Volume 8, Issue 1 (Continuously Updated 2025)
Func Disabil J 2025, 8(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Balali N, Irani A, Rayegani S M. Cognitive Impairment and Fall Risk in Multiple Sclerosis: A Review Study. Func Disabil J 2025; 8 (1)
URL: http://fdj.iums.ac.ir/article-1-292-en.html
URL: http://fdj.iums.ac.ir/article-1-292-en.html
1- Department of Occupational Therapy, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran. , negar.balali@sbmu.ac.ir
2- Department of Occupational Therapy, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
3- Department of Physical Medicine and Rehabilitation, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Department of Occupational Therapy, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
3- Department of Physical Medicine and Rehabilitation, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 779 kb]
(641 Downloads)
| Abstract (HTML) (1216 Views)
Selection criteria
The author screened all studies for inclusion in this review. Relevant studies were selected based on their titles, abstracts, and when additional information was required, based on their full texts.
Inclusion criteria
The inclusion criteria for this study were as follows:
Studies that assessed the relationship between cognitive function and fall risk in pwMS.
Studies whose outcomes were related to fall risk and cognition in pwMS.
Studies in which the participants had a confirmed diagnosis of Multiple Sclerosis.
Studies with full-text access.
Exclusion criteria
The exclusion criteria for this study, based on which irrelevant studies were excluded, included:
