Volume 8, Issue 1 (Continuously Updated 2025)
Func Disabil J 2025, 8(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Haddad M, Nokhodchi N. Comparing the Effects of Hydrotherapy and Facilitatory Kinesio Taping on proprioception, Strength and Fall Risk in Women with Diabetic Neuropathy. Func Disabil J 2025; 8 (1)
URL: http://fdj.iums.ac.ir/article-1-335-en.html
URL: http://fdj.iums.ac.ir/article-1-335-en.html
1- Department of Sports Sciences, Faculty of Human Sciences, University of Bojnord, Bojnord, Iran.
2- Department of Sports Sciences, Faculty of Human Sciences, University of Bojnord, Bojnord, Iran. ,nokhodchi@ub.ac.ir
2- Department of Sports Sciences, Faculty of Human Sciences, University of Bojnord, Bojnord, Iran. ,
Keywords: Hydrotherapy, Kinesio taping (KT), Proprioception, Accidental falls, Diabetic neuropathies
Full-Text [PDF 834 kb]
(87 Downloads)
| Abstract (HTML) (249 Views)
Full-Text: (35 Views)
Introduction
Diabetes is one of the most common metabolic disorders worldwide, and its prevalence among adults has been increasing over recent decades. In 2013, approximately 382 million people had diabetes, and this number is expected to rise to 592 million by 2035. The disease is categorized into two major types: Type I (5-8%) and type II (the majority of patients) [1]. Type II diabetes, primarily affected by genetic predisposition and unhealthy lifestyle factors, is marked by insufficient or ineffective levels of insulin secretion [2].
A common long-term complication of diabetes is diabetic neuropathy, which is associated with severe pain, sensory loss, and a higher risk of ulcers and amputations [3]. This condition is categorized into autonomic neuropathy and sensorimotor neuropathy. Autonomic neuropathy impairs the function of internal structures, such as the cardiovascular, digestive, urinary, and reproductive systems, whereas sensorimotor neuropathy primarily affects the neuromuscular system. The three most frequent subtypes of sensorimotor diabetic neuropathy include peripheral polyneuropathy, focal neuropathy, and diabetic amyotrophy [4]. Peripheral polyneuropathy is the most prevalent type of diabetic neuropathy, accounting for at least 50% of patients with a 25-year history of type II diabetes [5]. Diabetic peripheral neuropathy (DPN) results in impaired blood flow and progressive degeneration of nerve fibers [4]. It primarily affects the lower extremities, with symptoms such as distal limb pain and numbness, which can increase the risk of ulceration [6]. Peripheral neuropathy is associated with both direct and indirect complications, including impaired proprioception and balance, decreased muscle strength, and increased fall risk [7].
In peripheral neuropathy, degeneration of sensory afferents leads to postural instability and defective proprioception in the lower extremities [8]. Proprioception refers to the afferent information from the body’s internal peripheral regions, provided by the mechanical receptors in the joints, skin, and muscles. Impairments in proprioception disrupt feedback mechanisms and affect motor control [9]. Reduced proprioceptive ability lowers postural stability in patients with DPN, elevating the risk of accidental falls, particularly in elderly patients [10]. As a result, the progression of neuropathy and proprioceptive decline can lower functional balance and contribute to movement difficulties in daily activities [11].
Muscle strength is another crucial contributor to balance, influenced by joint angle, muscle group, type of contraction, and contraction speed [12]. Studies have suggested that in diabetic patients, the strength of the ankle flexor and extensor muscles decreases by 17% and 14%, respectively [13]. Reduced muscle strength in patients with type I and type II diabetes has been reported as a late complication of DPN, often presenting alongside motor nerve involvement [14]. Therapeutic interventions for DPN typically include antidepressant, anti-inflammatory, and anticonvulsant drugs. Nevertheless, due to their potential side effects, some non-pharmacological interventions have been explored to improve DPN symptoms, including acupuncture, laser therapy, phototherapy, thermotherapy, kinesiotherapy, and hydrotherapy [15].
In recent years, hydrotherapy has gained considerable attention as a complementary treatment for physical and motor impairments [16]. Hydrotherapy exercises provide physiological benefits, especially for patients with sensorimotor disorders [17]. Accordingly, aquatic exercises have long been used as a common therapeutic approach to reduce the effects of peripheral neuropathy on the sensorimotor functions of individuals with diabetes.
Kinesio tape is an elastic therapeutic tape commonly used in rehabilitation settings and by athletes to alleviate muscle spasms and pain, enhance muscle contraction, facilitate or inhibit muscle activity, increase range of motion, and improve blood and lymphatic circulation as well as proprioception. Kinesio tapes are designed to support soft tissues without restricting their function [18].
Research findings suggest that KT can improve proprioception and joint stability by inhibiting overactive muscles and facilitating weak ones, reducing pain, decreasing pressure on irritated nerve tissues, and altering the recruitment pattern of muscle fibers depending on the direction and degree of stretch [19]. Generally, kinesio tapes are assumed to facilitate a muscle when applied from its origin to its insertion and inhibit it when applied in the opposite direction [20].
The rising popularity of taping techniques among athletes, coupled with their reported benefits in enhancing athletic performance, has generated significant interest in applying kinesio tapes to improve physical abilities and quality of life in patients with various sensorimotor disorders, including neuropathy. In this regard, Thakur et al. highlighted the beneficial effects of KT on sensorimotor indices among patients with diabetic neuropathy [21]. Considering the importance of facilitating lower limb muscle activity for improved functioning in individuals with diabetic neuropathy, this study aimed to achieve two objectives: (1) to examine the effect of facilitatory KT on sensorimotor indices among patients with DPN and (2) to compare this approach with hydrotherapy, a common treatment recommended for alleviating the neuropathic symptoms in patients with DPN.
Materials and Methods
This research employed a double-group pre-test-post-test design.
Study participants
The study population comprised women aged 40-60 years with DPN residing in Ferdows, South Khorasan Province, Iran. A convenience sample of 20 eligible women with DPN was recruited from the South Khorasan Diabetes Association (Ferdows branch).
The sample size encompassed the entire statistical population due to the limited number of women with DPN within the specified age range and region. The inclusion criteria for the study were a confirmed diagnosis of type II diabetes for at least five years by a medical specialist, current use of medications (metformin 500 mg twice daily with meals and glibenclamide 5–10 mg in the morning in a fasted state), a confirmed diagnosis of diabetic neuropathy based on clinical and laboratory diagnostic criteria, ability to complete balance assessments using the Michigan questionnaire with a minimum score of 7, functional independence in daily activities, no fear of water, previous pool experience within the last three years, ability to walk in water, and absence of medical contraindications.
Participants were excluded if they had foot ulcers, orthopedic problems or surgeries affecting walking, neurological complications other than diabetic neuropathy, peripheral vascular disease, central nervous system disorders (e.g. dementia, Parkinson disease, or multiple sclerosis), musculoskeletal deformities of the lower extremities, uncontrolled cardiovascular or respiratory conditions, uncorrected visual acuity worse than 20/70, history of dizziness, uncontrolled hypertension, resting tachycardia or arrhythmia, or an allergy to tape [21, 22].
An orientation session was held to familiarize all participants with the research and measurement procedures. Participants were then randomly assigned to hydrotherapy or KT groups using a simple randomization method, achieved through drawing numbered envelopes.
Exercise protocol
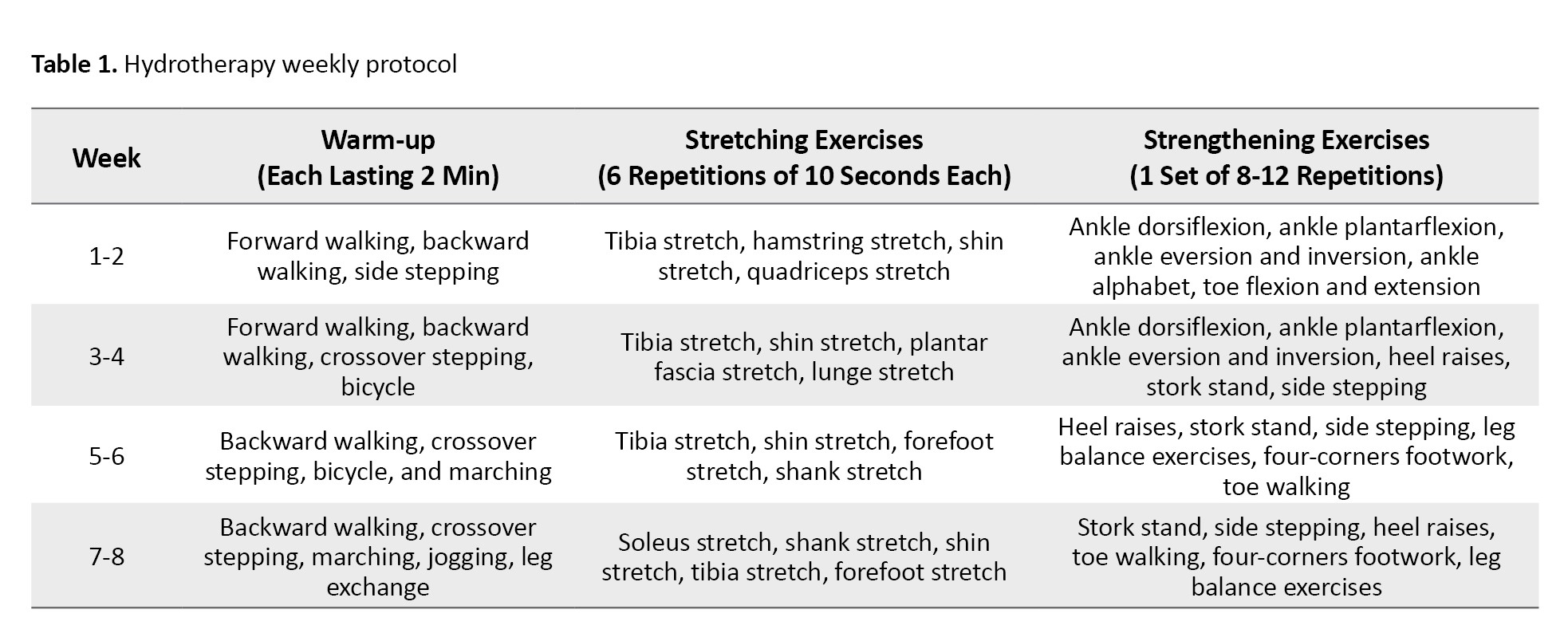
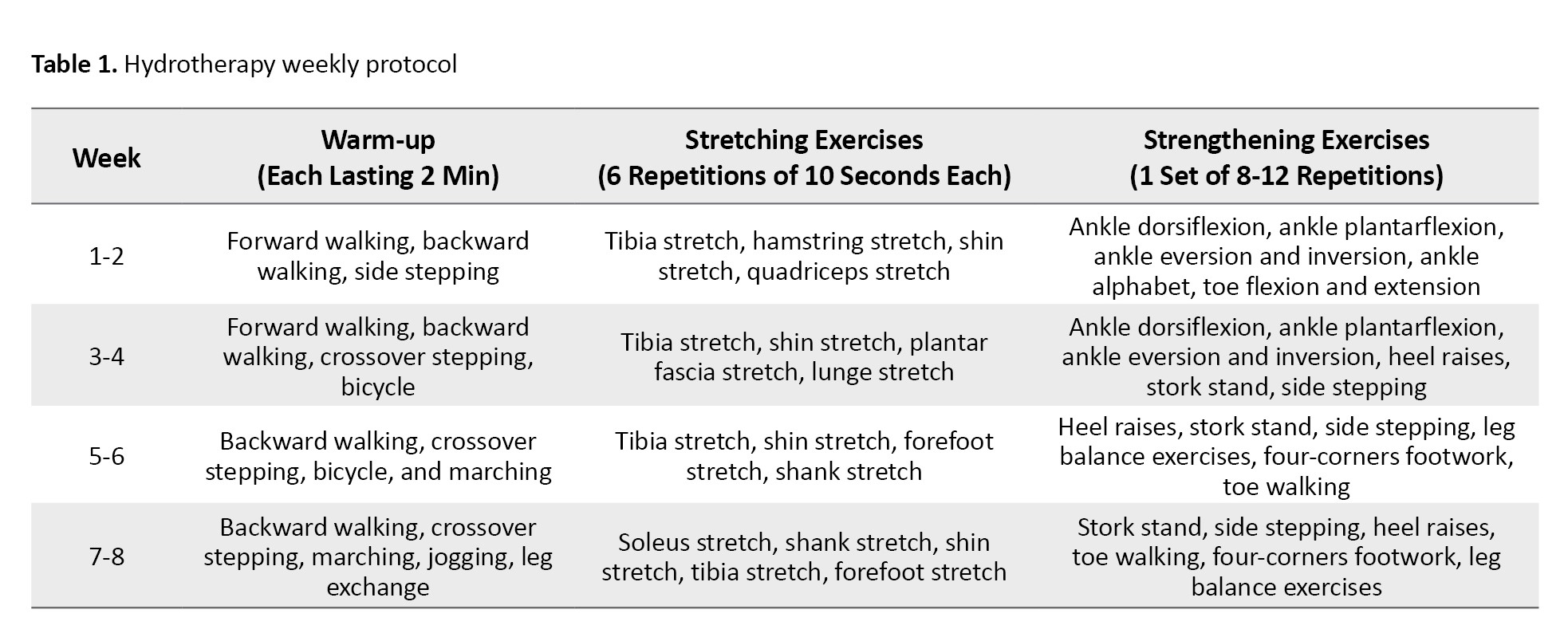
The hydrotherapy group participated in an 8-week training protocol consisting of three water-based exercise sessions per week, including warm-up, stretching, and strengthening exercises (Table 1) [16].
