.12116] [PMID]
20. Kadar, M., McDonald, R., & Lentin, P. (2012). Evidence‐based practice in occupational therapy services for children with autism spectrum disorders in Victoria, Australia. Australian Occupational Therapy Journal, 59(4), 284-293. [DOI:10.1111/j.1440-1630.2012.01015.x] [PMID]
21. Lawshe, C. H. (1975). A quantitative approach to content validity. Personnel psychology, 28(4), 563-575. [DOI:10.1111/j.1744-6570.1975.tb01393.x]
22. Miller-Kuhaneck, H. (2015). Autism spectrum disorder. In J. Case-Smith & J. C. O'Brien (Eds.), Occupational therapy for children and adolescents (7th ed., pp. 766-792). Canada: Elsevier: Mosby.
23. Myers, C. (2017). Occupational Therapists' Use of Research and Evidence Sources Associated With an Online Competence Assessment. American Journal of Occupational Therapy, 71(4_Supplement_1). [DOI:10.5014/ajot.2017.71S1-PO5155]
24. Pfeiffer, B. A., Koenig, K., Kinnealey, M., Sheppard, M., & Henderson, L. (2011). Effectiveness of sensory integration interventions in children with autism spectrum disorders: A pilot study. American Journal of Occupational Therapy, 65(1), 76-85. [DOI:10.5014/ajot.2011.09205] [PMID]
25. Rodger, S., & Brandenburg, J. (2009). Cognitive Orientation to (daily) Occupational Performance (CO‐OP) with children with Asperger's syndrome who have motor‐based occupational performance goals. Australian Occupational Therapy Journal, 56(1), 41-50. [DOI:10.1111/j.1440-1630.2008.00739.x] [PMID]
26. Rodger, S., Ireland, S., & Vun, M. (2008). Can Cognitive Orientation to daily Occupational Performance (CO-OP) help children with Asperger's syndrome to master social and organisational goals? British Journal of Occupational Therapy, 71(1), 23-32. [DOI:10.1177/030802260807100105]
27. Samadi, S. A., Mahmoodizadeh, A., & McConkey, R. (2012). A national study of the prevalence of autism among five-year-old children in Iran. Autism, 16(1), 5-14. [DOI:10.1177/1362361311407091] [PMID]
28. Schaaf, R. C., Benevides, T., Mailloux, Z., Faller, P., Hunt, J., van Hooydonk, E., . . . Kelly, D. (2014). An intervention for sensory difficulties in children with autism: A randomized trial. Journal of Autism and Developmental Disorders, 44(7), 1493-1506. [DOI:10.1007/s10803-014-2111-0]
29. Thompson-Hodgetts, S., & Magill-Evans, J. (2018). Sensory-Based Approaches in Intervention for Children With Autism Spectrum Disorder: Influences on Occupational Therapists' Recommendations and Perceived Benefits. American Journal of Occupational Therapy, 72(3), 7203205020p7203205021-7203205020p7203205028. [DOI:10.5014/ajot.2018.024729] [PMID]
30. Tomchek, S., & Koenig, K. (2016). Occupational therapy practice guidelines for children and adolescents with Autism Spectrum Disorders. Bethesda, MD: American Occupational Therapy Association, Inc. [DOI:10.5014/ajot.2017.711003] [PMID]
31. Watling, R., Deitz, J., Kanny, E. M., & McLaughlin, F. (1999). Current practice of occupational therapy for children with autism. American Journal of Occupational Therapy, 53(5), 498-505. [DOI:10.5014/ajot.53.5.498] [PMID]
32. Watling, R., & Hauer, S. (2015). Effectiveness of Ayres Sensory Integration® and sensory-based interventions for people with autism spectrum disorder: A systematic review. American Journal of Occupational Therapy, 69(5), 6905180030p6905180031-6905180030p6905180012. [DOI:10.5014/ajot.2015.018051] [PMID]
33. Watling, R., Tomchek, S., & LaVesser, P. (2005). The scope of occupational therapy services for individuals with autism spectrum disorders across the lifespan. The American journal of occupational therapy: official publication of the American Occupational Therapy Association, 59(6), 680-683. [DOI:10.5014/ajot.59.6.680] [PMID]
34. Weitlauf, A. S., Sathe, N., McPheeters, M. L., & Warren, Z. E. (2017). Interventions targeting sensory challenges in autism spectrum disorder: a systematic review. Pediatrics, 139(6), e20170347. [DOI:10.1542/peds.2017-0347] [PMID]
35. Wilkes‐Gillan, S., & Joosten, A. (2016). Technology‐based interventions were found to have evidence of effectiveness on a range of outcomes, including social problem solving and facial and emotional processing skills for individuals with autism spectrum disorders. Australian Occupational Therapy Journal, 63(2), 135-136. [DOI:10.1111/1440-1630.12274] [PMID]
36. Zablotsky, B., Black, L. I., Maenner, M. J., Schieve, L. A., & Blumberg, S. J. (2015). Estimated prevalence of autism and other developmental disabilities following questionnaire changes in the 2014 National Health Interview Survey. National health statistics report, 1-20.