Studies that examined only one variable (fall risk or cognitive/executive function) about MS. Studies that focused on pwMS with comorbid psychological disorders. Studies that did not assess the effect of rehabilitation interventions on both fall risk and executive performance. Duplicate studies already included in previous review studies.
Quality assessment of methodology
The quality of the reviewed studies and clinical trials included in this research was assessed using the CASP checklist, which covers various aspects also evaluated by other checklists. Cross-sectional and cohort studies were evaluated with the STROBE checklist, which comprehensively assesses the strengths, weaknesses, and generalizability of these studies [11, 12]. These checklists evaluate the studies based on their methodology and determine how statistically reliable their results are for decision-making.
Data extraction
The author extracted demographic information of the pwMS from the included studies, such as age, gender, and cognitive level. Additionally, the study results and the number of pwMS in each study were extracted.
Results
Literature search and methodology quality assessment
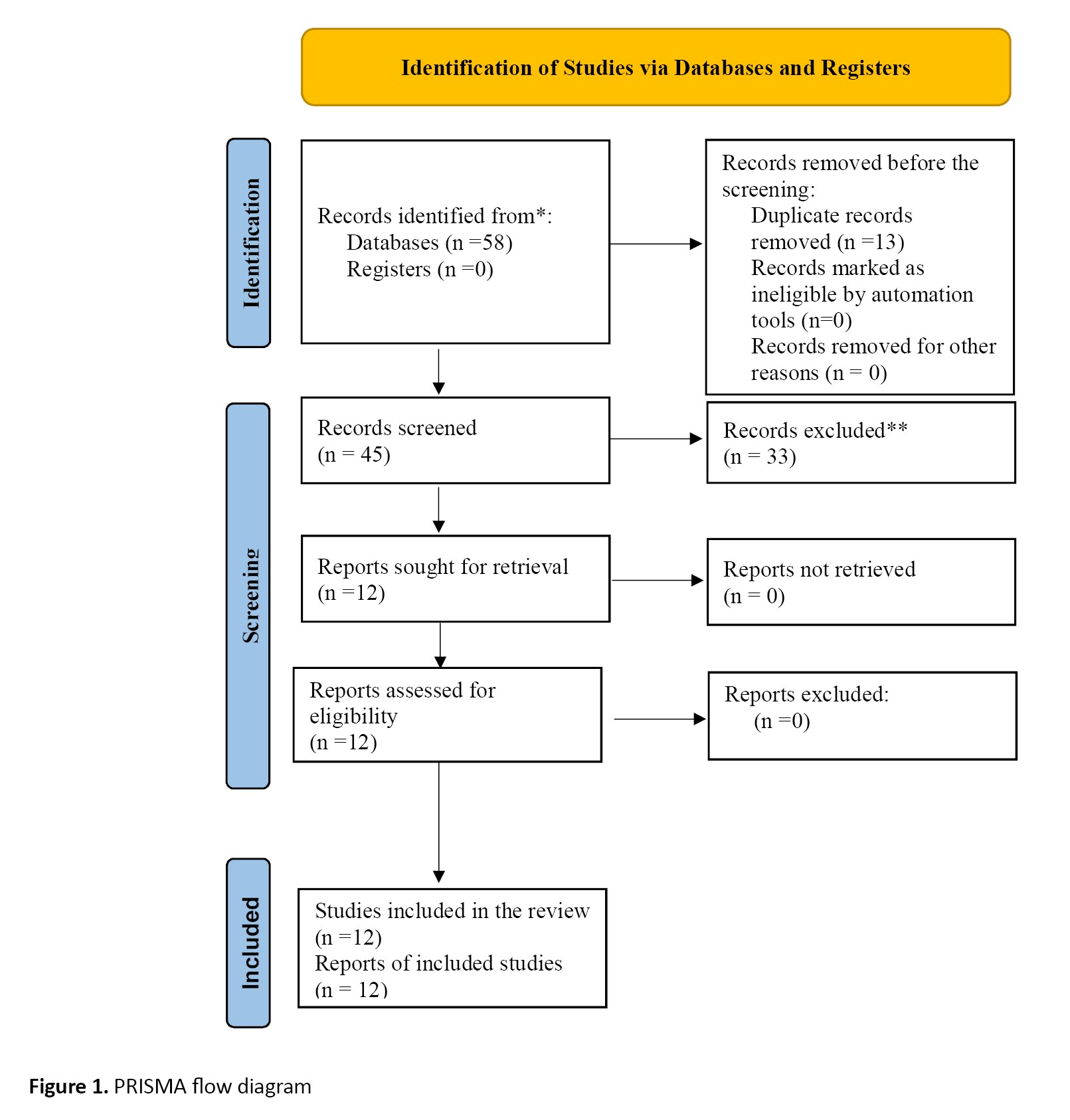
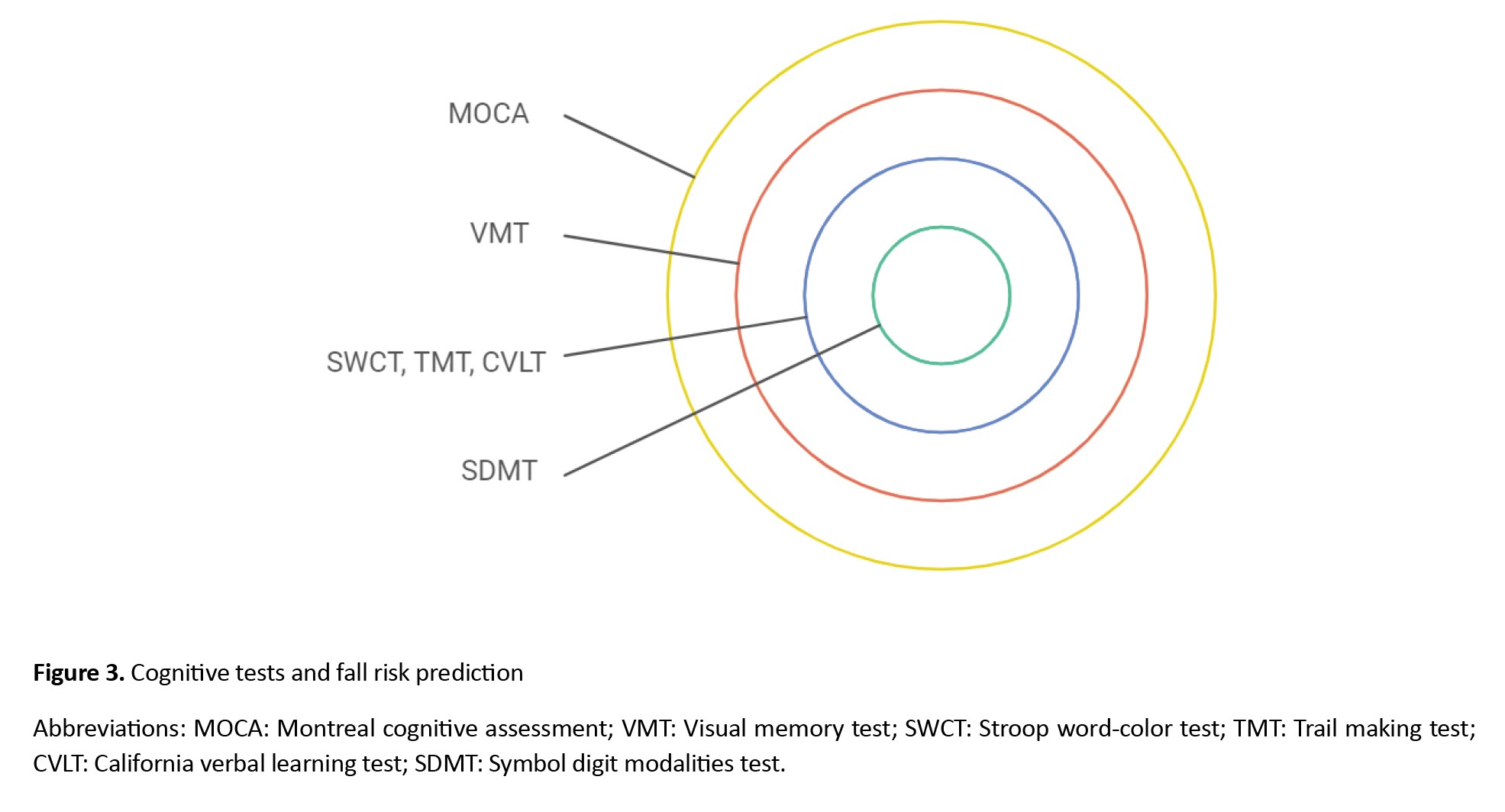
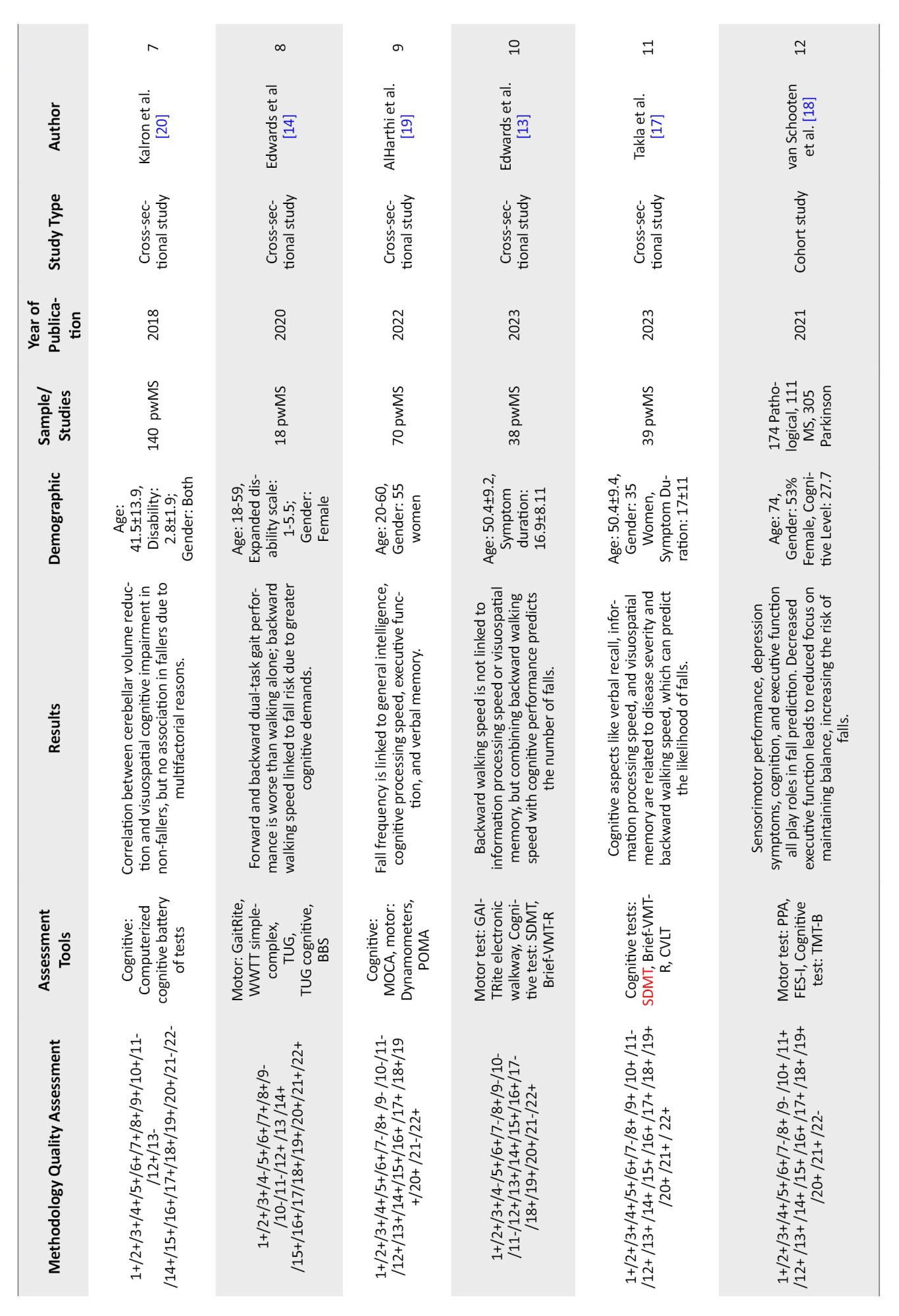
At the beginning of the search, 58 studies were identified based on their titles. After applying the inclusion and exclusion criteria, 12 studies were selected, and the other studies were excluded due to not meeting the inclusion criteria. Table 1 presents the quality of the included studies and the extracted data from each study.
