Volume 7, Issue 1 (Continuously Updated 2024)
Func Disabil J 2024, 7(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shourvazi R, MirzaKhani N, Rahmanirasa A, Pashmdarfard M, Loabichian M. The Relationship Between Sensory Processing, Substance Abuse and Impulsivity With Suicide in Schizophrenia: A Narrative Review. Func Disabil J 2024; 7 (1)
URL: http://fdj.iums.ac.ir/article-1-260-en.html
URL: http://fdj.iums.ac.ir/article-1-260-en.html
Roya Shourvazi1 

 , Navid MirzaKhani2
, Navid MirzaKhani2 

 , Amir Rahmanirasa2
, Amir Rahmanirasa2 

 , Marzieh Pashmdarfard *3
, Marzieh Pashmdarfard *3 

 , Maedeh Loabichian1
, Maedeh Loabichian1 




 , Navid MirzaKhani2
, Navid MirzaKhani2 

 , Amir Rahmanirasa2
, Amir Rahmanirasa2 

 , Marzieh Pashmdarfard *3
, Marzieh Pashmdarfard *3 

 , Maedeh Loabichian1
, Maedeh Loabichian1 


1- Student Research Committee, Department of Occupational Therapy, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Department of Occupational Therapy, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
3- Department of Occupational Therapy, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran. ,mpashmdarfard@gmail.com
2- Department of Occupational Therapy, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
3- Department of Occupational Therapy, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 1069 kb]
(192 Downloads)
| Abstract (HTML) (739 Views)
Full-Text: (122 Views)
Introduction
Schizophrenia is known as a debilitating mental disorder with the appearance of various symptoms, such as delusions, hallucinations, disturbed speech or behavior and cognitive impairment. Its early onset, along with its chronic symptoms, makes it a disabling disorder for many patients and their families [1]. Schizophrenia affects approximately 1% of the population worldwide and typically the onset of the disease occurs early in life (usually in late adolescence or early adulthood). Most patients have long-term side effects [2].
The main reasons for this disorder are not well understood and a combination of genetic and environmental factors play a role in the emergence of this disease [1, 3]. Environmental factors include birth complications, such as oxygen deprivation [4] and prematurity [5]. Advanced paternal age can also contribute to the development of schizophrenia [6]. Other non-genetic factors associated with the onset of schizophrenia include trauma, social isolation, migration, city life and substance abuse [7].
The primary reason for death among people with schizophrenia spectrum disorders (SSD) is suicide. The rate of suicide attempts among individuals with psychotic disorders ranges from 10% to 50%. Approximately 40% to 79% of individuals with schizophrenia report suicidal ideation at least once during their illness [8]. Even in the early stages of schizophrenia, the suicide rate is 2.4%, and in the first five years of the illness, the suicide rate is 0.48% per year [9].
Various risk factors for suicide among individuals with schizophrenia have been identified. Being male, being Caucasian, younger age, having concurrent depression, history of suicide attempts and lack of social support are the most influential factors [10]. Additionally, the risk of suicide significantly increases in the presence of substance abuse or dependence [11].
Substance abuse is common among people with schizophrenia, particularly in men. Nearly 50% of individuals with schizophrenia have a comorbid substance use disorder (SUD) at some stage during their illness [2]. Substance abuse in schizophrenia is associated with worse outcomes, including severe psychotic symptoms and less treatment adherence [12].
Regarding substance abuse, most studies report an increased risk of suicide and aggression [9] and most individuals with schizophrenia suffer from comorbid conditions, including impulse control disorders [13]. Sensory processing is one of the basic brain functions that is impaired in individuals with schizophrenia and this impaired sensory processing is related to emotional regulation and symptoms, such as suicidal thoughts and hopelessness [14].
Sensory processing refers to the way the nervous system receives sensory signals and converts them into appropriate behavioral and motor responses [15]. The sensory processing pattern in patients with psychiatric disorders, including schizophrenia demonstrates lower levels of sensory registration, sensory avoidance and sensory sensitivity, as well as reduced sensory-seeking behavior [16].