Kinesio taping
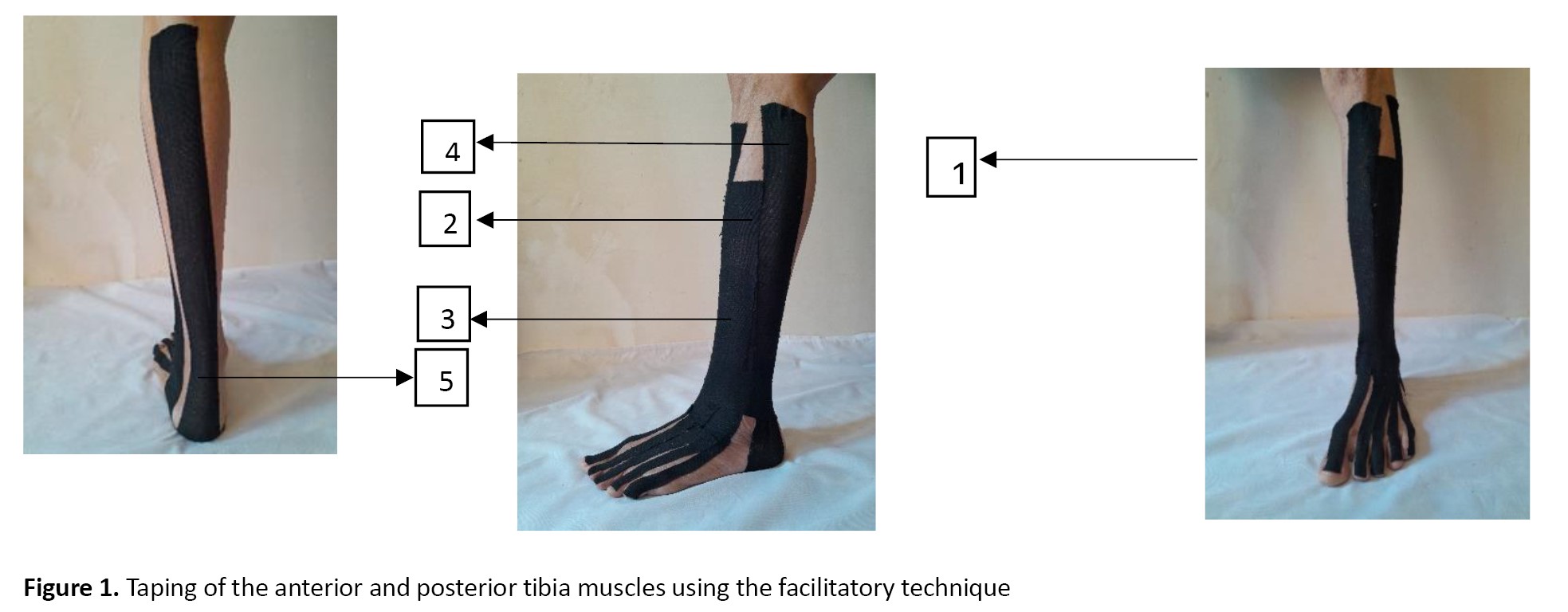
The kinesio tape used in this study was Kindmax, a 5-cm-wide tape manufactured by Shanghai Sport Product, China. The tape was applied to the tibialis anterior, extensor digitorum longus, extensor hallucis longus, peroneus longus, and gastrocnemius muscles for 24 hours a day over 8 weeks. It was replaced every five days (Figure 1). The tape was stretched to approximately 50% of its original length and applied from the muscle’s origin to its insertion [19].
1) Tibialis anterior: Participants lay supine on a treatment table while kinesio tapes were applied to their tibialis anterior muscles. The tape was anchored at the muscle’s origin (lateral condyle) and proximal anterolateral tibia. While the participants performed plantarflexion and eversion, the tape was tightened and secured to the muscle’s insertion point (lateral cuneiform bone surface).
2) Extensor digitorum longus: An inverted Y-shaped tape was applied, anchored at the muscle’s origin (lateral tibial condyle, distal three-quarters of medial fibula). Participants were then directed to dorsiflex the foot and extend the lateral four toes as the tape was secured from the metatarsophalangeal joints to the middle and distal phalanges of the lateral four toes.
3) Extensor hallucis longus: An I-shaped tape was applied to this muscle from the muscle’s origin in the mid-anterior surface of the ulna to the posterior aspect of the thumb’s distal phalanx.
4) Peroneus longus: The participant lay supine when the long fibular muscle was taped. The tape was secured at the proximal and lateral fibula, applied along the entire lateral surface of the leg, passed behind the lateral malleolus, and secured at the mid-lateral foot.
5) Gastrocnemius: The knee was fully extended to apply the tape on the gastrocnemius. The tape was anchored from the origin (posterior surface of the medial and lateral distal femoral condyles) to the posterior surface of the calcaneus.
Ankle joint position sense
The ankle joint position sense was evaluated using the active repositioning test at target angles of 10° and 20° for dorsiflexion and plantarflexion. A Biometrics Ltd. electrogoniometer (accuracy ±0.1°) was used for the measurements. The test was conducted separately for each leg while participants sat on a chair with their legs hanging freely. Each participant leaned against the backrest at a 90° angle. The researcher moved the ankle to the target angle at a steady rate of nearly 6° per second, maintained it for 5 seconds, and then slowly returned the limb to the starting position. Subsequently, participants were instructed to reproduce the same angle with their eyes closed. The difference between the reproduced and target angles was measured by an electrogoniometer. Each participant was assessed three times for each leg in both dorsiflexion and plantarflexion conditions, and the average of the three attempts for both legs was calculated as their score [23].
Strength
A Siemens Siwarex WL 250 model 7MH5105 load cell (Germany), with a 500 kg weight capacity, was employed in this study to measure the maximum strength of the anterior and posterior leg muscles. Participants were seated with their knees straight and their ankles positioned at a 90° angle relative to their legs. The equipment was adjusted to prevent any undesirable movement. Each participant performed three attempts for each test and each leg and was verbally encouraged to achieve maximum voluntary contraction. A 60-second rest period was provided between each attempt. The mean maximum strength from all three attempts across both legs was recorded as the dorsiflexion and plantarflexion muscle strength scores [24].
Balance
The Berg balance scale was employed to assess balance. This test is a reliable, functional scale for evaluating balance disorders in the elderly population. The scale consists of 14 items that assess both static and dynamic balance. The items are scored on a 5-point Likert scale (0-4) based on the quality or duration of task performance. The maximum scale score is 56, and a score below 45 indicates a high risk of falling [22]. This scale includes the following items:
1) standing up unsupported; 2) sitting unsupported; 3) standing up from a sitting position; 4) sitting down from a standing position; 5) standing with closed eyes; 6) transferring from one chair to another; 7) standing with feet together; 8) picking up an object from the floor while standing; 9) reaching forward with outstretched arms; 10) turning around in a complete rotation 11) turning right and left to look back; 12) placing the feet alternately on a stool; 13) standing on one leg, and 14) standing independently with one foot in front of the other [25].
International fall efficiency scale
This scale consists of 16 items rated on a 4-point Likert scale ranging from “not at all worried” to “completely worried” (scores 1 to 4). Higher scores indicate a greater fear of falling. The scale demonstrates strong reliability and validity, with a Pearson correlation coefficient of 0.70 and an intraclass correlation coefficient of 0.98 [26].
Statistical analysis
The collected data were analyzed using the SPSS software, version 16. The significance level was set at P<0.05. First, the normality of the data was verified using the Shapiro-Wilk test. Independent samples t-tests were conducted to compare baseline mean differences between groups, while paired samples t-tests were employed to assess within-group changes. Analysis of covariance (ANCOVA) was used to compare between-group differences. Results are presented as Mean±SD.