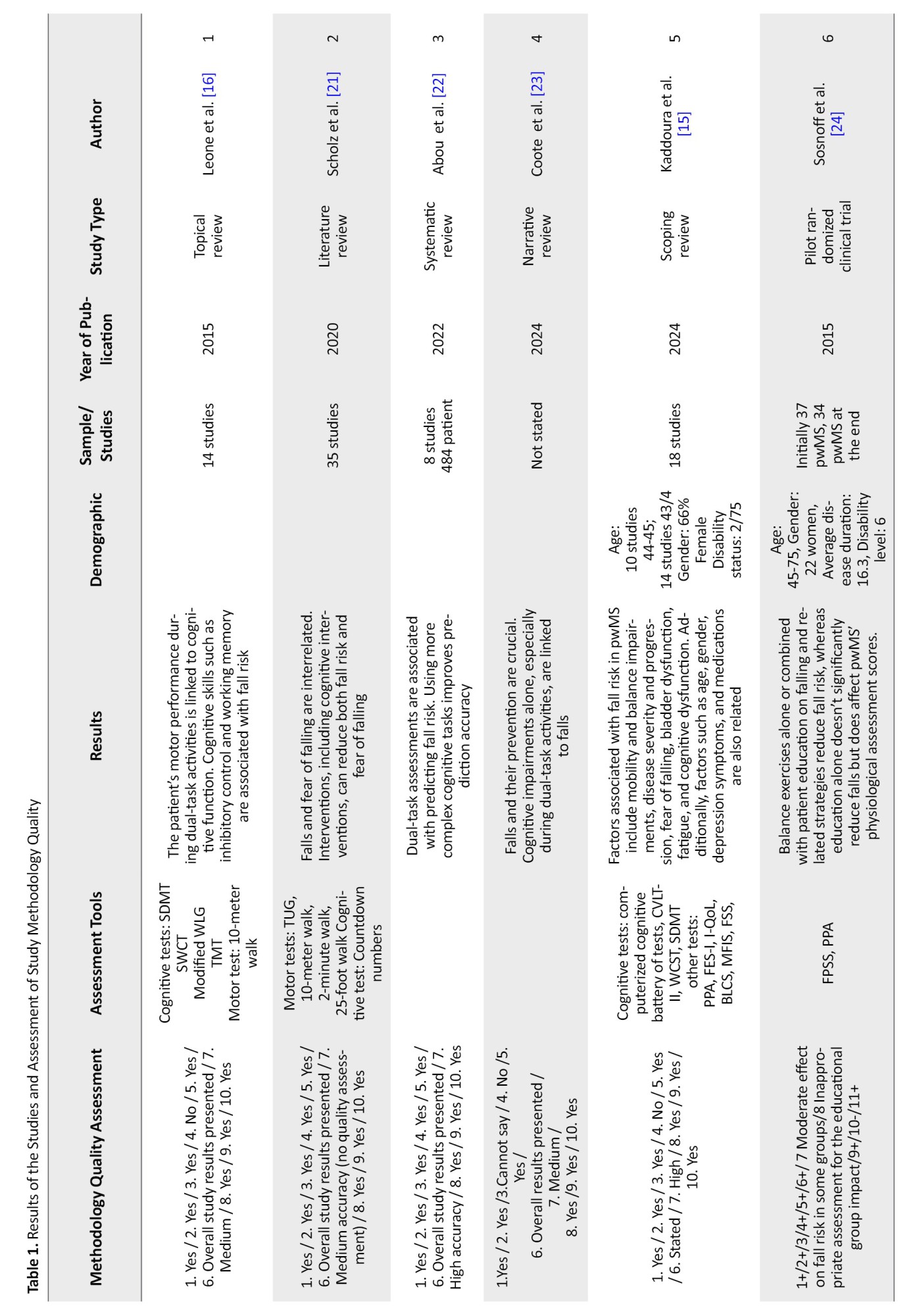
Executive function encompasses various cognitive skills, such as attention, planning, working memory, organization, cognitive flexibility, inhibition, problem-solving, and more. The assessment tools used in the reviewed studies to evaluate executive function include:
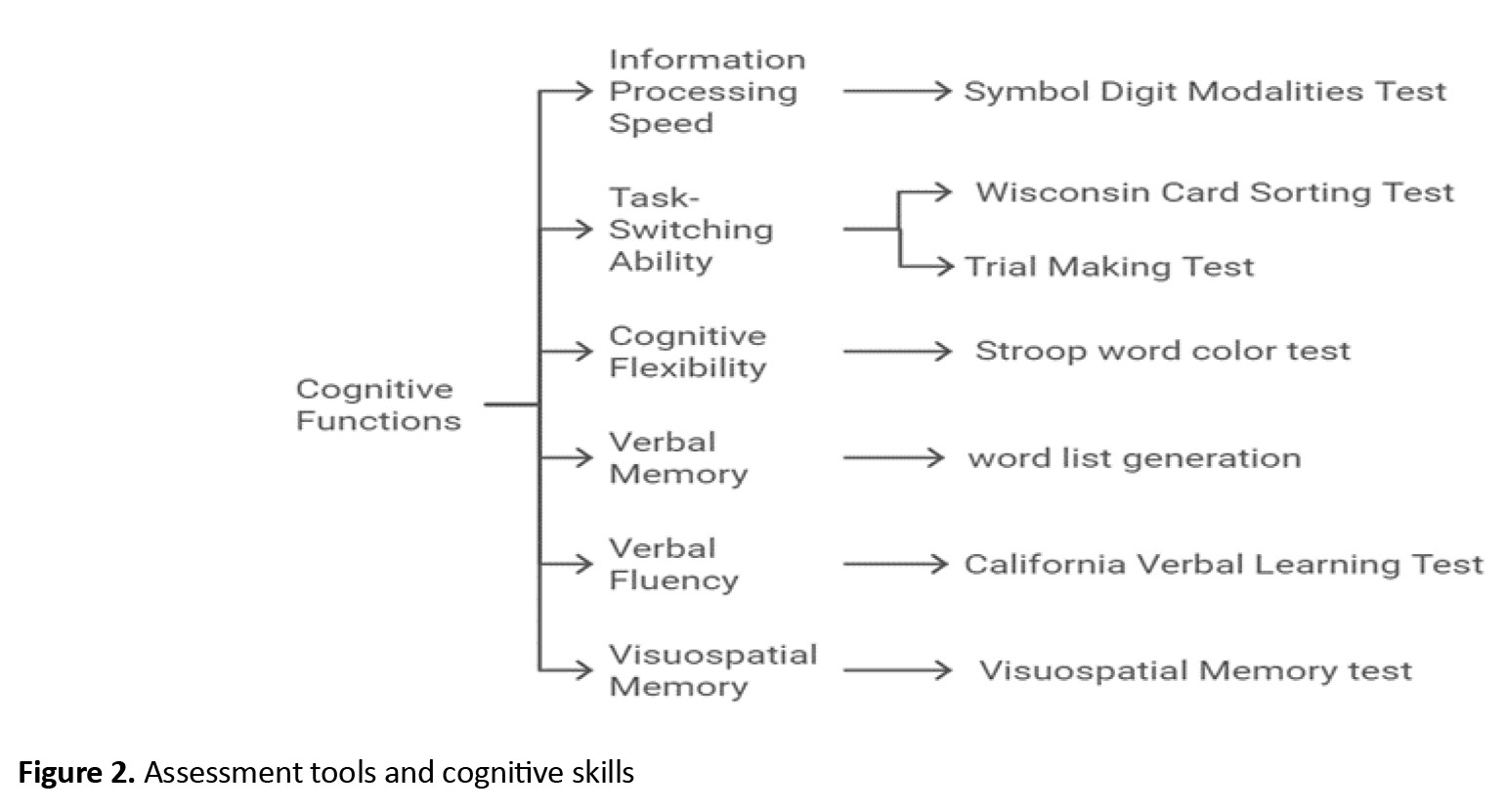
Symbol digit modalities test (SDMT) assesses information processing speed. The Stroop word-color test (SWCT) assesses information processing speed, cognitive flexibility, selective attention, and inhibitory control. Word list generation (WLG) assesses memory and verbal fluency. Trail making test (TMT) assesses cognitive-motor speed and task-switching ability. California verbal learning test (CVLT) assesses working memory and verbal memory. Wisconsin card sorting test (WCST) assesses task-switching ability. A brief visual memory test (VMT) assesses visuospatial memory. The computerized cognitive battery of tests assesses verbal and non-verbal memory, visuospatial processing, attention, information processing speed, executive function, and motor skills. Montreal cognitive assessment (MOCA) assesses short-term memory, visuospatial skills, abstraction, and orientation.
Information processing speed was assessed using the SDMT in five studies, where three studies found that information processing speed is related to fall risk in pwMS, one study reported no relationship, and another found that backward walking speed is related to fall risk but not dependent on information processing speed [13-17].