According to the studies, substance abuse and impulsivity are related to each other and exacerbate each other [13, 17] and these two factors, along with altered sensory processing, have a vital effect on the incidence of suicide in patients with schizophrenia [14]. Most studies in the field of suicide in individuals with schizophrenia have investigated the relationship between demographic factors such as age, gender, etc. [9, 18]. Despite the high importance of the three components of substance abuse, impulsivity, and sensory processing in the incidence of suicide in schizophrenic patients, fewer studies have investigated the relationship between these components in the suicide of these patients and also the studies that have been conducted in this field provide contradictory information about the relationship between these factors and the suicide of individuals with schizophrenia.
On the other hand, due to the high rate of suicide in schizophrenic patients, more and more in-depth investigations in this field and further investigation of risk factors and their relationship to the occurrence of suicide can be effective in preventing suicide and helping to reduce its rate and increase the life expectancy of these patients.
Therefore, this study was conducted to review the relationship between three variables of sensory processing, substance abuse, and impulsivity with suicide in patients with schizophrenia.
Materials and Methods
The present study is a literature review conducted using a systematic search approach. The keywords listed in the Table 1 were searched in databases, such as PubMed, Web of Science, and Google Scholar from 2010 to 2024.

Results
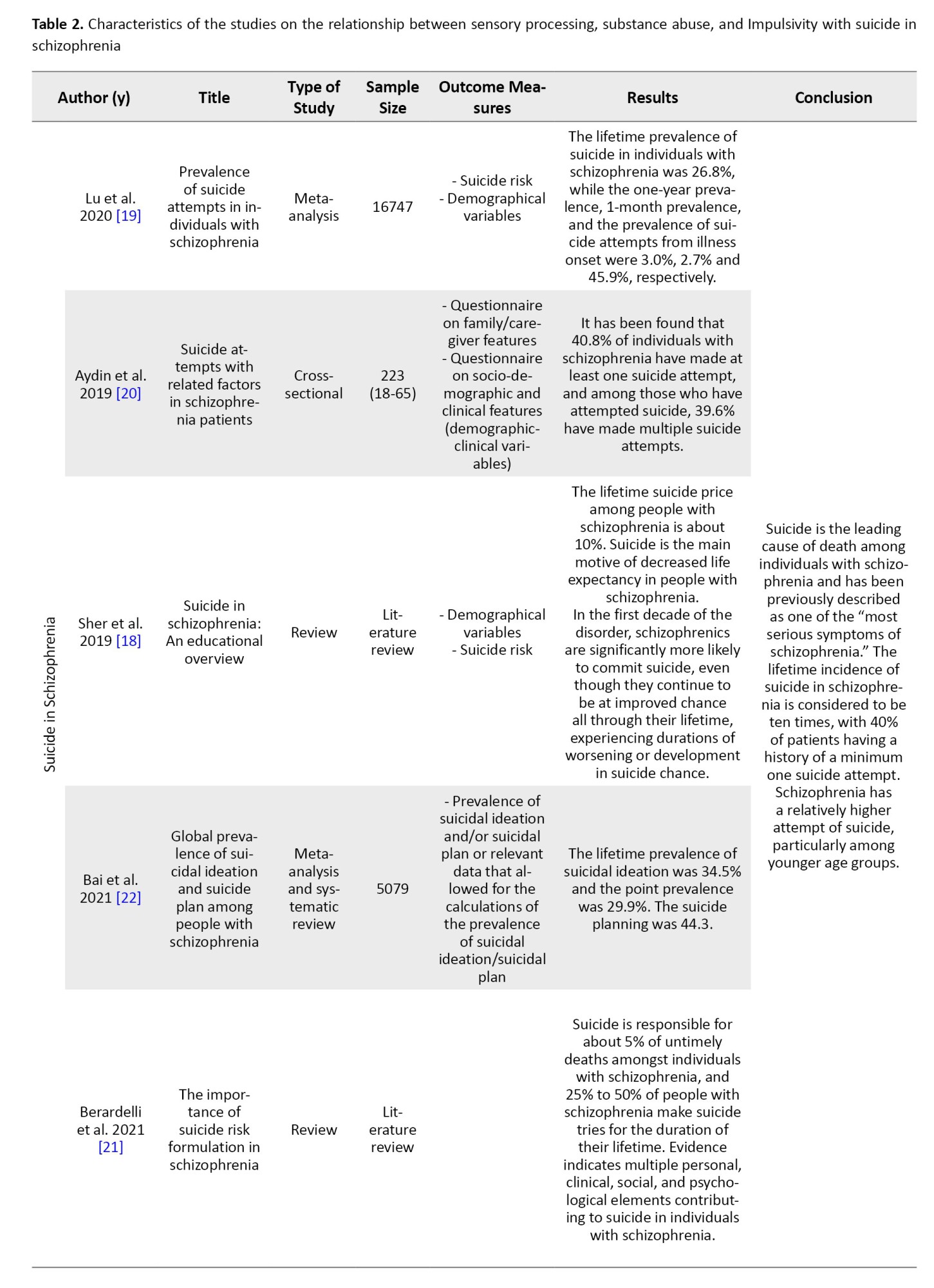
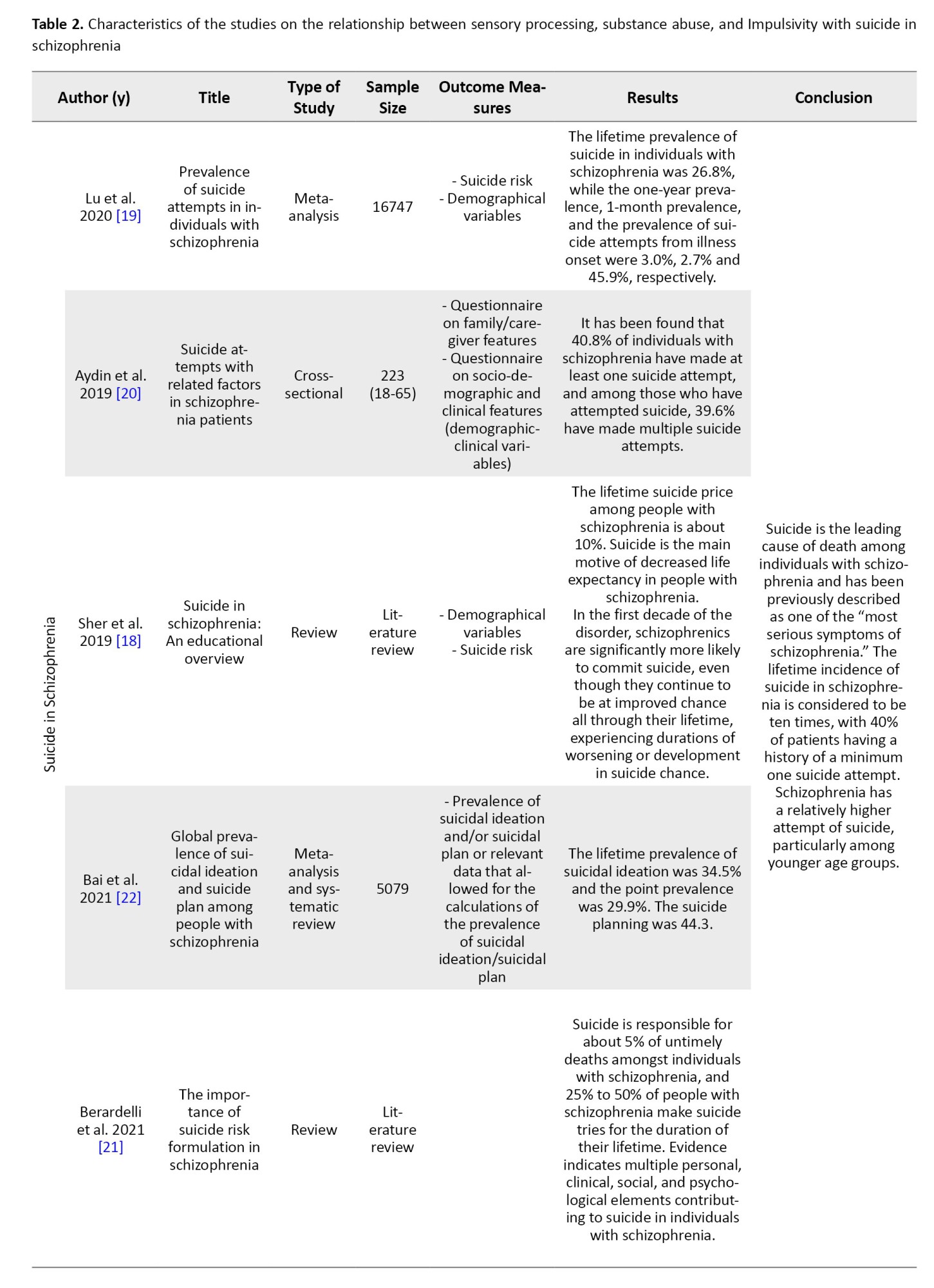
Using the keywords listed in Table 1, first, 372 articles were found after that 16 articles were identified as the most recent and relevant articles. These include 5 articles on suicide in schizophrenia, 3 articles on sensory processing in schizophrenia, 5 articles on substance abuse in schizophrenia and 3 articles on impulsivity and schizophrenia, as reported in Table 2.