Results
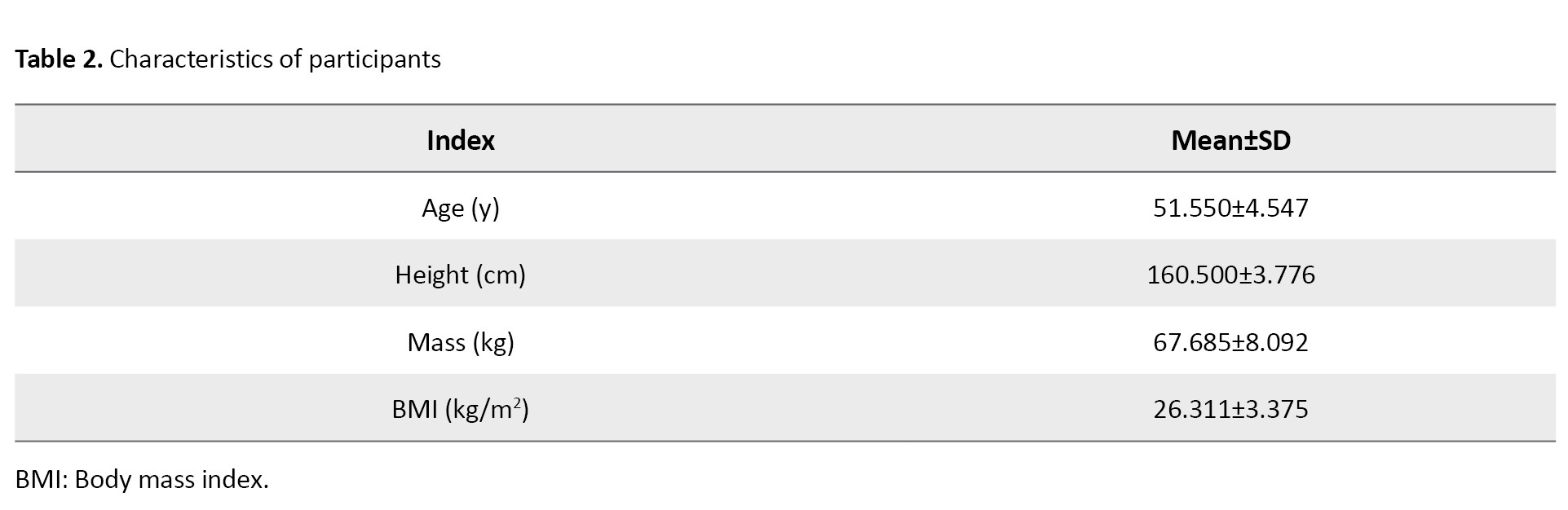
A total of 20 participants with DPN completed the study. Table 2 presents the demographic characteristics of the participants.
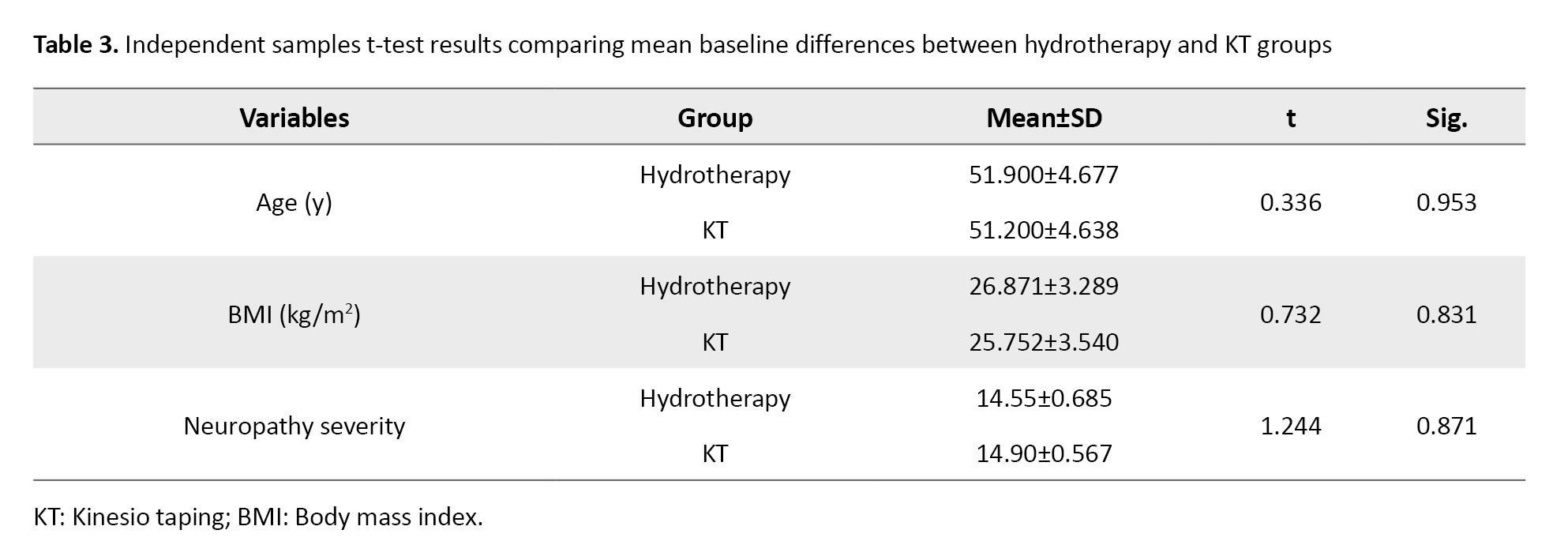
Based on the independent-samples t-test results (Table 3), no significant baseline differences were observed between the hydrotherapy and KT groups in terms of age, body mass index (BMI), and neuropathy severity (P>0.05).
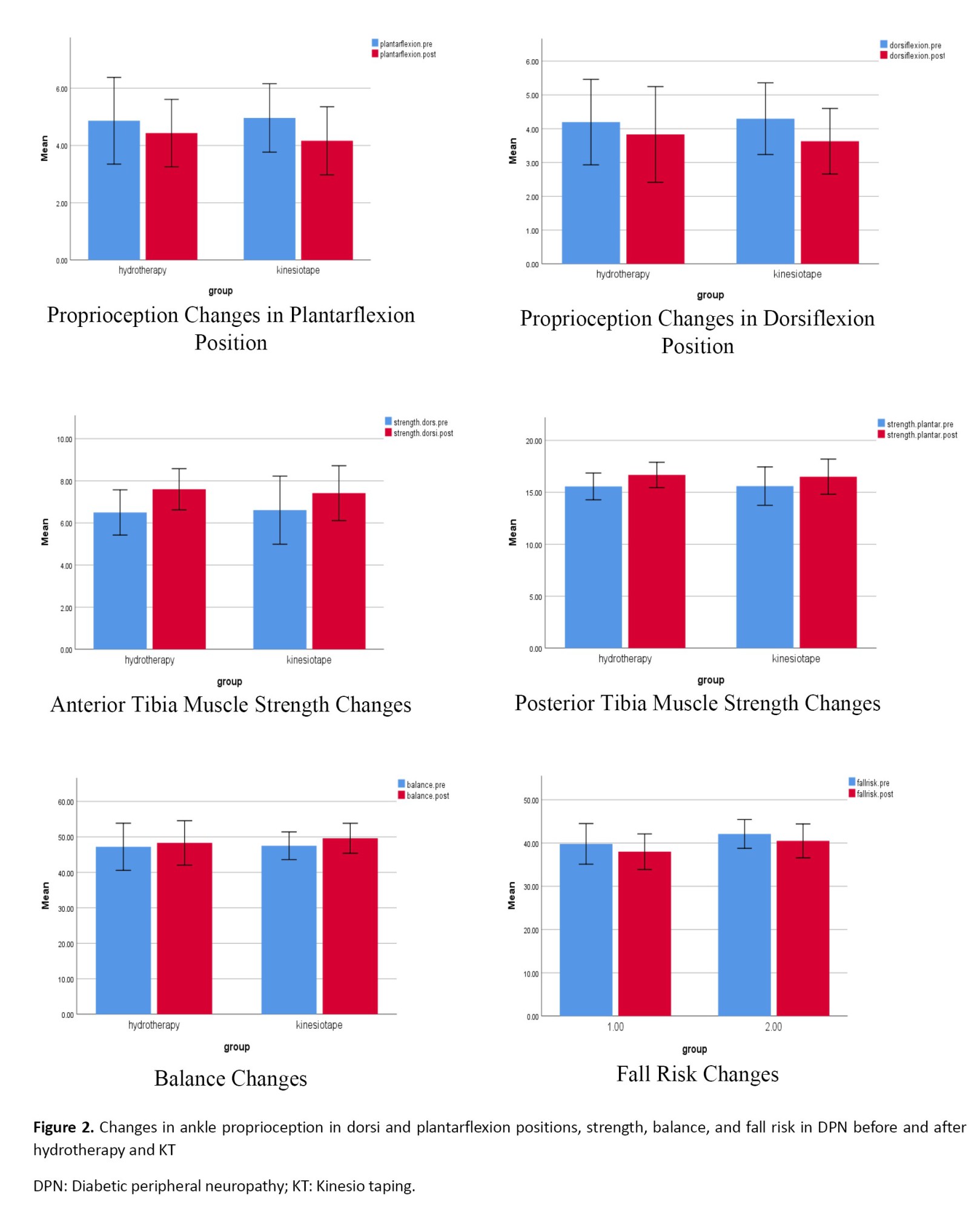
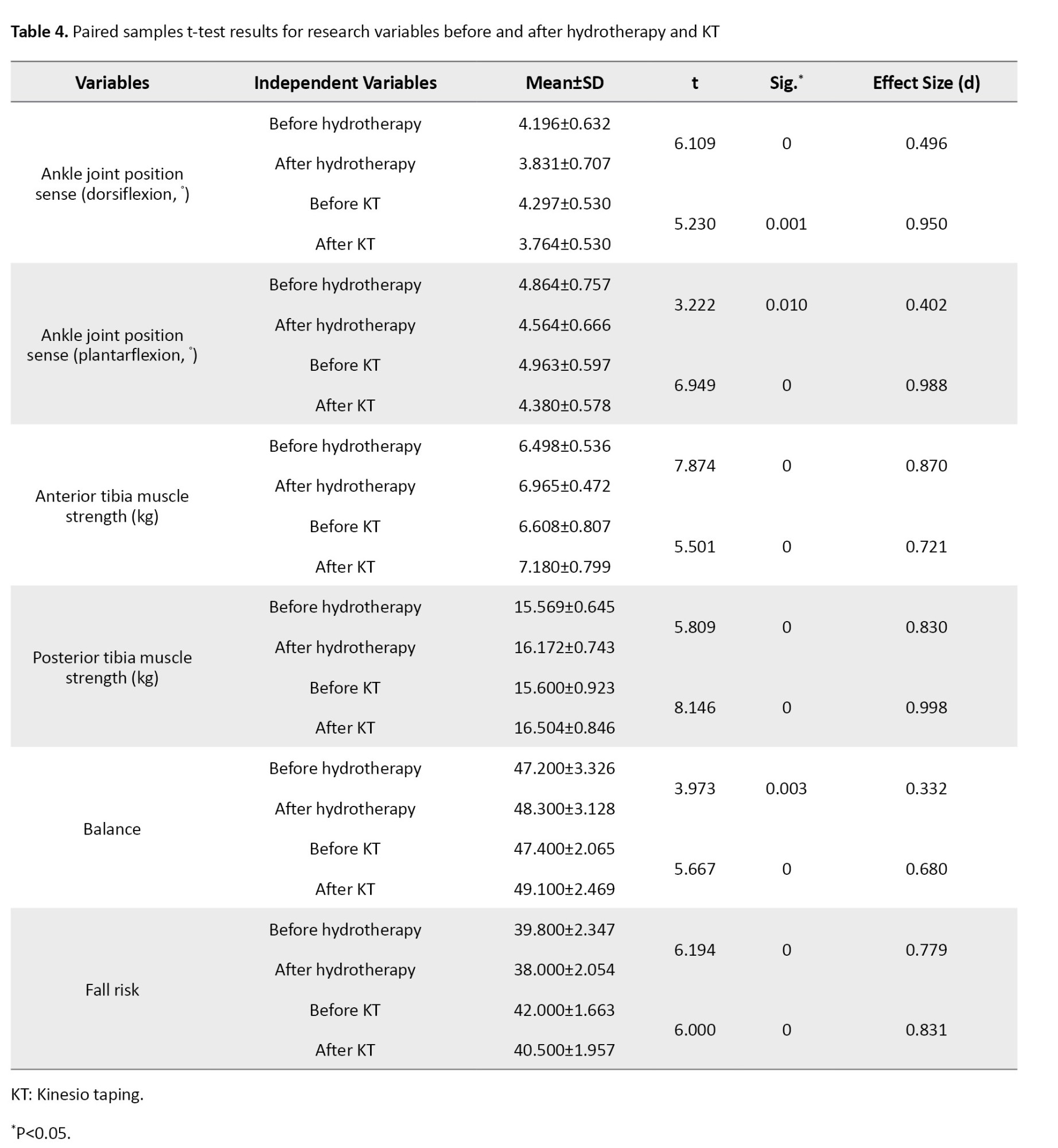
Based on the paired-samples t-test results (Table 4), eight weeks of hydrotherapy exercises and the application of facilitatory KT led to significant improvements in ankle joint position sense (both dorsiflexion and plantarflexion), strength, balance, and fall risk in women with DPN (P<0.05).