Task-switching ability was assessed using the WCST in one study [15] and the TMT in two studies [16, 18], all of which found a relationship with fall risk. Cognitive flexibility and inhibitory control were evaluated using the SWCT in one study, which found a relationship with fall risk [16]. Working memory and verbal memory were assessed using the CVLT in two studies, both of which found that working memory is related to fall risk [15, 17]. Verbal fluency, assessed using the WLG in two studies, had no relationship with fall risk [14, 16]. Visuospatial memory, assessed using the VMT in three studies, was reported in two studies to be related to backward walking speed, which in turn is related to fall risk. However, one study found that visuospatial memory affects backward walking speed but not its relationship with fall risk [13, 14, 17]. The MOCA assessment tool in one study also reported a relationship between visuospatial memory and fall risk [19]. In one study, various cognitive factors were assessed using the computerized cognitive battery of tests, revealing that all cognitive skills differ between pwMS with and without a history of falls. However, no significant difference was observed in visuospatial processing and memory. Balance problems in pwMS with a history of falls were associated with verbal fluency, attention and working memory [20].
Cognitive performance becomes more pronounced during dual-task activities. Based on this, two studies have indicated that during dual-task activities, it is easier to predict the risk of falls in pwMS. The more cognitively demanding the dual-task, the more accurate the assessment of the patient’s performance to assess and predict the risk of falling. However, it was stated in a study that dual-task evaluation cannot predict the risk of falling [16, 21-24]. The greater severity of the disease, the more significant the cognitive issues in pwMS [17] and in three studies, the results show a correlation between disease severity and the risk of falling [15, 18].
Discussion
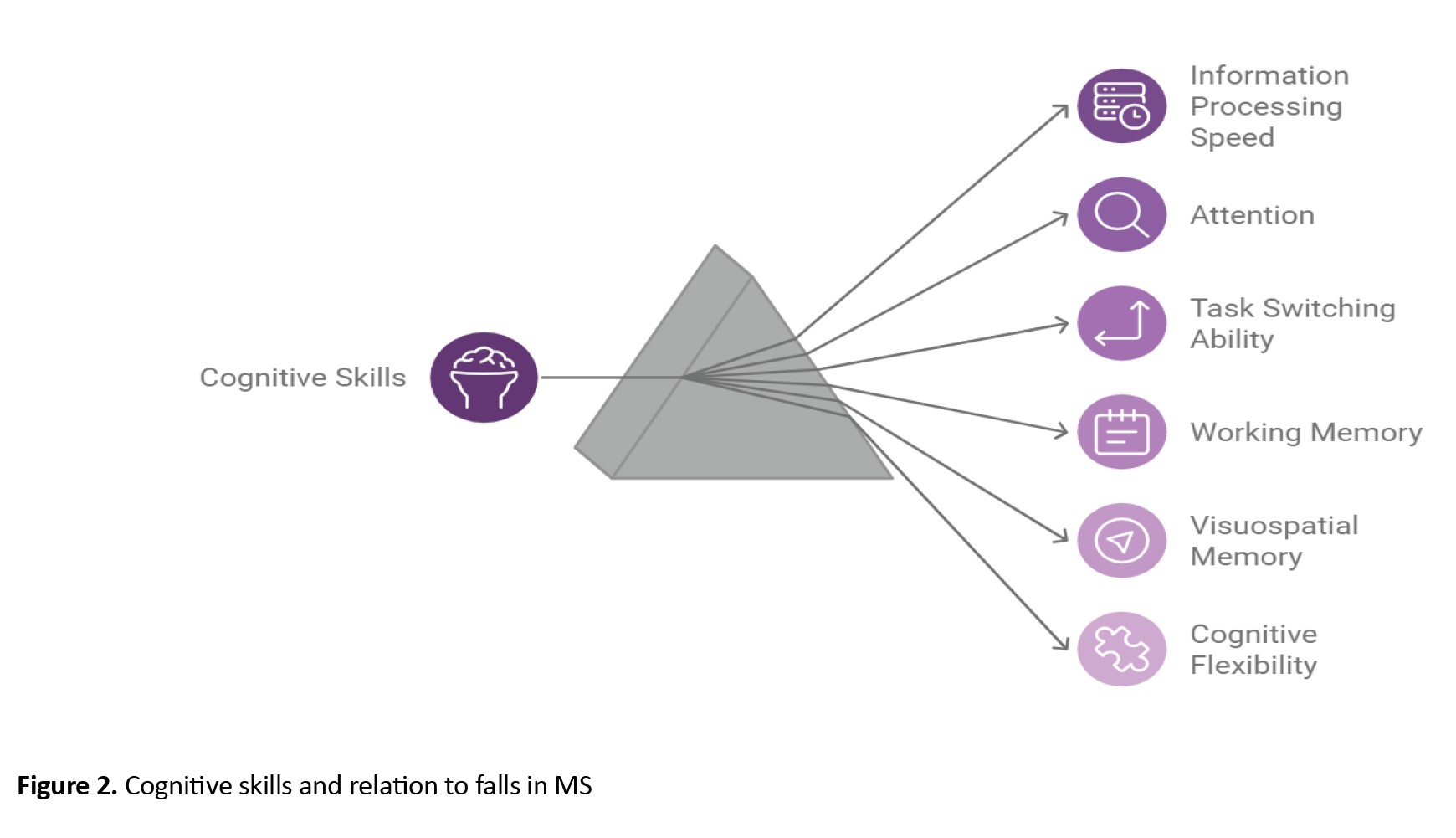
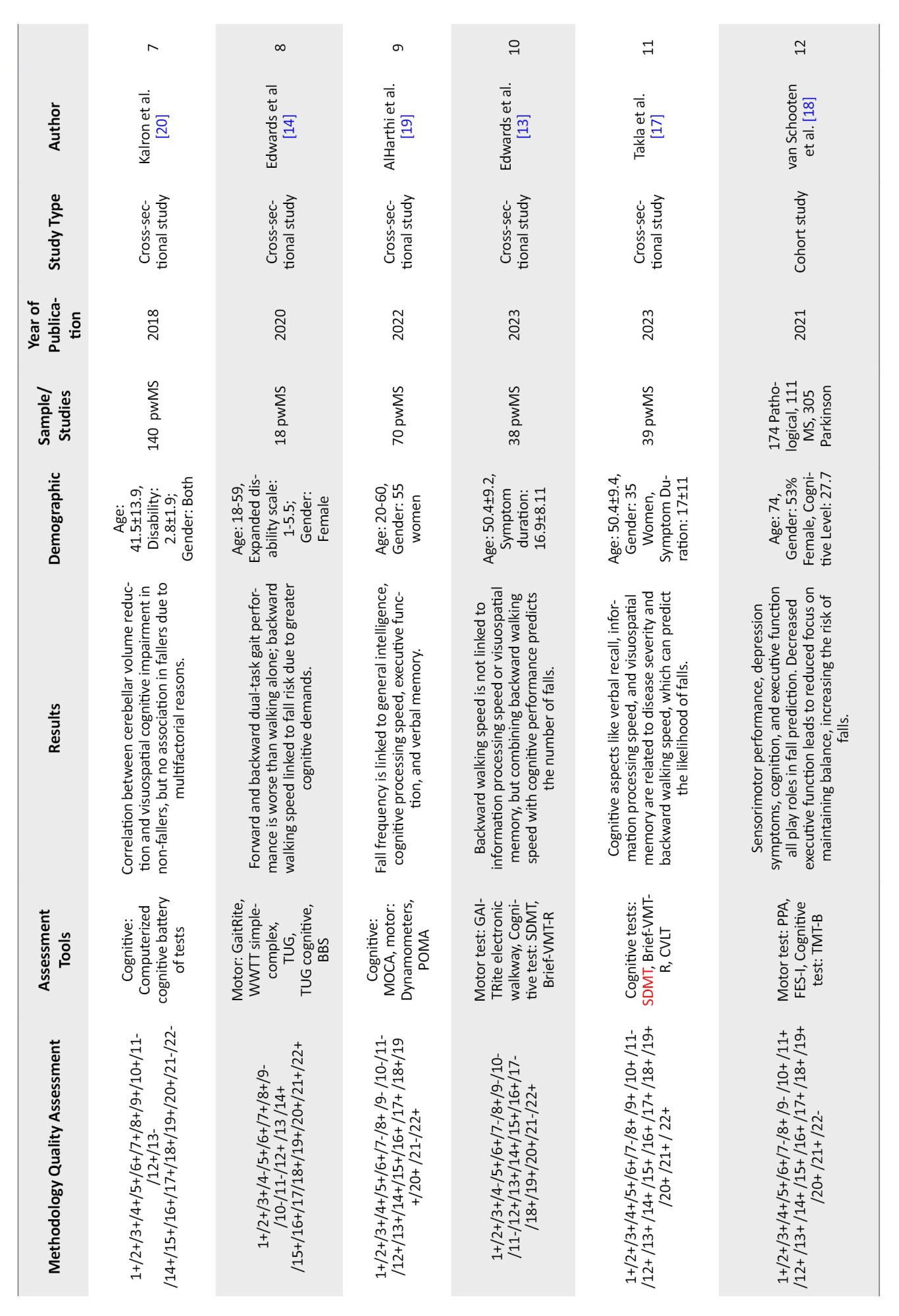
This study was conducted to investigate the relationship between executive function, the risk of falling, and the accuracy of assessment tools that examine these cognitive skills. According to the reviewed studies, the cognitive skills that are impaired in pwMS and play a role in executive function, as well as being associated with the risk of falling, include information processing speed, the ability to switch between tasks, cognitive flexibility, response inhibition, working memory and visuospatial memory. The cognitive skills most strongly related to the risk of falling are information processing speed, attention, the ability to switch between tasks, and working memory. Additionally, since visuospatial memory affects the backward walking speed, it is also linked to the risk of falling. Cognitive flexibility, response inhibition, and verbal memory have less of a relationship with the risk of falling. Verbal fluency, one of the executive function cognitive skills, is not associated with the risk of falling (Figure 1). Each of these cognitive domains is assessed with greater precision by specific assessment tools, as follows: Information processing speed by the SDMT, task-switching ability by the WCST and TMT, cognitive flexibility by the SWCT, verbal memory and verbal fluency by the WLG and CVLT and visuospatial memory by the VMT (Figure 2).