Discussion
This study includes the results of 16 articles published from 2010 to 2022. The main results of this review are as follows:
The suicide rate in schizophrenia is significantly higher than in the population. Various studies report different incidences of suicide in schizophrenia. In a comprehensive review conducted by Lu et al. [19] in 2020, the lifetime suicide rate was reported to be 26.8%. However, another study conducted by Aydin et al. [20] in 2019 reported a much higher suicide rate among these patients. In this study, it was mentioned that at least 40.8% of individuals with schizophrenia attempted and 39.6% of these individuals attempted suicide repeatedly. Different studies, using different populations and methodologies, provide different estimates of suicide rates in schizophrenia. The population size in the first study was much larger than in the second study, and the significant difference in the reported prevalence of suicide may be due to this reason. The first study appears to provide a more accurate statistical estimate due to a more extensive investigation.
In two other studies conducted in 2021, Berardelli et al. [21] also reported the suicide attempt rate among individuals with schizophrenia to be between 25% and 50%, while Bai et al. [22] 34.5% of these patients had suicidal thoughts and 44.3% of planned suicides, which is consistent with the above studies.
In 2019, the suicide rate in individuals with schizophrenia was reported to be 10% [18]. This rate significantly differs from the prevalence reported in other studies, indicating a potential increase in suicide rates among these patients over time.
Despite the varying prevalence rates mentioned, all of these studies indicate that suicide is the most significant factor in reducing hope for life and the main cause of mortality in individuals with schizophrenia, emphasizing the need for careful examination. Furthermore, individuals who attempt suicide tend to have more severe symptoms.
Therefore, suicide in schizophrenia is a serious and highly prevalent issue, with its rates increasing over time. By addressing the risk factors and factors associated with suicide, it is possible to reduce its occurrence in these patients.
Sensory processing in schizophrenia
Sensory processing and its patterns in schizophrenia have been the subject of studies that have demonstrated significant sensory differences compared to healthy individuals. In studies conducted by van den Boogert et al. in 2022 [16], Halperin et al. [23] and Zhou et al. [24] in 2020, it was shown that sensory processing is compromised in individuals with schizophrenia, and sensory avoiding and sensory sensitivity patterns are observed to a greater extent than in healthy individuals. The low registration pattern is significantly more prevalent in these patients compared to the healthy group, while sensory seeking is less common.
Halperin et al. [23] also addressed in their study that sensory processing difficulties can have a significant impact on daily functioning, social performance and quality of life. These studies also indicated a significant relationship between sensory processing problems and psychiatric symptoms.
Therefore, the multiple sensory processing difficulties in these patients can have highly detrimental effects on their lives, including reduced quality of life, diminished functional capacity, and increased hopelessness. Consequently, due to the high prevalence of sensory processing problems in schizophrenia and their impact on the lives of these patients, studying these issues is of utmost importance.
Substance abuse in schizophrenia
The comorbidity of substance abuse is highly common. Hunt et al. [25] reported an occurrence rate of substance abuse in schizophrenia at 41.7%. Kelkar et al. [26] reported a prevalence rate of 48%. Both studies also noted that substance abuse is significantly more prevalent in men with schizophrenia than in women.