Moreover, the ANCOVA results (Table 5 and Figure 2) indicated a significant difference between the effects of facilitatory KT and hydrotherapy on ankle joint position sense in both dorsiflexion and plantarflexion positions of the ankle joint, as well as on balance (P<0.05).
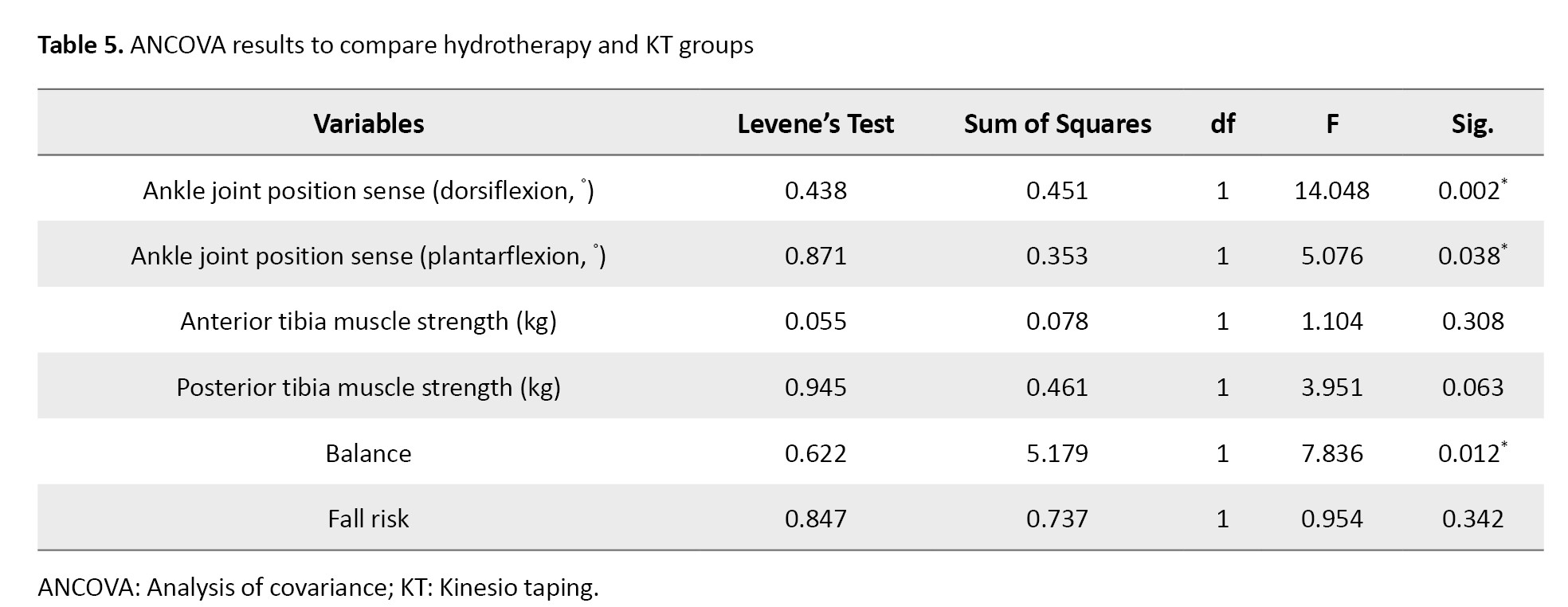
However, no significant differences were observed between the effects of KT and hydrotherapy on muscle strength and fall risk.
Discussion
This study sought to investigate and compare the effects of hydrotherapy exercises and facilitatory KT on ankle joint position sense, strength, balance, and fall risk in women with DPN. The results revealed that an 8-week intervention involving either hydrotherapy or the application of facilitatory KT improved ankle joint position sense in women with DPN. However, KT produced a greater effect size than hydrotherapy.
Relying on joint and muscle receptors, joint position sense plays a crucial role in the perception of limb and joint position. Known as the primary receptors involved in joint position sense, muscle spindles are affected by changes in muscle length as well as inputs from skin and joint receptors [27]. According to previous research, joint receptors complement muscle receptors in the joint position sense, particularly during joint stretching or compression [28]. The majority of previous research has confirmed the effectiveness of sports exercises in improving proprioception and joint position sense in patients with DPN [29]. Likewise, hydrotherapy exercises have been shown to improve proprioception and position sense in individuals with DPN [16]. The results of the current study are consistent with these findings.
It is necessary to investigate potential central mechanisms to determine the reasons behind the improvement in joint position sense following participation in hydrotherapy exercises. In this regard, increased attention may be a potential mechanism for improving exercise-induced proprioception. The hydrotherapy exercises used in the current study appear to have increased participants’ attention to proprioceptive cues at both automatic and conscious levels, paving the way for participants to improve their position sense. Furthermore, studies have demonstrated that training increases the output of muscle spindles, which may improve movement accuracy by modulating muscle tonicity [30].
Moreover, the current study’s findings revealed the beneficial effects of facilitatory KT on joint position sense, which aligns with the results reported by Thakur et al. KT exerts pressure, heat, and cutaneous stimulation that activate joint receptors and improve ankle joint position sense in women with DPN. Although the precise mechanism underlying KT’s facilitative effect is not fully understood, researchers have proposed two possible hypotheses. The first highlights increased lymph and blood flow as a result of skin elevation and the subsequent expansion of the space between the skin and underlying muscles in the KT area. The second hypothesis argues that KT stimulates cutaneous mechanoreceptors and activates central nervous system regulatory mechanisms, thereby enhancing muscle activation through tension and pressure applied to the skin beneath the tape. In this regard, recent research has demonstrated the positive impact of facilitative KT on enhancing muscular electrical activity [31, 32].
Furthermore, the current study found that KT exerted greater beneficial effects on position sense and a larger effect size than hydrotherapy. The angles used to investigate joint position sense in this study were in the mid-range of motion (10° dorsiflexion and 20° plantarflexion). At these angles, the muscle spindle plays a more significant role than joint receptors. Therefore, muscle activity facilitation by a KT could increase muscle spindle stimulation through tensile forces, resulting in a greater accuracy in position sense.
The current study also found that 8 weeks of hydrotherapy exercises or KT improved the strength of ankle flexor and extensor muscles in women with DPN, with no significant difference between the two interventions. Previous studies have demonstrated that resistance training can enhance muscle strength in individuals with DPN [33]. The findings of the current study similarly indicate that aquatic exercises can enhance lower extremity muscle strength in women with DPN.
The possible reasons behind improved muscle strength following hydrotherapy exercises can include neural adaptations such as reduced resistance in nerve pathways to impulse transmission, cortical sensorimotor reorganization, reduced inhibitory nerve reflexes, use of more efficient motor units, increased activation of the nervous system, enhanced efficiency and strength of synaptic communication, and facilitated transfer of data from every sense [34]. Moreover, the results of the present study revealed that the use of facilitatory KT increased the strength of the ankle dorsiflexor and plantarflexor muscles. Earlier studies, such as those by Ahmed et al, have also reported the positive effects of resistance training combined with KT on muscular strength in individuals with DPN [19]. KT widens the interstitial space between the skin and soft tissues, resulting in increased local blood flow, reduced local edema, and stimulation of the skin, muscle, and fascia. Consequently, this provides more effective sensory input to the central nervous system, resulting in reduced muscle inhibition and stronger muscle contractions. Given that the facilitation technique was used for taping, it was expected to increase strength by stimulating muscle spindles, as confirmed by the current study findings.
This study further indicated that 8 weeks of hydrotherapy or KT improved balance and reduced the risk of falls in women with DPN. Additionally, the findings revealed that the facilitatory application of kinesio tape had a greater effect on improving balance than hydrotherapy. However, there were no significant differences between the two groups in terms of fall risk reduction. In this regard, previous studies by Sakinepoor et al. and Shourabi et al. have demonstrated that both aquatic exercise and resistance training improve balance in individuals with DPN [16, 35]. They have also reported that in-water therapeutic exercises exert a greater effect on balance than resistance training [35]. In line with these findings, the current study suggests that increased joint position sense, a crucial component of balance control, may be a possible explanation for the observed improvement in balance. To maintain proper balance, the motor control system must continuously monitor changes in joint position [36]. The results of this study indicate that joint position sense improved significantly after hydrotherapy and kinesio tape application. As a result, it is reasonable to conclude that an improvement in joint position sense is one of the most likely causes of improved balance in women with DPN. Another important factor in maintaining balance is strength, which helps to prevent postural fluctuations. Indeed, a decline in muscle strength is considered a health concern that can compromise balance [34]. This study found that hydrotherapy exercises and KT increased strength in individuals with DPN. Therefore, increased strength could be the second possible cause of improved balance in women with DPN.
As muscle weakness, impaired balance, and motor control problems all contribute to falls, hydrotherapy can be an effective strategy to improve balance and prevent falls. This is because increasing muscle strength and balance leads to better motor control and a lower fear of falling. Regarding the positive effects of KT on improving balance and lowering fall risk in women with DPN, it can be argued that the enhanced balance following the use of kinesio tapes can be attributed to their effects on improving ankle joint position sense and increasing strength. The results of this study showed that KT exerted a greater effect on balance than hydrotherapy. However, no significant differences were found between the two methods in terms of strength gain. Hence, it can be posited that the enhanced balance in people with DPN is primarily attributable to improvements in joint position sense rather than increased strength of the dorsiflexor and plantar flexor muscles.