Full-Text: (538 Views)
Introduction
Multiple sclerosis (MS) is a progressive inflammatory disease of the central nervous system that affects the brain, spinal cord and optic nerves. The prevalence of this disease exceeds 2.5 million people worldwide, with a higher incidence in women compared to men. MS is typically diagnosed between the ages of 20 and 50 and both genetic and environmental factors play a role in its development. Environmental factors include geographical location, vitamin D deficiency, smoking, obesity, and infections [1].
The types of MS are as follows: Relapsing-remitting MS (RRMS): About 85% of individuals begin with this type. The duration of relapses can range from days to months, followed by complete or nearly complete recovery of function. Between attacks, the disease does not progress, and relapses usually occur one to two times a year.
Secondary progressive MS: This type occurs in nearly 90% of persons with MS (pwMS) with RRMS about fifteen years after diagnosis, following a change in the disease type. Initially, relapses are observed, but subsequently, no further relapses occur, although the patient’s disability progresses over time.
Primary progressive MS: About 10-15% of individuals have this type. There are no distinct relapses, and symptoms progress gradually and continuously. pwMS are diagnosed later (in their late 30s to early 40s) and respond less to medications [1].
Radiological isolated syndrome: MRI shows signs of MS, but no clinical symptoms. There is about a one-third probability of developing MS within five years for these individuals [1].
The pathological manifestations of MS vary depending on the location of lesions in the central nervous system, making individuals susceptible to motor, sensory and cognitive impairments [2]. For example, when lesions are present in the optic nerve, the patient may experience painful vision loss, and when lesions occur in the spinal cord, symptoms such as hemiparesis, paresthesia and sphincter dysfunction can be observed [3]. Furthermore, studies have shown a connection between the cerebellum and balance, gait and cognition in these individuals, with changes in cerebellar volume associated with cognitive disorders [4].
Falls are a common issue among pwMS, with approximately 56% of them falling in three months [2]. Postural imbalance, a significant fall risk factor, is observed in 75% of pwMS [5] and impairments in proprioception and cognitive dysfunctions are related to their balance and fall risk [6]. Multifactorial fall risk factors include individual factors, such as poor balance, muscle weakness, fatigue, and pain; environmental factors, such as surface conditions and distraction factors, and activity-related factors, such as hurry to complete tasks or multitasking [7]. These factors have been examined using myelin water imaging, revealing that the volume of corticospinal tracts and superior cerebellar peduncles is associated with fall risk [8]. Long-term negative effects of falls in pwMS include fear of falling, reduced activities, and decreased social participation [5].
Cognition can be described as “the mental act or process of acquiring knowledge and understanding through thought, experience, and the senses.” Various cognitive domains in MS are affected to differing degrees. The vulnerable cognitive domains in MS include information processing speed, memory, executive function, visuospatial processing, language function, and social cognition. Most pwMS primarily struggle with information processing speed, memory, and learning, while facing fewer issues with executive function and visuospatial processing. The impact of cognitive impairments can be observed in various aspects of pwMS’ lives, including quality of life, disease management, safety (fall risk and driving), financial matters, employment and social participation [9].
Several key components of executive function may predict fall risk, including difficulties in response inhibition, attention, and switching under timed conditions, which are problematic for pwMS. Thus, the relationship between cognitive performance and fall risk in pwMS can be inferred [10]. Previous studies have not examined the connection between each cognitive skill and fall risk, nor have they assessed cognitive assessment tools that provide greater accuracy in expressing this relationship. This review was conducted to explore the relationship between cognitive skills involved in executive function and fall risk in pwMS and to examine cognitive assessment tools that more accurately express this relationship.
Materials and Methods
Search strategy
In this study, research conducted on the relationship between cognitive function, executive function, and the likelihood of falls in pwMS was reviewed from 2015 to 2024 across databases, including Google Scholar, PubMed and Science Direct. The relationship between MS, cognition and the risk of falling was investigated, and 58 studies were selected based on their titles. Then, the abstracts and full texts of the studies were reviewed, and the following studies were excluded, 13 studies due to duplication, 1 study because it focused on pwMS with psychiatric disorder, 15 studies for not examining the relationship between cognition and fall risk, considering only one of these variables about MS, 2 studies for not involving only pwMS, 6 studies as they were already included in previous review studies, 6 studies that examined only the relationship between dual-task activities and either cognitive status or fall risk and 3 studies due to lack of access to their full texts. Finally, 12 studies were included in the analysis (Figure 1).
Multiple sclerosis (MS) is a progressive inflammatory disease of the central nervous system that affects the brain, spinal cord and optic nerves. The prevalence of this disease exceeds 2.5 million people worldwide, with a higher incidence in women compared to men. MS is typically diagnosed between the ages of 20 and 50 and both genetic and environmental factors play a role in its development. Environmental factors include geographical location, vitamin D deficiency, smoking, obesity, and infections [1].
The types of MS are as follows: Relapsing-remitting MS (RRMS): About 85% of individuals begin with this type. The duration of relapses can range from days to months, followed by complete or nearly complete recovery of function. Between attacks, the disease does not progress, and relapses usually occur one to two times a year.
Secondary progressive MS: This type occurs in nearly 90% of persons with MS (pwMS) with RRMS about fifteen years after diagnosis, following a change in the disease type. Initially, relapses are observed, but subsequently, no further relapses occur, although the patient’s disability progresses over time.
Primary progressive MS: About 10-15% of individuals have this type. There are no distinct relapses, and symptoms progress gradually and continuously. pwMS are diagnosed later (in their late 30s to early 40s) and respond less to medications [1].
Radiological isolated syndrome: MRI shows signs of MS, but no clinical symptoms. There is about a one-third probability of developing MS within five years for these individuals [1].