Chaudhury et al. [27] showed that substance abuse was recognized as a critical risk factor for schizophrenia. It was also stated that substance abuse precedes schizophrenia in over 60% of cases, and in most instances, both occurrences happen within a month, suggesting a potential causal connection between substance abuse and schizophrenia.
According to the results of studies, substance abuse can have detrimental effects on the course of schizophrenia. Hunt et al. [25] and Kelkar et al. [26] indicated that substance abuse can lead to an earlier onset of schizophrenia, exacerbate negative and positive symptoms, and prolong the duration of the illness.
Studies have also demonstrated that substance abuse can lead to increased self-harm and mortality rates in individuals with schizophrenia. Güney et al. [28] stated in their study that substance abuse can increase self-harm by four times in patients with schizophrenia, making it a significant predictor of self-harm in these individuals. Another study conducted by Lähteenvuo et al. [29] found that substance abuse leads to a 50% to 100% increase in hospitalizations and mortality in schizophrenia.
The prevalence of substance abuse in schizophrenia is increasing over time, likely due to easier access to drugs and the higher inclination of people with schizophrenia towards substance use. The comorbidity of substance abuse and schizophrenia worsens the prognosis for these patients and is considered a major risk factor for suicide in this population.
Impulsivity in Schizophrenia
The study results of Ouzir et al. [17], Sehgal and Patil [30] and Iancu et al. [31] have indicated that impulsivity in schizophrenia is associated with increased suicide and self-harm.
Ouzir et al. [17] also stated that impulsivity in individuals with schizophrenia can play a key role in maintaining addiction, which in turn can worsen the prognosis and exacerbate schizophrenia symptoms.
Impulsivity has an impact on increased substance abuse, and substance abuse directly affects the worsening of schizophrenia symptoms and suicide. Additionally, impulsivity itself can be a reason for suicide. Therefore, the comorbidity of these three factors can serve as predictors of suicide in individuals with schizophrenia.
Conclusion
Given the high suicide rate among individuals with schizophrenia, this issue has become a serious problem. Therefore, addressing suicide risk factors in these patients is of great importance for the management and prevention of suicide.
Numerous studies have focused solely on examining these suicide risk factors in individuals with schizophrenia, but to date, there has been limited research on predicting several of these factors for suicide.
The conducted studies indicate a high comorbidity between substance abuse and schizophrenia, and it has a significant impact on suicide in these patients. Additionally, sensory processing and impulsivity are crucial factors in self-harm and suicide attempts, although they have received less attention.
By examining the predictive impact of mentioned factors, it is possible to prevent suicide in schizophrenia by controlling and managing them.
Ethical Considerations
Compliance with ethical guidelines
This article is a review study with no human or animal sample.
Funding
The paper was extracted from the master's thesis of Roya Shourvazi, approved by the Department of Occupational Therapy, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Authors' contributions
Conceptualization and supervision: Marzieh Pashmdarfard, and Roya Shourvazi; Methodology: Marzieh Pashmdarfard and Navid Mirzakhany; Funding acquisition, and resources: Amir Rahmnanirasa. Writing the original draft: Roya shourvazi, and Maedeh Loabichian; Investigation, review and editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors express their gratitude to Shahid Beheshti University of Medical Sciences, Tehran, Iran.
References
Schizophrenia is known as a debilitating mental disorder with the appearance of various symptoms, such as delusions, hallucinations, disturbed speech or behavior and cognitive impairment. Its early onset, along with its chronic symptoms, makes it a disabling disorder for many patients and their families [1]. Schizophrenia affects approximately 1% of the population worldwide and typically the onset of the disease occurs early in life (usually in late adolescence or early adulthood). Most patients have long-term side effects [2].
The main reasons for this disorder are not well understood and a combination of genetic and environmental factors play a role in the emergence of this disease [1, 3]. Environmental factors include birth complications, such as oxygen deprivation [4] and prematurity [5]. Advanced paternal age can also contribute to the development of schizophrenia [6]. Other non-genetic factors associated with the onset of schizophrenia include trauma, social isolation, migration, city life and substance abuse [7].
The primary reason for death among people with schizophrenia spectrum disorders (SSD) is suicide. The rate of suicide attempts among individuals with psychotic disorders ranges from 10% to 50%. Approximately 40% to 79% of individuals with schizophrenia report suicidal ideation at least once during their illness [8]. Even in the early stages of schizophrenia, the suicide rate is 2.4%, and in the first five years of the illness, the suicide rate is 0.48% per year [9].