The current study also examined the effects of KT and hydrotherapy on fall risk in women with DPN. The findings showed that both interventions effectively lowered fall risk in women with DPN, with no significant differences between the two approaches. According to previous studies, closed kinetic chain activities improve balance by connecting the feet to the ground, making the ankle joint the primary mechanism for controlling the body’s center of gravity [37]. As a result, improving the accuracy of the ankle joint position sense can lead to a more accurate and timely diagnosis of bodily disturbances, enabling appropriate adjustments in ankle muscle contractions to effectively reduce the body’s center of gravity and postural sway in patients with DPN. Strengthening the anterior and posterior tibia muscles is another major factor in improving motor control and lowering fall risk [38]. Given the findings of the current study, which demonstrate that hydrotherapy and KT improve both ankle joint position sense and the strength of the ankle dorsiflexor and plantarflexor muscles, it is reasonable to conclude that these two factors collectively contribute to lowering the fall risk index in women with DPN.
Conclusion
Based on the findings, while both facilitatory KT and hydrotherapy exhibited positive effects on ankle joint position sense, strength, balance, and fall risk in women with DPN, facilitatory KT proved to be more effective on joint position sense and balance compared to hydrotherapy. As such, facilitatory KT can be considered a suitable, cost-effective, and easily accessible strategy to complement other therapeutic interventions for women with DPN. Given the potential effects of long-term KT application and hydrotherapy exercises on factors such as fasting blood sugar, insulin resistance, neuropathy symptoms, and neuropathy pain, it is recommended that future studies investigate these variables in both genders.
Ethical Considerations
Compliance with ethical guidelines
This studywas confirmed by the Ethics Committee of the University of Bojnord, Bojnord, Iran (Code: IR.UB.REC.1403.018). Written informed consent was obtained from all participants, who were assured that they could withdraw from the study at any stage of the tests or exercises without penalty. Moreover, they were assured that their personal and medical information would be kept confidential.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Writing the original draft, project administration, supervision, formal analysis, data curation, and conceptualization: Nader Nokhodchi; Resources, methodology, and investigation: Mohadeseh Haddad; Review, and editing, visualization, validation, and software: Nader Nokhodchi and Mohadeseh Haddad.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all participants for their valuable cooperation throughout this study.
References
Diabetes is one of the most common metabolic disorders worldwide, and its prevalence among adults has been increasing over recent decades. In 2013, approximately 382 million people had diabetes, and this number is expected to rise to 592 million by 2035. The disease is categorized into two major types: Type I (5-8%) and type II (the majority of patients) [1]. Type II diabetes, primarily affected by genetic predisposition and unhealthy lifestyle factors, is marked by insufficient or ineffective levels of insulin secretion [2].
A common long-term complication of diabetes is diabetic neuropathy, which is associated with severe pain, sensory loss, and a higher risk of ulcers and amputations [3]. This condition is categorized into autonomic neuropathy and sensorimotor neuropathy. Autonomic neuropathy impairs the function of internal structures, such as the cardiovascular, digestive, urinary, and reproductive systems, whereas sensorimotor neuropathy primarily affects the neuromuscular system. The three most frequent subtypes of sensorimotor diabetic neuropathy include peripheral polyneuropathy, focal neuropathy, and diabetic amyotrophy [4]. Peripheral polyneuropathy is the most prevalent type of diabetic neuropathy, accounting for at least 50% of patients with a 25-year history of type II diabetes [5]. Diabetic peripheral neuropathy (DPN) results in impaired blood flow and progressive degeneration of nerve fibers [4]. It primarily affects the lower extremities, with symptoms such as distal limb pain and numbness, which can increase the risk of ulceration [6]. Peripheral neuropathy is associated with both direct and indirect complications, including impaired proprioception and balance, decreased muscle strength, and increased fall risk [7].
In peripheral neuropathy, degeneration of sensory afferents leads to postural instability and defective proprioception in the lower extremities [8]. Proprioception refers to the afferent information from the body’s internal peripheral regions, provided by the mechanical receptors in the joints, skin, and muscles. Impairments in proprioception disrupt feedback mechanisms and affect motor control [9]. Reduced proprioceptive ability lowers postural stability in patients with DPN, elevating the risk of accidental falls, particularly in elderly patients [10]. As a result, the progression of neuropathy and proprioceptive decline can lower functional balance and contribute to movement difficulties in daily activities [11].
Muscle strength is another crucial contributor to balance, influenced by joint angle, muscle group, type of contraction, and contraction speed [12]. Studies have suggested that in diabetic patients, the strength of the ankle flexor and extensor muscles decreases by 17% and 14%, respectively [13]. Reduced muscle strength in patients with type I and type II diabetes has been reported as a late complication of DPN, often presenting alongside motor nerve involvement [14]. Therapeutic interventions for DPN typically include antidepressant, anti-inflammatory, and anticonvulsant drugs. Nevertheless, due to their potential side effects, some non-pharmacological interventions have been explored to improve DPN symptoms, including acupuncture, laser therapy, phototherapy, thermotherapy, kinesiotherapy, and hydrotherapy [15].
In recent years, hydrotherapy has gained considerable attention as a complementary treatment for physical and motor impairments [16]. Hydrotherapy exercises provide physiological benefits, especially for patients with sensorimotor disorders [17]. Accordingly, aquatic exercises have long been used as a common therapeutic approach to reduce the effects of peripheral neuropathy on the sensorimotor functions of individuals with diabetes.
Kinesio tape is an elastic therapeutic tape commonly used in rehabilitation settings and by athletes to alleviate muscle spasms and pain, enhance muscle contraction, facilitate or inhibit muscle activity, increase range of motion, and improve blood and lymphatic circulation as well as proprioception. Kinesio tapes are designed to support soft tissues without restricting their function [18].
Research findings suggest that KT can improve proprioception and joint stability by inhibiting overactive muscles and facilitating weak ones, reducing pain, decreasing pressure on irritated nerve tissues, and altering the recruitment pattern of muscle fibers depending on the direction and degree of stretch [19]. Generally, kinesio tapes are assumed to facilitate a muscle when applied from its origin to its insertion and inhibit it when applied in the opposite direction [20].
The rising popularity of taping techniques among athletes, coupled with their reported benefits in enhancing athletic performance, has generated significant interest in applying kinesio tapes to improve physical abilities and quality of life in patients with various sensorimotor disorders, including neuropathy. In this regard, Thakur et al. highlighted the beneficial effects of KT on sensorimotor indices among patients with diabetic neuropathy [21]. Considering the importance of facilitating lower limb muscle activity for improved functioning in individuals with diabetic neuropathy, this study aimed to achieve two objectives: (1) to examine the effect of facilitatory KT on sensorimotor indices among patients with DPN and (2) to compare this approach with hydrotherapy, a common treatment recommended for alleviating the neuropathic symptoms in patients with DPN.
Materials and Methods
This research employed a double-group pre-test-post-test design.
Study participants
The study population comprised women aged 40-60 years with DPN residing in Ferdows, South Khorasan Province, Iran. A convenience sample of 20 eligible women with DPN was recruited from the South Khorasan Diabetes Association (Ferdows branch).
The sample size encompassed the entire statistical population due to the limited number of women with DPN within the specified age range and region. The inclusion criteria for the study were a confirmed diagnosis of type II diabetes for at least five years by a medical specialist, current use of medications (metformin 500 mg twice daily with meals and glibenclamide 5–10 mg in the morning in a fasted state), a confirmed diagnosis of diabetic neuropathy based on clinical and laboratory diagnostic criteria, ability to complete balance assessments using the Michigan questionnaire with a minimum score of 7, functional independence in daily activities, no fear of water, previous pool experience within the last three years, ability to walk in water, and absence of medical contraindications.
Participants were excluded if they had foot ulcers, orthopedic problems or surgeries affecting walking, neurological complications other than diabetic neuropathy, peripheral vascular disease, central nervous system disorders (e.g. dementia, Parkinson disease, or multiple sclerosis), musculoskeletal deformities of the lower extremities, uncontrolled cardiovascular or respiratory conditions, uncorrected visual acuity worse than 20/70, history of dizziness, uncontrolled hypertension, resting tachycardia or arrhythmia, or an allergy to tape [21, 22].
An orientation session was held to familiarize all participants with the research and measurement procedures. Participants were then randomly assigned to hydrotherapy or KT groups using a simple randomization method, achieved through drawing numbered envelopes.
Exercise protocol
The hydrotherapy group participated in an 8-week training protocol consisting of three water-based exercise sessions per week, including warm-up, stretching, and strengthening exercises (Table 1) [16].
Kinesio taping
The kinesio tape used in this study was Kindmax, a 5-cm-wide tape manufactured by Shanghai Sport Product, China. The tape was applied to the tibialis anterior, extensor digitorum longus, extensor hallucis longus, peroneus longus, and gastrocnemius muscles for 24 hours a day over 8 weeks. It was replaced every five days (Figure 1). The tape was stretched to approximately 50% of its original length and applied from the muscle’s origin to its insertion [19].
1) Tibialis anterior: Participants lay supine on a treatment table while kinesio tapes were applied to their tibialis anterior muscles. The tape was anchored at the muscle’s origin (lateral condyle) and proximal anterolateral tibia. While the participants performed plantarflexion and eversion, the tape was tightened and secured to the muscle’s insertion point (lateral cuneiform bone surface).
2) Extensor digitorum longus: An inverted Y-shaped tape was applied, anchored at the muscle’s origin (lateral tibial condyle, distal three-quarters of medial fibula). Participants were then directed to dorsiflex the foot and extend the lateral four toes as the tape was secured from the metatarsophalangeal joints to the middle and distal phalanges of the lateral four toes.
3) Extensor hallucis longus: An I-shaped tape was applied to this muscle from the muscle’s origin in the mid-anterior surface of the ulna to the posterior aspect of the thumb’s distal phalanx.
4) Peroneus longus: The participant lay supine when the long fibular muscle was taped. The tape was secured at the proximal and lateral fibula, applied along the entire lateral surface of the leg, passed behind the lateral malleolus, and secured at the mid-lateral foot.
5) Gastrocnemius: The knee was fully extended to apply the tape on the gastrocnemius. The tape was anchored from the origin (posterior surface of the medial and lateral distal femoral condyles) to the posterior surface of the calcaneus.
Ankle joint position sense
The ankle joint position sense was evaluated using the active repositioning test at target angles of 10° and 20° for dorsiflexion and plantarflexion. A Biometrics Ltd. electrogoniometer (accuracy ±0.1°) was used for the measurements. The test was conducted separately for each leg while participants sat on a chair with their legs hanging freely. Each participant leaned against the backrest at a 90° angle. The researcher moved the ankle to the target angle at a steady rate of nearly 6° per second, maintained it for 5 seconds, and then slowly returned the limb to the starting position. Subsequently, participants were instructed to reproduce the same angle with their eyes closed. The difference between the reproduced and target angles was measured by an electrogoniometer. Each participant was assessed three times for each leg in both dorsiflexion and plantarflexion conditions, and the average of the three attempts for both legs was calculated as their score [23].
Strength
A Siemens Siwarex WL 250 model 7MH5105 load cell (Germany), with a 500 kg weight capacity, was employed in this study to measure the maximum strength of the anterior and posterior leg muscles. Participants were seated with their knees straight and their ankles positioned at a 90° angle relative to their legs. The equipment was adjusted to prevent any undesirable movement. Each participant performed three attempts for each test and each leg and was verbally encouraged to achieve maximum voluntary contraction. A 60-second rest period was provided between each attempt. The mean maximum strength from all three attempts across both legs was recorded as the dorsiflexion and plantarflexion muscle strength scores [24].