The pathological manifestations of MS vary depending on the location of lesions in the central nervous system, making individuals susceptible to motor, sensory and cognitive impairments [2]. For example, when lesions are present in the optic nerve, the patient may experience painful vision loss, and when lesions occur in the spinal cord, symptoms such as hemiparesis, paresthesia and sphincter dysfunction can be observed [3]. Furthermore, studies have shown a connection between the cerebellum and balance, gait and cognition in these individuals, with changes in cerebellar volume associated with cognitive disorders [4].
Falls are a common issue among pwMS, with approximately 56% of them falling in three months [2]. Postural imbalance, a significant fall risk factor, is observed in 75% of pwMS [5] and impairments in proprioception and cognitive dysfunctions are related to their balance and fall risk [6]. Multifactorial fall risk factors include individual factors, such as poor balance, muscle weakness, fatigue, and pain; environmental factors, such as surface conditions and distraction factors, and activity-related factors, such as hurry to complete tasks or multitasking [7]. These factors have been examined using myelin water imaging, revealing that the volume of corticospinal tracts and superior cerebellar peduncles is associated with fall risk [8]. Long-term negative effects of falls in pwMS include fear of falling, reduced activities, and decreased social participation [5].
Cognition can be described as “the mental act or process of acquiring knowledge and understanding through thought, experience, and the senses.” Various cognitive domains in MS are affected to differing degrees. The vulnerable cognitive domains in MS include information processing speed, memory, executive function, visuospatial processing, language function, and social cognition. Most pwMS primarily struggle with information processing speed, memory, and learning, while facing fewer issues with executive function and visuospatial processing. The impact of cognitive impairments can be observed in various aspects of pwMS’ lives, including quality of life, disease management, safety (fall risk and driving), financial matters, employment and social participation [9].
Several key components of executive function may predict fall risk, including difficulties in response inhibition, attention, and switching under timed conditions, which are problematic for pwMS. Thus, the relationship between cognitive performance and fall risk in pwMS can be inferred [10]. Previous studies have not examined the connection between each cognitive skill and fall risk, nor have they assessed cognitive assessment tools that provide greater accuracy in expressing this relationship. This review was conducted to explore the relationship between cognitive skills involved in executive function and fall risk in pwMS and to examine cognitive assessment tools that more accurately express this relationship.
Materials and Methods
Search strategy
In this study, research conducted on the relationship between cognitive function, executive function, and the likelihood of falls in pwMS was reviewed from 2015 to 2024 across databases, including Google Scholar, PubMed and Science Direct. The relationship between MS, cognition and the risk of falling was investigated, and 58 studies were selected based on their titles. Then, the abstracts and full texts of the studies were reviewed, and the following studies were excluded, 13 studies due to duplication, 1 study because it focused on pwMS with psychiatric disorder, 15 studies for not examining the relationship between cognition and fall risk, considering only one of these variables about MS, 2 studies for not involving only pwMS, 6 studies as they were already included in previous review studies, 6 studies that examined only the relationship between dual-task activities and either cognitive status or fall risk and 3 studies due to lack of access to their full texts. Finally, 12 studies were included in the analysis (Figure 1).
Selection criteria
The author screened all studies for inclusion in this review. Relevant studies were selected based on their titles, abstracts, and when additional information was required, based on their full texts.
Inclusion criteria
The inclusion criteria for this study were as follows:
Studies that assessed the relationship between cognitive function and fall risk in pwMS.
Studies whose outcomes were related to fall risk and cognition in pwMS.
Studies in which the participants had a confirmed diagnosis of Multiple Sclerosis.
Studies with full-text access.
Exclusion criteria
The exclusion criteria for this study, based on which irrelevant studies were excluded, included:
Studies that examined only one variable (fall risk or cognitive/executive function) about MS. Studies that focused on pwMS with comorbid psychological disorders. Studies that did not assess the effect of rehabilitation interventions on both fall risk and executive performance. Duplicate studies already included in previous review studies.
Quality assessment of methodology
The quality of the reviewed studies and clinical trials included in this research was assessed using the CASP checklist, which covers various aspects also evaluated by other checklists. Cross-sectional and cohort studies were evaluated with the STROBE checklist, which comprehensively assesses the strengths, weaknesses, and generalizability of these studies [11, 12]. These checklists evaluate the studies based on their methodology and determine how statistically reliable their results are for decision-making.
Data extraction
The author extracted demographic information of the pwMS from the included studies, such as age, gender, and cognitive level. Additionally, the study results and the number of pwMS in each study were extracted.
Results
Literature search and methodology quality assessment
At the beginning of the search, 58 studies were identified based on their titles. After applying the inclusion and exclusion criteria, 12 studies were selected, and the other studies were excluded due to not meeting the inclusion criteria. Table 1 presents the quality of the included studies and the extracted data from each study.
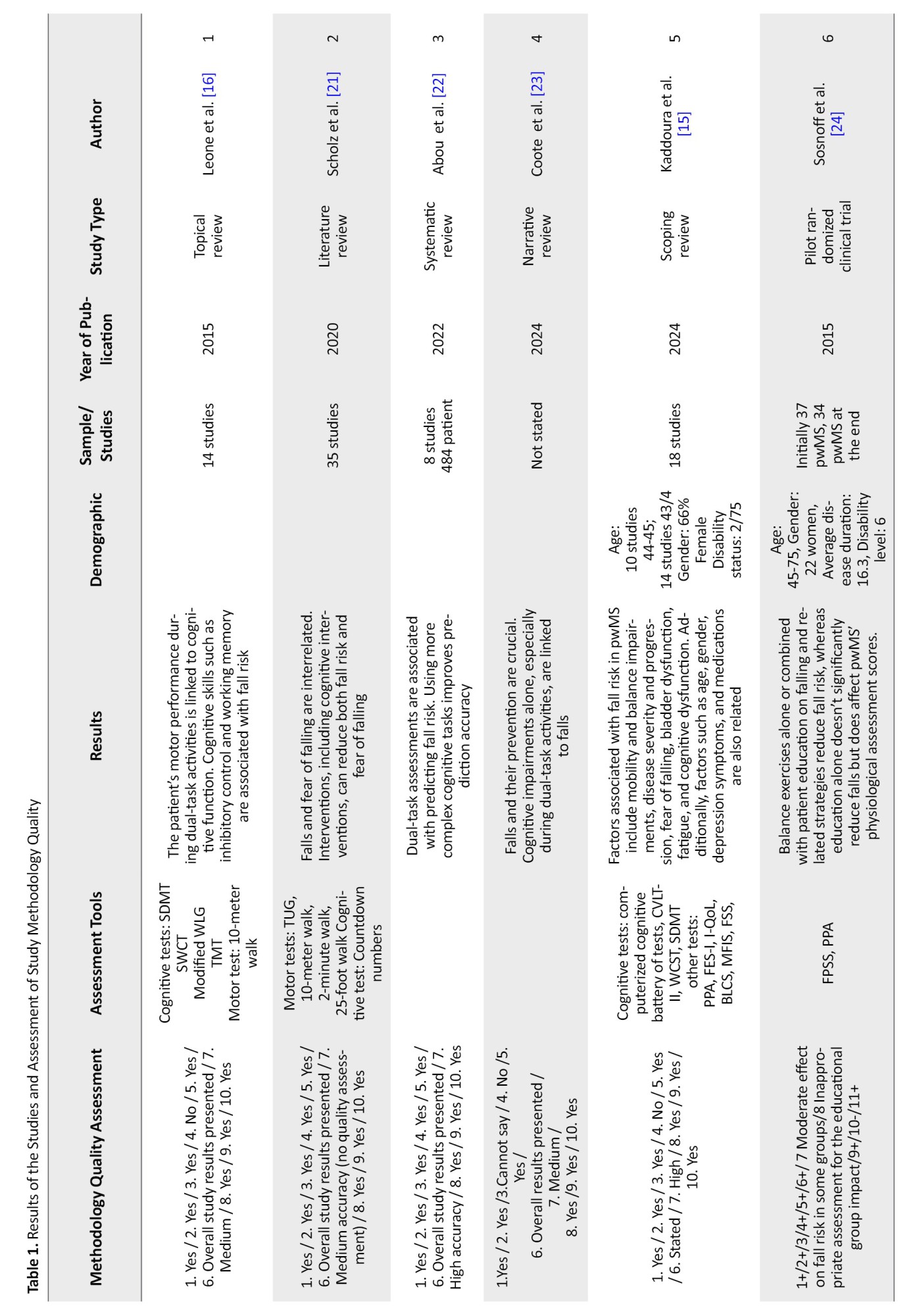
Executive function encompasses various cognitive skills, such as attention, planning, working memory, organization, cognitive flexibility, inhibition, problem-solving, and more. The assessment tools used in the reviewed studies to evaluate executive function include:
Symbol digit modalities test (SDMT) assesses information processing speed. The Stroop word-color test (SWCT) assesses information processing speed, cognitive flexibility, selective attention, and inhibitory control. Word list generation (WLG) assesses memory and verbal fluency. Trail making test (TMT) assesses cognitive-motor speed and task-switching ability. California verbal learning test (CVLT) assesses working memory and verbal memory. Wisconsin card sorting test (WCST) assesses task-switching ability. A brief visual memory test (VMT) assesses visuospatial memory. The computerized cognitive battery of tests assesses verbal and non-verbal memory, visuospatial processing, attention, information processing speed, executive function, and motor skills. Montreal cognitive assessment (MOCA) assesses short-term memory, visuospatial skills, abstraction, and orientation.