Various risk factors for suicide among individuals with schizophrenia have been identified. Being male, being Caucasian, younger age, having concurrent depression, history of suicide attempts and lack of social support are the most influential factors [10]. Additionally, the risk of suicide significantly increases in the presence of substance abuse or dependence [11].
Substance abuse is common among people with schizophrenia, particularly in men. Nearly 50% of individuals with schizophrenia have a comorbid substance use disorder (SUD) at some stage during their illness [2]. Substance abuse in schizophrenia is associated with worse outcomes, including severe psychotic symptoms and less treatment adherence [12].
Regarding substance abuse, most studies report an increased risk of suicide and aggression [9] and most individuals with schizophrenia suffer from comorbid conditions, including impulse control disorders [13]. Sensory processing is one of the basic brain functions that is impaired in individuals with schizophrenia and this impaired sensory processing is related to emotional regulation and symptoms, such as suicidal thoughts and hopelessness [14].
Sensory processing refers to the way the nervous system receives sensory signals and converts them into appropriate behavioral and motor responses [15]. The sensory processing pattern in patients with psychiatric disorders, including schizophrenia demonstrates lower levels of sensory registration, sensory avoidance and sensory sensitivity, as well as reduced sensory-seeking behavior [16].
According to the studies, substance abuse and impulsivity are related to each other and exacerbate each other [13, 17] and these two factors, along with altered sensory processing, have a vital effect on the incidence of suicide in patients with schizophrenia [14]. Most studies in the field of suicide in individuals with schizophrenia have investigated the relationship between demographic factors such as age, gender, etc. [9, 18]. Despite the high importance of the three components of substance abuse, impulsivity, and sensory processing in the incidence of suicide in schizophrenic patients, fewer studies have investigated the relationship between these components in the suicide of these patients and also the studies that have been conducted in this field provide contradictory information about the relationship between these factors and the suicide of individuals with schizophrenia.
On the other hand, due to the high rate of suicide in schizophrenic patients, more and more in-depth investigations in this field and further investigation of risk factors and their relationship to the occurrence of suicide can be effective in preventing suicide and helping to reduce its rate and increase the life expectancy of these patients.
Therefore, this study was conducted to review the relationship between three variables of sensory processing, substance abuse, and impulsivity with suicide in patients with schizophrenia.
Materials and Methods
The present study is a literature review conducted using a systematic search approach. The keywords listed in the Table 1 were searched in databases, such as PubMed, Web of Science, and Google Scholar from 2010 to 2024.

Results
Using the keywords listed in Table 1, first, 372 articles were found after that 16 articles were identified as the most recent and relevant articles. These include 5 articles on suicide in schizophrenia, 3 articles on sensory processing in schizophrenia, 5 articles on substance abuse in schizophrenia and 3 articles on impulsivity and schizophrenia, as reported in Table 2.


Discussion
This study includes the results of 16 articles published from 2010 to 2022. The main results of this review are as follows:
The suicide rate in schizophrenia is significantly higher than in the population. Various studies report different incidences of suicide in schizophrenia. In a comprehensive review conducted by Lu et al. [19] in 2020, the lifetime suicide rate was reported to be 26.8%. However, another study conducted by Aydin et al. [20] in 2019 reported a much higher suicide rate among these patients. In this study, it was mentioned that at least 40.8% of individuals with schizophrenia attempted and 39.6% of these individuals attempted suicide repeatedly. Different studies, using different populations and methodologies, provide different estimates of suicide rates in schizophrenia. The population size in the first study was much larger than in the second study, and the significant difference in the reported prevalence of suicide may be due to this reason. The first study appears to provide a more accurate statistical estimate due to a more extensive investigation.
In two other studies conducted in 2021, Berardelli et al. [21] also reported the suicide attempt rate among individuals with schizophrenia to be between 25% and 50%, while Bai et al. [22] 34.5% of these patients had suicidal thoughts and 44.3% of planned suicides, which is consistent with the above studies.