Balance
The Berg balance scale was employed to assess balance. This test is a reliable, functional scale for evaluating balance disorders in the elderly population. The scale consists of 14 items that assess both static and dynamic balance. The items are scored on a 5-point Likert scale (0-4) based on the quality or duration of task performance. The maximum scale score is 56, and a score below 45 indicates a high risk of falling [22]. This scale includes the following items:
1) standing up unsupported; 2) sitting unsupported; 3) standing up from a sitting position; 4) sitting down from a standing position; 5) standing with closed eyes; 6) transferring from one chair to another; 7) standing with feet together; 8) picking up an object from the floor while standing; 9) reaching forward with outstretched arms; 10) turning around in a complete rotation 11) turning right and left to look back; 12) placing the feet alternately on a stool; 13) standing on one leg, and 14) standing independently with one foot in front of the other [25].
International fall efficiency scale
This scale consists of 16 items rated on a 4-point Likert scale ranging from “not at all worried” to “completely worried” (scores 1 to 4). Higher scores indicate a greater fear of falling. The scale demonstrates strong reliability and validity, with a Pearson correlation coefficient of 0.70 and an intraclass correlation coefficient of 0.98 [26].
Statistical analysis
The collected data were analyzed using the SPSS software, version 16. The significance level was set at P<0.05. First, the normality of the data was verified using the Shapiro-Wilk test. Independent samples t-tests were conducted to compare baseline mean differences between groups, while paired samples t-tests were employed to assess within-group changes. Analysis of covariance (ANCOVA) was used to compare between-group differences. Results are presented as Mean±SD.
Results
A total of 20 participants with DPN completed the study. Table 2 presents the demographic characteristics of the participants.
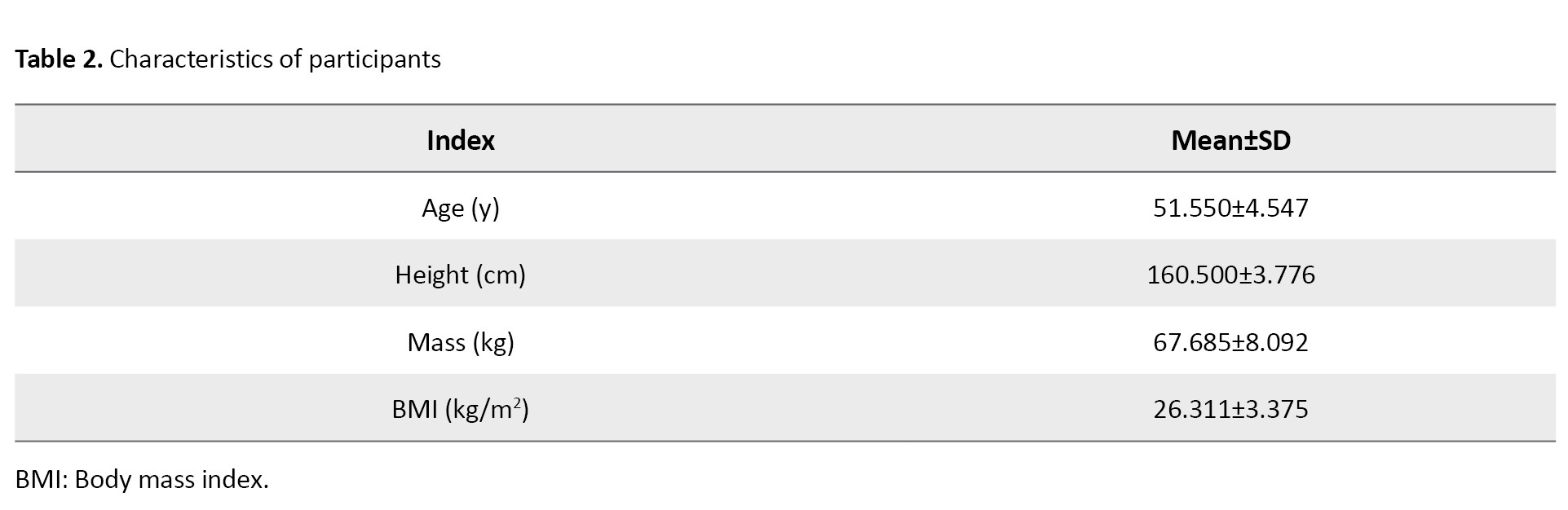
Based on the independent-samples t-test results (Table 3), no significant baseline differences were observed between the hydrotherapy and KT groups in terms of age, body mass index (BMI), and neuropathy severity (P>0.05).
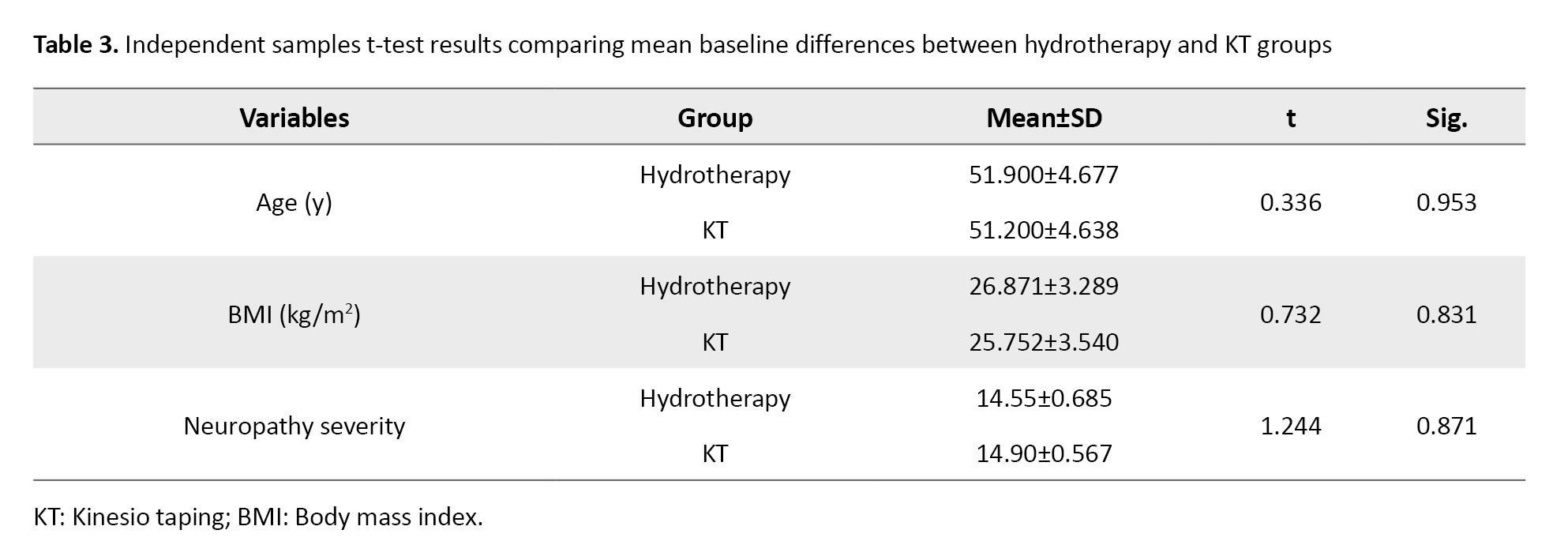
Based on the paired-samples t-test results (Table 4), eight weeks of hydrotherapy exercises and the application of facilitatory KT led to significant improvements in ankle joint position sense (both dorsiflexion and plantarflexion), strength, balance, and fall risk in women with DPN (P<0.05).
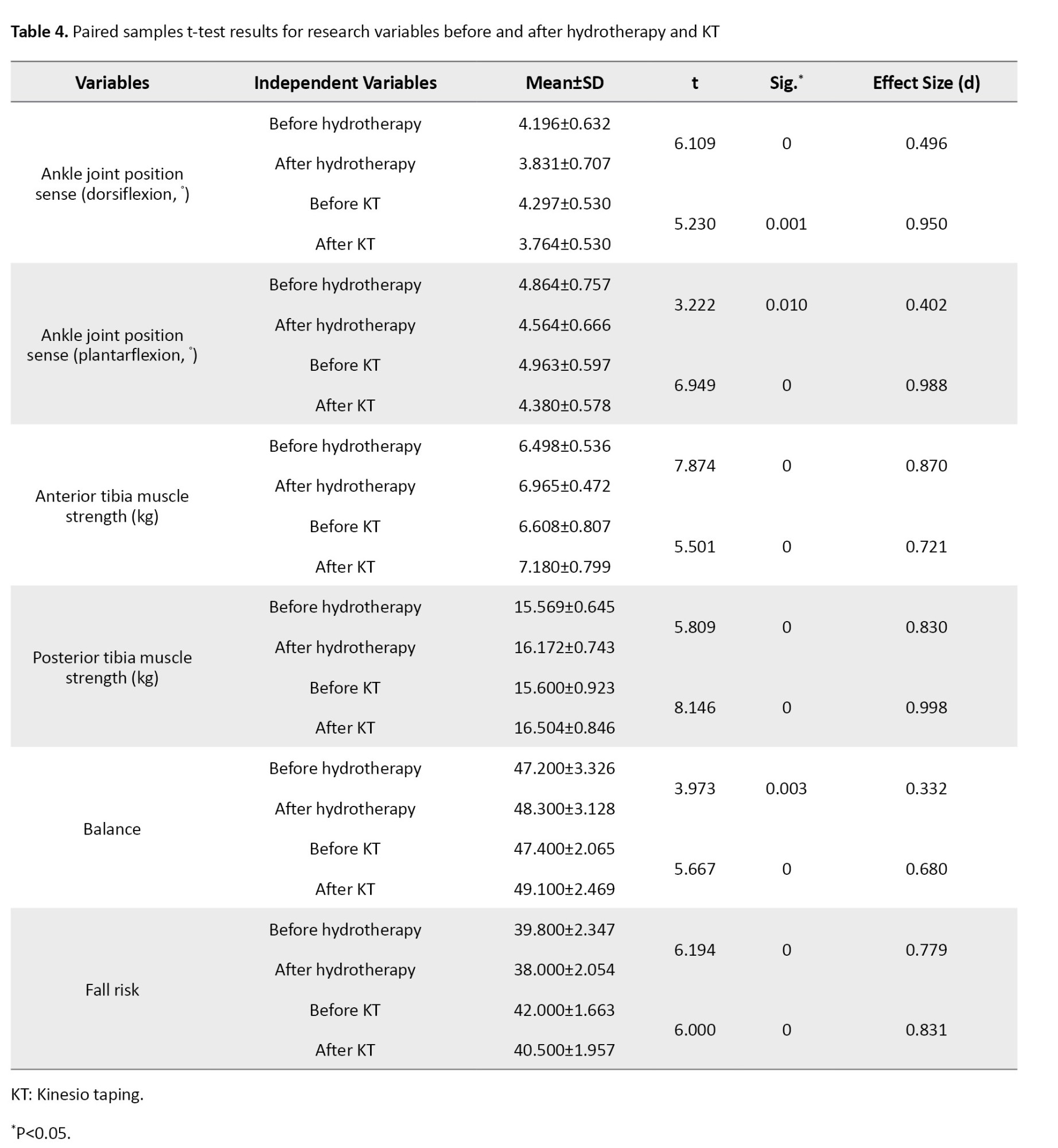
Moreover, the ANCOVA results (Table 5 and Figure 2) indicated a significant difference between the effects of facilitatory KT and hydrotherapy on ankle joint position sense in both dorsiflexion and plantarflexion positions of the ankle joint, as well as on balance (P<0.05).