Information processing speed was assessed using the SDMT in five studies, where three studies found that information processing speed is related to fall risk in pwMS, one study reported no relationship, and another found that backward walking speed is related to fall risk but not dependent on information processing speed [13-17].
Task-switching ability was assessed using the WCST in one study [15] and the TMT in two studies [16, 18], all of which found a relationship with fall risk. Cognitive flexibility and inhibitory control were evaluated using the SWCT in one study, which found a relationship with fall risk [16]. Working memory and verbal memory were assessed using the CVLT in two studies, both of which found that working memory is related to fall risk [15, 17]. Verbal fluency, assessed using the WLG in two studies, had no relationship with fall risk [14, 16]. Visuospatial memory, assessed using the VMT in three studies, was reported in two studies to be related to backward walking speed, which in turn is related to fall risk. However, one study found that visuospatial memory affects backward walking speed but not its relationship with fall risk [13, 14, 17]. The MOCA assessment tool in one study also reported a relationship between visuospatial memory and fall risk [19]. In one study, various cognitive factors were assessed using the computerized cognitive battery of tests, revealing that all cognitive skills differ between pwMS with and without a history of falls. However, no significant difference was observed in visuospatial processing and memory. Balance problems in pwMS with a history of falls were associated with verbal fluency, attention and working memory [20].
Cognitive performance becomes more pronounced during dual-task activities. Based on this, two studies have indicated that during dual-task activities, it is easier to predict the risk of falls in pwMS. The more cognitively demanding the dual-task, the more accurate the assessment of the patient’s performance to assess and predict the risk of falling. However, it was stated in a study that dual-task evaluation cannot predict the risk of falling [16, 21-24]. The greater severity of the disease, the more significant the cognitive issues in pwMS [17] and in three studies, the results show a correlation between disease severity and the risk of falling [15, 18].
Discussion
This study was conducted to investigate the relationship between executive function, the risk of falling, and the accuracy of assessment tools that examine these cognitive skills. According to the reviewed studies, the cognitive skills that are impaired in pwMS and play a role in executive function, as well as being associated with the risk of falling, include information processing speed, the ability to switch between tasks, cognitive flexibility, response inhibition, working memory and visuospatial memory. The cognitive skills most strongly related to the risk of falling are information processing speed, attention, the ability to switch between tasks, and working memory. Additionally, since visuospatial memory affects the backward walking speed, it is also linked to the risk of falling. Cognitive flexibility, response inhibition, and verbal memory have less of a relationship with the risk of falling. Verbal fluency, one of the executive function cognitive skills, is not associated with the risk of falling (Figure 1). Each of these cognitive domains is assessed with greater precision by specific assessment tools, as follows: Information processing speed by the SDMT, task-switching ability by the WCST and TMT, cognitive flexibility by the SWCT, verbal memory and verbal fluency by the WLG and CVLT and visuospatial memory by the VMT (Figure 2).
The severity of the disease and the number of relapses experienced by the pwMS are significant factors influencing the extent of cognitive problems faced by these individuals. The greater the severity of the disease and the number of relapses, the more observable cognitive issues are present. Given that cognition is related to balance and the likelihood of falling, an increase in disease severity and cognitive problems also heightens the risk of falls. Therefore, assessing and providing appropriate interventions for the cognitive skills and executive functioning of pwMS can impact their likelihood of falling. Since falling is one of the common issues and complaints among pwMS and can lead to secondary problems, such as decreased participation, one of the main goals of occupational therapy is to promote occupational justice and facilitate the individual’s participation in meaningful and valuable occupations to enhance their health and well-being so it is recommended that occupational therapists consider cognitive issues in addition to balance when evaluating and providing interventions tailored to the patient’s condition.
The cognitive tests examined in this study for their accuracy in assessing cognitive problems to predict the risk of falling include SDMT, SWCT, WLG, TMT, CVLT, WCST, VMT, and MOCA. SDMT has been widely used in studies and has demonstrated a relationship between executive function and the likelihood of falling, indicating its high accuracy in assessing executive function and predicting fall risk. SWCT, TMT, and CVLT have also been utilized, with their results confirming findings from various studies; thus, these tests possess the necessary accuracy for evaluating executive function and predicting fall risk. VMT shows the relationship between visuospatial memory and backward walking speed, which is effective in predicting the risk of falling. Therefore, this test does not directly indicate the relationship between executive function and fall risk. The computerized cognitive battery of tests has not demonstrated a relationship between visuospatial memory and fall risk, while MOCA has explicitly stated the relationship between visuospatial memory and the risk of falling so according to this point to the lower accuracy of MOCA in assessing executive function and predicting fall risk (Figure 3).
The cognitive tests examined in this study for their accuracy in assessing cognitive problems to predict the risk of falling include SDMT, SWCT, WLG, TMT, CVLT, WCST, VMT, and MOCA. SDMT has been widely used in studies and has demonstrated a relationship between executive function and the likelihood of falling, indicating its high accuracy in assessing executive function and predicting fall risk. SWCT, TMT, and CVLT have also been utilized, with their results confirming findings from various studies; thus, these tests possess the necessary accuracy for evaluating executive function and predicting fall risk. VMT shows the relationship between visuospatial memory and backward walking speed, which is effective in predicting the risk of falling. Therefore, this test does not directly indicate the relationship between executive function and fall risk. The computerized cognitive battery of tests has not demonstrated a relationship between visuospatial memory and fall risk, while MOCA has explicitly stated the relationship between visuospatial memory and the risk of falling so according to this point to the lower accuracy of MOCA in assessing executive function and predicting fall risk (Figure 3).
This review study delineates the relationship between executive function and cognitive skills with fall risk, as well as the accuracy of various cognitive assessments in measuring executive function and predicting fall risk in pwMS. However, this study had limitations, including the unavailability of the full text of certain studies that may have provided useful results, and the diversity in the methodology of the reviewed studies, which may introduce bias in interpreting the results. Therefore, cross-sectional studies and clinical trials with larger sample sizes are needed for future investigations to provide more definitive conclusions.