In 2019, the suicide rate in individuals with schizophrenia was reported to be 10% [18]. This rate significantly differs from the prevalence reported in other studies, indicating a potential increase in suicide rates among these patients over time.
Despite the varying prevalence rates mentioned, all of these studies indicate that suicide is the most significant factor in reducing hope for life and the main cause of mortality in individuals with schizophrenia, emphasizing the need for careful examination. Furthermore, individuals who attempt suicide tend to have more severe symptoms.
Therefore, suicide in schizophrenia is a serious and highly prevalent issue, with its rates increasing over time. By addressing the risk factors and factors associated with suicide, it is possible to reduce its occurrence in these patients.
Sensory processing in schizophrenia
Sensory processing and its patterns in schizophrenia have been the subject of studies that have demonstrated significant sensory differences compared to healthy individuals. In studies conducted by van den Boogert et al. in 2022 [16], Halperin et al. [23] and Zhou et al. [24] in 2020, it was shown that sensory processing is compromised in individuals with schizophrenia, and sensory avoiding and sensory sensitivity patterns are observed to a greater extent than in healthy individuals. The low registration pattern is significantly more prevalent in these patients compared to the healthy group, while sensory seeking is less common.
Halperin et al. [23] also addressed in their study that sensory processing difficulties can have a significant impact on daily functioning, social performance and quality of life. These studies also indicated a significant relationship between sensory processing problems and psychiatric symptoms.
Therefore, the multiple sensory processing difficulties in these patients can have highly detrimental effects on their lives, including reduced quality of life, diminished functional capacity, and increased hopelessness. Consequently, due to the high prevalence of sensory processing problems in schizophrenia and their impact on the lives of these patients, studying these issues is of utmost importance.
Substance abuse in schizophrenia
The comorbidity of substance abuse is highly common. Hunt et al. [25] reported an occurrence rate of substance abuse in schizophrenia at 41.7%. Kelkar et al. [26] reported a prevalence rate of 48%. Both studies also noted that substance abuse is significantly more prevalent in men with schizophrenia than in women.
Chaudhury et al. [27] showed that substance abuse was recognized as a critical risk factor for schizophrenia. It was also stated that substance abuse precedes schizophrenia in over 60% of cases, and in most instances, both occurrences happen within a month, suggesting a potential causal connection between substance abuse and schizophrenia.
According to the results of studies, substance abuse can have detrimental effects on the course of schizophrenia. Hunt et al. [25] and Kelkar et al. [26] indicated that substance abuse can lead to an earlier onset of schizophrenia, exacerbate negative and positive symptoms, and prolong the duration of the illness.
Studies have also demonstrated that substance abuse can lead to increased self-harm and mortality rates in individuals with schizophrenia. Güney et al. [28] stated in their study that substance abuse can increase self-harm by four times in patients with schizophrenia, making it a significant predictor of self-harm in these individuals. Another study conducted by Lähteenvuo et al. [29] found that substance abuse leads to a 50% to 100% increase in hospitalizations and mortality in schizophrenia.
The prevalence of substance abuse in schizophrenia is increasing over time, likely due to easier access to drugs and the higher inclination of people with schizophrenia towards substance use. The comorbidity of substance abuse and schizophrenia worsens the prognosis for these patients and is considered a major risk factor for suicide in this population.
Impulsivity in Schizophrenia
The study results of Ouzir et al. [17], Sehgal and Patil [30] and Iancu et al. [31] have indicated that impulsivity in schizophrenia is associated with increased suicide and self-harm.
Ouzir et al. [17] also stated that impulsivity in individuals with schizophrenia can play a key role in maintaining addiction, which in turn can worsen the prognosis and exacerbate schizophrenia symptoms.
Impulsivity has an impact on increased substance abuse, and substance abuse directly affects the worsening of schizophrenia symptoms and suicide. Additionally, impulsivity itself can be a reason for suicide. Therefore, the comorbidity of these three factors can serve as predictors of suicide in individuals with schizophrenia.
Conclusion
Given the high suicide rate among individuals with schizophrenia, this issue has become a serious problem. Therefore, addressing suicide risk factors in these patients is of great importance for the management and prevention of suicide.
Numerous studies have focused solely on examining these suicide risk factors in individuals with schizophrenia, but to date, there has been limited research on predicting several of these factors for suicide.