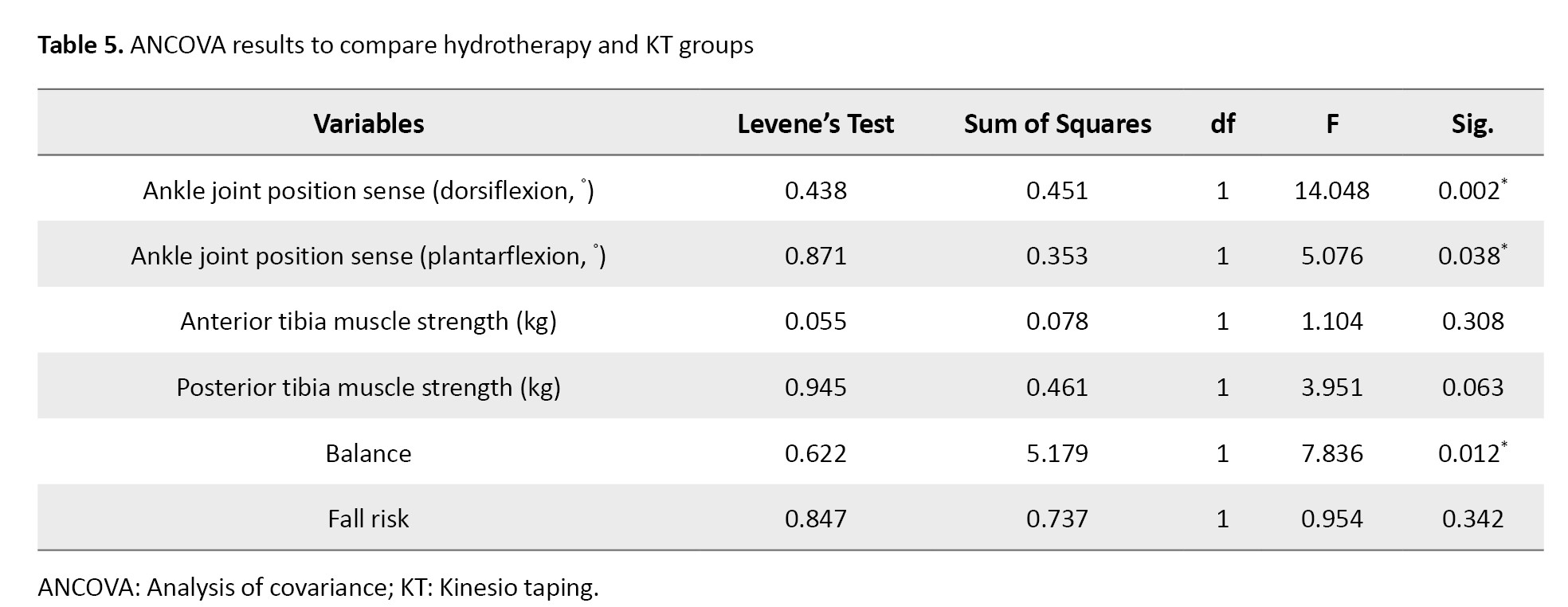
However, no significant differences were observed between the effects of KT and hydrotherapy on muscle strength and fall risk.
Discussion
This study sought to investigate and compare the effects of hydrotherapy exercises and facilitatory KT on ankle joint position sense, strength, balance, and fall risk in women with DPN. The results revealed that an 8-week intervention involving either hydrotherapy or the application of facilitatory KT improved ankle joint position sense in women with DPN. However, KT produced a greater effect size than hydrotherapy.
Relying on joint and muscle receptors, joint position sense plays a crucial role in the perception of limb and joint position. Known as the primary receptors involved in joint position sense, muscle spindles are affected by changes in muscle length as well as inputs from skin and joint receptors [27]. According to previous research, joint receptors complement muscle receptors in the joint position sense, particularly during joint stretching or compression [28]. The majority of previous research has confirmed the effectiveness of sports exercises in improving proprioception and joint position sense in patients with DPN [29]. Likewise, hydrotherapy exercises have been shown to improve proprioception and position sense in individuals with DPN [16]. The results of the current study are consistent with these findings.
It is necessary to investigate potential central mechanisms to determine the reasons behind the improvement in joint position sense following participation in hydrotherapy exercises. In this regard, increased attention may be a potential mechanism for improving exercise-induced proprioception. The hydrotherapy exercises used in the current study appear to have increased participants’ attention to proprioceptive cues at both automatic and conscious levels, paving the way for participants to improve their position sense. Furthermore, studies have demonstrated that training increases the output of muscle spindles, which may improve movement accuracy by modulating muscle tonicity [30].
Moreover, the current study’s findings revealed the beneficial effects of facilitatory KT on joint position sense, which aligns with the results reported by Thakur et al. KT exerts pressure, heat, and cutaneous stimulation that activate joint receptors and improve ankle joint position sense in women with DPN. Although the precise mechanism underlying KT’s facilitative effect is not fully understood, researchers have proposed two possible hypotheses. The first highlights increased lymph and blood flow as a result of skin elevation and the subsequent expansion of the space between the skin and underlying muscles in the KT area. The second hypothesis argues that KT stimulates cutaneous mechanoreceptors and activates central nervous system regulatory mechanisms, thereby enhancing muscle activation through tension and pressure applied to the skin beneath the tape. In this regard, recent research has demonstrated the positive impact of facilitative KT on enhancing muscular electrical activity [31, 32].
Furthermore, the current study found that KT exerted greater beneficial effects on position sense and a larger effect size than hydrotherapy. The angles used to investigate joint position sense in this study were in the mid-range of motion (10° dorsiflexion and 20° plantarflexion). At these angles, the muscle spindle plays a more significant role than joint receptors. Therefore, muscle activity facilitation by a KT could increase muscle spindle stimulation through tensile forces, resulting in a greater accuracy in position sense.
The current study also found that 8 weeks of hydrotherapy exercises or KT improved the strength of ankle flexor and extensor muscles in women with DPN, with no significant difference between the two interventions. Previous studies have demonstrated that resistance training can enhance muscle strength in individuals with DPN [33]. The findings of the current study similarly indicate that aquatic exercises can enhance lower extremity muscle strength in women with DPN.
The possible reasons behind improved muscle strength following hydrotherapy exercises can include neural adaptations such as reduced resistance in nerve pathways to impulse transmission, cortical sensorimotor reorganization, reduced inhibitory nerve reflexes, use of more efficient motor units, increased activation of the nervous system, enhanced efficiency and strength of synaptic communication, and facilitated transfer of data from every sense [34]. Moreover, the results of the present study revealed that the use of facilitatory KT increased the strength of the ankle dorsiflexor and plantarflexor muscles. Earlier studies, such as those by Ahmed et al, have also reported the positive effects of resistance training combined with KT on muscular strength in individuals with DPN [19]. KT widens the interstitial space between the skin and soft tissues, resulting in increased local blood flow, reduced local edema, and stimulation of the skin, muscle, and fascia. Consequently, this provides more effective sensory input to the central nervous system, resulting in reduced muscle inhibition and stronger muscle contractions. Given that the facilitation technique was used for taping, it was expected to increase strength by stimulating muscle spindles, as confirmed by the current study findings.
This study further indicated that 8 weeks of hydrotherapy or KT improved balance and reduced the risk of falls in women with DPN. Additionally, the findings revealed that the facilitatory application of kinesio tape had a greater effect on improving balance than hydrotherapy. However, there were no significant differences between the two groups in terms of fall risk reduction. In this regard, previous studies by Sakinepoor et al. and Shourabi et al. have demonstrated that both aquatic exercise and resistance training improve balance in individuals with DPN [16, 35]. They have also reported that in-water therapeutic exercises exert a greater effect on balance than resistance training [35]. In line with these findings, the current study suggests that increased joint position sense, a crucial component of balance control, may be a possible explanation for the observed improvement in balance. To maintain proper balance, the motor control system must continuously monitor changes in joint position [36]. The results of this study indicate that joint position sense improved significantly after hydrotherapy and kinesio tape application. As a result, it is reasonable to conclude that an improvement in joint position sense is one of the most likely causes of improved balance in women with DPN. Another important factor in maintaining balance is strength, which helps to prevent postural fluctuations. Indeed, a decline in muscle strength is considered a health concern that can compromise balance [34]. This study found that hydrotherapy exercises and KT increased strength in individuals with DPN. Therefore, increased strength could be the second possible cause of improved balance in women with DPN.
As muscle weakness, impaired balance, and motor control problems all contribute to falls, hydrotherapy can be an effective strategy to improve balance and prevent falls. This is because increasing muscle strength and balance leads to better motor control and a lower fear of falling. Regarding the positive effects of KT on improving balance and lowering fall risk in women with DPN, it can be argued that the enhanced balance following the use of kinesio tapes can be attributed to their effects on improving ankle joint position sense and increasing strength. The results of this study showed that KT exerted a greater effect on balance than hydrotherapy. However, no significant differences were found between the two methods in terms of strength gain. Hence, it can be posited that the enhanced balance in people with DPN is primarily attributable to improvements in joint position sense rather than increased strength of the dorsiflexor and plantar flexor muscles.
The current study also examined the effects of KT and hydrotherapy on fall risk in women with DPN. The findings showed that both interventions effectively lowered fall risk in women with DPN, with no significant differences between the two approaches. According to previous studies, closed kinetic chain activities improve balance by connecting the feet to the ground, making the ankle joint the primary mechanism for controlling the body’s center of gravity [37]. As a result, improving the accuracy of the ankle joint position sense can lead to a more accurate and timely diagnosis of bodily disturbances, enabling appropriate adjustments in ankle muscle contractions to effectively reduce the body’s center of gravity and postural sway in patients with DPN. Strengthening the anterior and posterior tibia muscles is another major factor in improving motor control and lowering fall risk [38]. Given the findings of the current study, which demonstrate that hydrotherapy and KT improve both ankle joint position sense and the strength of the ankle dorsiflexor and plantarflexor muscles, it is reasonable to conclude that these two factors collectively contribute to lowering the fall risk index in women with DPN.
Conclusion
Based on the findings, while both facilitatory KT and hydrotherapy exhibited positive effects on ankle joint position sense, strength, balance, and fall risk in women with DPN, facilitatory KT proved to be more effective on joint position sense and balance compared to hydrotherapy. As such, facilitatory KT can be considered a suitable, cost-effective, and easily accessible strategy to complement other therapeutic interventions for women with DPN. Given the potential effects of long-term KT application and hydrotherapy exercises on factors such as fasting blood sugar, insulin resistance, neuropathy symptoms, and neuropathy pain, it is recommended that future studies investigate these variables in both genders.