Conclusion
In this review study, we concluded that a relationship is observed between executive function and cognitive skills with the risk of falling in pwMS. The greater the cognitive problems in pwMS and the weaker their executive function, the higher the risk of falling in these individuals. Therefore, it is essential to assess executive function in these persons using tests that have greater accuracy for evaluating executive function and predicting fall risk, as well as interventions aimed at improving executive function.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization: Ashkan Irani and Negar Balali; Supervision: Ashkan Irani and Mansoor Rayegani; Data collection and analysis: Negar Balali and Ashkan Irani; Writing the initial draft: Negar Balali and Ashkan Irani; Revision and editing: All authors.
Conflict of interest
The authors declare no conflict of interest.
References
Conclusion
In this review study, we concluded that a relationship is observed between executive function and cognitive skills with the risk of falling in pwMS. The greater the cognitive problems in pwMS and the weaker their executive function, the higher the risk of falling in these individuals. Therefore, it is essential to assess executive function in these persons using tests that have greater accuracy for evaluating executive function and predicting fall risk, as well as interventions aimed at improving executive function.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization: Ashkan Irani and Negar Balali; Supervision: Ashkan Irani and Mansoor Rayegani; Data collection and analysis: Negar Balali and Ashkan Irani; Writing the initial draft: Negar Balali and Ashkan Irani; Revision and editing: All authors.
Conflict of interest
The authors declare no conflict of interest.
References
- Lazaro RT, Reina-Guerra SG, Quiben M. Umphred’s neurological rehabilitation. Amsterdam: Elsevier Health Sciences; 2019. [Link]
- Comber L, Sosnoff JJ, Galvin R, Coote S. Postural control deficits in people with multiple sclerosis: A systematic review and meta-analysis. Gait Posture. 2018; 61:445-52. [DOI:10.1016/j.gaitpost.2018.02.018] [PMID]
- Oh J, Vidal-Jordana A, Montalban X. Multiple sclerosis: Clinical aspects. Curr Opin Neurol. 2018; 31(6):752-9. [DOI:10.1097/WCO.0000000000000622] [PMID]
- Eskut N, Koc AM, Köskderelioglu A, Unsal Bilgin YO, Tekindal MA. Is there a relationship between fall status, cognition and cerebellar lobule volume in patients with multiple sclerosis? Appl Neuropsychol Adult. 2023; 30(5):535-45. [DOI:10.1080/23279095.2021.1962881] [PMID]
- To-Alemanji J. Role of cognitive motor interference as a fall risk among adults with relapsing-remitting multiple sclerosis [PhD dissertation]. Virginia: George Mason University; 2018. [Link]
- Henning DA, Huisinga JM, Lynch S, Fritz NE. Cognition and proprioception in persons with multiple sclerosis and healthy controls: Nascent findings. Mult Scler Relat Disord. 2022; 68:104372.[DOI:10.1016/j.msard.2022.104372] [PMID]
- Abou L, McCloskey C, Wernimont C, Fritz NE, Kratz AL. Examination of risk factors associated with falls and injurious falls in people with multiple sclerosis: An updated nationwide study. Arch Phys Med Rehabil. 2024; 105(4):717-24. [DOI:10.1016/j.apmr.2023.11.011] [PMID]
- Edwards EM, Stanley JA, Daugherty AM, Lynn J, Borich MR, Fritz NE. Associations between myelin water imaging and measures of fall risk and functional mobility in multiple sclerosis. J Neuroimaging. 2023; 33(1):94-101. [DOI:10.1111/jon.13064] [PMID]
- Langdon D, Young C. Cognition in multiple sclerosis. Karger Publishers Ltd; 2023. [Link]
- Saverino A, Waller D, Rantell K, Parry R, Moriarty A, Playford ED. The role of cognitive factors in predicting balance and fall risk in a neuro-rehabilitation setting. Plos One. 2016; 11(4):e0153469. [DOI:10.1371/journal.pone.0153469] [PMID]
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet. 2007; 370(9596):1453-7. [DOI:10.1016/S0140-6736(07)61602-X] [PMID]
- Zeng X, Zhang Y, Kwong JS, Zhang C, Li S, Sun F, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta‐analysis, and clinical practice guideline: A systematic review. J Evid Based Med. 2015; 8(1):2-10. [DOI:10.1111/jebm.12141]
- Edwards EM, Daugherty AM, Fritz NE. Examining the influence of cognition on the relationship between backward walking and falls in persons with multiple sclerosis. Int J MS Care. 2023; 25(2):51-5. [DOI:10.7224/1537-2073.2021-130] [PMID]
- Edwards EM, Kegelmeyer DA, Kloos AD, Nitta M, Raza D, Nichols-Larsen DS, et al. Backward walking and dual‐task assessment improve identification of gait impairments and fall risk in individuals with MS. Mult Scler Int. 2020; 2020:6707414. [DOI:10.1155/2020/6707414] [PMID]
- Kaddoura R, Faraji H, Othman M, Abu Hijleh A, Loney T, Goswami N, et al. Exploring factors associated with falls in multiple sclerosis: Insights from a scoping review. Clin Interv Aging. 2024; 19:923-38. [DOI:10.2147/CIA.S460475] [PMID]
- Leone C, Patti F, Feys P. Measuring the cost of cognitive-motor dual tasking during walking in multiple sclerosis. Mult Scler. 2015; 21(2):123-31. [DOI:10.1177/1352458514547408] [PMID]
- Takla TN, Chargo AN, Daugherty AM, Fritz NE. Cognitive contributors of backward walking in persons with multiple sclerosis. Mult Scler Int. 2023; 2023:5582242. [DOI:10.1155/2023/5582242] [PMID]
- van Schooten KS, Taylor ME, Close JC, Davis JC, Paul SS, Canning CG, et al. Sensorimotor, cognitive, and affective functions contribute to the prediction of falls in old age and neurologic disorders: An observational study. Arch Phys Med Rehabil. 2021; 102(5):874-80. [DOI:10.1016/j.apmr.2020.10.134] [PMID]
- AlHarthi H, Almurdi MM. Association between cognitive impairment and motor dysfunction among patients with multiple sclerosis [Unpublished]. 2022. [DOI:10.21203/rs.3.rs-2098782/v1]
- Kalron A, Allali G, Achiron A. Cerebellum and cognition in multiple sclerosis: The fall status matters. J Neurol. 2018; 265(4):809-16. [DOI:10.1007/s00415-018-8774-2] [PMID]
- Scholz M, Haase R, Trentzsch K, Weidemann ML, Ziemssen T. Fear of falling and falls in people with multiple sclerosis: A literature review. Mult Scler Relat Disord. 2021; 47:102609. [DOI:10.1016/j.msard.2020.102609] [PMID]
- Abou L, Peters J, Fritz NE, Sosnoff JJ, Kratz AL. Motor cognitive dual-task testing to predict future falls in multiple sclerosis: A systematic review. Neurorehabil Neural Repair. 2022; 36(12):757-69. [DOI:10.1177/15459683221131791] [PMID]
- Coote S, Comber L, Quinn G, Santoyo-Medina C, Kalron A, Gunn H. Falls in people with multiple sclerosis: Risk identification, intervention, and future directions. Int J MS Care. 2020; 22(6):247-55. [DOI:10.7224/1537-2073.2020-014] [PMID]
- Sosnoff JJ, Moon Y, Wajda DA, Finlayson ML, McAuley E, Peterson EW, et al. Fall risk and incidence reduction in high risk individuals with multiple sclerosis: A pilot randomized control trial. Clin Rehabil. 2015; 29(10):952-60. [DOI:10.1177/0269215514564899] [PMID]
Type of Study: Review Article |
Subject:
Occupational Therapy
Received: 2024/10/20 | Accepted: 2024/10/31 | Published: 2025/03/22
Received: 2024/10/20 | Accepted: 2024/10/31 | Published: 2025/03/22