Ethical Considerations
Compliance with ethical guidelines
This studywas confirmed by the Ethics Committee of the University of Bojnord, Bojnord, Iran (Code: IR.UB.REC.1403.018). Written informed consent was obtained from all participants, who were assured that they could withdraw from the study at any stage of the tests or exercises without penalty. Moreover, they were assured that their personal and medical information would be kept confidential.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Writing the original draft, project administration, supervision, formal analysis, data curation, and conceptualization: Nader Nokhodchi; Resources, methodology, and investigation: Mohadeseh Haddad; Review, and editing, visualization, validation, and software: Nader Nokhodchi and Mohadeseh Haddad.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all participants for their valuable cooperation throughout this study.
References
- Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diab Res Clin Prac. 2014; 103(2):137-49. [DOI:10.1016/j.diabres.2013.11.002] [PMID]
- Olokoba AB, Obateru OA, Olokoba LB. Type 2 diabetes mellitus: A review of current trends. Oman Med Journal. 2012; 27(4):269-73. [DOI:10.5001/omj.2012.68] [PMID]
- Booya F, Bandarian F, Larijani B, Pajouhi M, Nooraei M, Lotfi J. Potential risk factors for diabetic neuropathy: A case control study. BMC Neurol. 2005; 5:24. [DOI:10.1186/1471-2377-5-24] [PMID]
- Vinik AI, Nevoret ML, Casellini C, Parson H. Diabetic neuropathy. Endocrinol Metab Clin North Am. 2013; 42(4):747-87. [DOI:10.1016/j.ecl.2013.06.001] [PMID]
- Feldman EL, Russell JW, Sullivan KA, Golovoy D. New insights into the pathogenesis of diabetic neuropathy. Curr Opin Neurol. 1999; 12(5):553-63. [DOI:10.1097/00019052-199910000-00009] [PMID]
- Rathur HM, Boulton AJ. The neuropathic diabetic foot. Nat Clin Pract Endocrinol Metab. 2007; 3(1):14-25. [DOI:10.1038/ncpendmet0347]
- Bagherzadeh Cham M, Mohseni-Bandpei MA, Bahramizadeh M, Forogh B, Kalbasi S, Biglarian A. Effects of vibro-medical insoles with and without vibrations on balance control in diabetic patients with mild-to-moderate peripheral neuropathy. J Biomech. 2020;103:109656. [DOI:10.1016/j.jbiomech.2020.109656] [PMID]
- Nardone A, Grasso M, Schieppati M. Balance control in peripheral neuropathy: Are patients equally unstable under static and dynamic conditions? Gait Posture. 2006; 23(3):364-73. [DOI:10.1016/j.gaitpost.2005.04.002] [PMID]
- Guede-Rojas F, Benavides-Villanueva A, Salgado-González S, Mendoza C, Arias-Álvarez G, Soto-Martínez A, et al. Effect of strength training on knee proprioception in patients with knee osteoarthritis: A systematic review and meta-analysis. Sports Med Health Sci. 2024; 6(2):101-10. [DOI:10.1016/j.smhs.2023.10.005] [PMID]
- Ites KI, Anderson EJ, Cahill ML, Kearney JA, Post EC, Gilchrist LS. Balance interventions for diabetic peripheral neuropathy: A systematic review. J Geriatr Phys Ther. 2011; 34(3):109-16. [DOI:10.1519/JPT.0b013e318212659a] [PMID]
- Trikkalinou A, Papazafiropoulou AK, Melidonis A. Type 2 diabetes and quality of life. World J Diab. 2017;8(4):120-9. [DOI:10.4239/wjd.v8.i4.120] [PMID]
- Ghaderiyan M, Ghasemi G. [Comparison of the amount and ratio of ankle muscles isometric strength in persons with planus, cavus and normal foot types (Persian)]. Stud Sport Med. 2017; 8(20):53-72. [DOI:10.22089/smj.2017.898]
- Andersen H, Nielsen S, Mogensen CE, Jakobsen J. Muscle strength in type 2 diabetes. Diabetes. 2004; 53(6):1543-8. [DOI:10.2337/diabetes.53.6.1543] [PMID]
- Womack L, Peters D, Barrett EJ, Kaul S, Price W, Lindner JR. Abnormal skeletal muscle capillary recruitment during exercise in patients with type 2 diabetes mellitus and microvascular complications. J Am Coll Cardiol. 2009; 53(23):2175-83. [DOI:10.1016/j.jacc.2009.02.042] [PMID]
- Shanb AA, Youssef EF, Al Baker WI, Al-Khamis FA, Hassan A, Jatoi NA. The efficacy of adding electromagnetic therapy or laser therapy to medications in patients with diabetic peripheral neuropathy. J Lasers Med Sci. 2020; 11(1):20-8. [DOI:10.15171/jlms.2020.05] [PMID]
- Shourabi P, Bagheri R, Ashtary-Larky D, Wong A, Motevalli MS, Hedayati A, et al. Effects of hydrotherapy with massage on serum nerve growth factor concentrations and balance in middle aged diabetic neuropathy patients. Complement Ther Clin Pract. 2020; 39:101141. [DOI:10.1016/j.ctcp.2020.101141] [PMID]
- Lee BA, Oh DJ. The effects of aquatic exercise on body composition, physical fitness, and vascular compliance of obese elementary students. J Exerc Rehabil. 2014; 10(3):184-90. [DOI:10.12965/jer.140115] [PMID]
- Aghaie P, Abbasi A, Letafatkar A. [The immediate effect of facilitatory and inhibitory Kinesio taping on the muscular activity and fatigue of the elbow flexor muscles (Persian)]. Stud Sport Med. 2021; 13(29):207-28. [DOI:10.22089/smj.2021.11497.1540]
- Ahmed AE, Mohamed NI, Mariam EM, Ahmed M. Effect of Kinesio tape versus resistive exercise on dorsiflexors functional performance in diabetic peripheral neuropathy. Med J Cairo Univ. 2020; 88:1777-82. [DOI:10.21608/mjcu.2020.116827]
- Nokhodchi N, Hosseini M, Attaran Iraj Z, Rahimi A. The effects of Kinesio-tape through facilitation of hamstring and inhibition of quadriceps on biomechanical variables affecting anterior cruciate ligament injury when landing in active healthy young women. J Adv Sport Technol. 2020; 4(2):104-13. [Link]
- Thakur K, Goyal M. Effectiveness of neuromuscular taping on balance, proprioception, pain, and nerve conduction parameters in patients with diabetic peripheral neuropathy: A two-group pretest-posttest randomized sham-controlled trial study protocol. J Diabetes Metab Disord. 2023; 22(2):1793-800. [DOI:10.1007/s40200-023-01275-5] [PMID]
- Balducci S, Iacobellis G, Parisi L, Di Biase N, Calandriello E, Leonetti F, et al. Exercise training can modify the natural history of diabetic peripheral neuropathy. J Diabetes Complications. 2006; 20(4):216-23. [DOI:10.1016/j.jdiacomp.2005.07.005] [PMID]
- Ghazavi N, Sadat SJ, Rostaei N. Effect of proprioceptive exercises on lower extremity proprioception in patients with diabetic neuropathy. J Clin Care Skills. 2021; 2(4):201-5. [DOI:10.52547/jccs.2.4.201]
- Martinelli AR, Mantovani AM, Nozabieli AJ, Ferreira DM, Barela JA, de Camargo MR, et al. Muscle strength and ankle mobility for the gait parameters in diabetic neuropathies. Foot. 2013; 23(1):17-21. [DOI:10.1016/j.foot.2012.11.001] [PMID]
- Badura P, Pietka E. Automatic Berg Balance Scale assessment system based on accelerometric signals. Biomed Signal Process Control. 2016; 24:114-9. [DOI:10.1016/j.bspc.2015.10.005]
- Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990; 45(6):P239-43. [DOI:10.1093/geronj/45.6.P239] [PMID]
- Lephart SM, Fu FH. The role of proprioception in the treatment of sports injuries. Sports Exerc Inj. 1995; 1(2):96-102. [Link]
- Hall JE, Hall ME. Textbook of medical physiology. Philadelphia: Elsevier; 2021. [Link]
- Hernandez-Secorun M, Vidal-Peracho C, Marquez-Gonzalvo S, Corral-de-Toro J, Müller-Thyssen-Uriarte J, et al. Exercise and manual therapy for diabetic peripheral neuropathy: A systematic review. Appl Sci. 2021; 11(12):5665. [DOI:10.3390/app11125665]
- Ashton-Miller JA, Wojtys EM, Huston LJ, Fry-Welch D. Can proprioception really be improved by exercises? Knee Surg Sports Traumatol Arthrosc. 2001; 9(3):128-36. [DOI:10.1007/s001670100208] [PMID]
- Sinaei E, Foroozantabar V, Kordi Yoosefinejad A, Sobhani S, Motealleh A. Electromyographic comparison of vastus medialis obliquus facilitatory versus vastus lateralis inhibitory Kinesio taping in athletes with patellofemoral pain: A randomized clinical trial. J Bodyw Mov Ther. 2021; 28:157-63. [DOI:10.1016/j.jbmt.2021.07.017] [PMID]
- Raza A, Zaki S, Alam MF, Sharma S, Aysha T, Khiyami AT, et al. Effects of facilitatory and inhibitory Kinesio taping on lateral gastrocnemius muscle activity, motor neuron excitability, and countermovement jump height in university athletes from multiple sports: A randomized controlled trial. Heliyon. 2023; 9(12):e23230. [DOI:10.1016/j.heliyon.2023.e23230] [PMID]
- Badri N, Hamedinia MR, Hosseini Kakhk AR, Askari R, Azizi R. [The effect of two types of combined training on physical performance and body composition in type 2 diabetic women with peripheral neuropathy (Persian)]. J Health Care. 2019; 21(1):77-89. [DOI:10.29252/jhc.21.1.77]
- Candeloro JM, Caromano FA. Effect of a hydrotherapy program on flexibility and muscle strength in elderly women. Braz J Phys Ther. 2007; 11(4):303-9. [DOI:10.1590/S1413-35552007000400010]
- Sakinepoor A, Naderi A, Mazidi M, Hashemian AH, Mirzaei M, Letafatkar A. [Effect of resistance and aquatic exercises on balance in diabetes peripheral neuropathy patients: A randomized clinical trial study (Persian)]. J Diabetes Nurs. 2019; 7(4):968-82. [Link]
- de Noronha M, França LC, Haupenthal A, Nunes GS. Intrinsic predictive factors for ankle sprain in active university students: A prospective study. Scand J Med Sci Sports. 2013; 23(5):541-7. [DOI:10.1111/j.1600-0838.2011.01434.x] [PMID]
- Koenig JP, Puckree T. Injury prevalence, stability and balance among female adolescent soccer players injury. Afr J Phys Health Educ Recreat Dance. 2015; 21(1.1):81-91. [Link]
- Geigle PR, Cheek WL Jr, Gould ML, Hunt CH, Shafiq B. Aquatic physical therapy for balance: the interaction of somatosensory and hydrodynamic principles. J Aquat Phys Ther. 1997; 5(1):4-10. [Link]
Type of Study: Research |
Subject:
Rehabilitation management
Received: 2025/09/7 | Accepted: 2025/09/22 | Published: 2025/03/2
Received: 2025/09/7 | Accepted: 2025/09/22 | Published: 2025/03/2