The conducted studies indicate a high comorbidity between substance abuse and schizophrenia, and it has a significant impact on suicide in these patients. Additionally, sensory processing and impulsivity are crucial factors in self-harm and suicide attempts, although they have received less attention.
By examining the predictive impact of mentioned factors, it is possible to prevent suicide in schizophrenia by controlling and managing them.
Ethical Considerations
Compliance with ethical guidelines
This article is a review study with no human or animal sample.
Funding
The paper was extracted from the master's thesis of Roya Shourvazi, approved by the Department of Occupational Therapy, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Authors' contributions
Conceptualization and supervision: Marzieh Pashmdarfard, and Roya Shourvazi; Methodology: Marzieh Pashmdarfard and Navid Mirzakhany; Funding acquisition, and resources: Amir Rahmnanirasa. Writing the original draft: Roya shourvazi, and Maedeh Loabichian; Investigation, review and editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors express their gratitude to Shahid Beheshti University of Medical Sciences, Tehran, Iran.
References
- Patel KR, Cherian J, Gohil K, Atkinson D. Schizophrenia: Overview and treatment options. P & T. 2014; 39(9):638-45. [PMID] [PMCID]
- Carlborg A, Winnerbäck K, Jönsson EG, Jokinen J, Nordström P. Suicide in schizophrenia. Expert Review of Neurotherapeutics. 2010; 10(7):1153-64. [DOI:10.1586/ern.10.82] [PMID]
- MacDonald AW, Schulz SC. What we know: Findings that every theory of schizophrenia should explain. Schizophrenia Bulletin. 2009; 35(3):493-508. [DOI:10.1093/schbul/sbp017]
- Dalman C, Thomas HV, David AS, Gentz J, Lewis G, Allebeck P. Signs of asphyxia at birth and risk of schizophrenia: Population-based case-control study. The British Journal of Psychiatry. 2001; 179(5):403-8. [DOI:10.1192/bjp.179.5.403]
- Ichiki M, Kunugi H, Takei N, Murray RM, Baba H, Arai H, et al. Intra-uterine physical growth in schizophrenia: Evidence confirming excess of premature birth. Psychological Medicine. 2000; 30(3):597-604. [DOI:10.1017/S003329179900210X]
- Dalman C, Allebeck P. Paternal age and schizophrenia: Further support for an association. American Journal of Psychiatry. 2002; 159(9):1591-2. [DOI:10.1176/appi.ajp.159.9.1591]
- Stilo SA, Murray RM. Non-genetic factors in schizophrenia. Current Psychiatry Reports. 2019; 21:1-0. [DOI:10.1007/s11920-019-1091-3]
- Jakhar K, Beniwal RP, Bhatia T, Deshpande SN. Self-harm and suicide attempts in Schizophrenia. Asian Journal of Psychiatry. 2017; 30:102-6. [DOI:10.1016/j.ajp.2017.08.012]
- Popovic D, Benabarre A, Crespo JM, Goikolea JM, González‐Pinto A, Gutiérrez‐Rojas L, et al. Risk factors for suicide in schizophrenia: Systematic review and clinical recommendations. Acta Psychiatrica Scandinavica. 2014; 130(6):418-26. [DOI:10.1111/acps.12332]
- Cohen CI, Abdallah CG, Diwan S. Suicide attempts and associated factors in older adults with schizophrenia. Schizophrenia Research. 2010; 119(1-3):253-7. [DOI:10.1016/j.schres.2010.03.010]
- Hawton K, Sutton L, Haw C, Sinclair J, Deeks JJ. Schizophrenia and suicide: Systematic review of risk factors. The British Journal of Psychiatry. 2005; 187(1):9-20. [DOI:10.1192/bjp.187.1.9]
- Winklbaur B, Ebner N, Sachs G, Thau K, Fischer G. Substance abuse in patients with schizophrenia. Dialogues in Clinical Neuroscience. 2006; 8(1):37-43. [DOI:10.31887/DCNS.2006.8.1/bwinklbaur]
- Dumais A, Potvin S, Joyal C, Allaire JF, Stip E, Lesage A, et al. Schizophrenia and serious violence: a clinical-profile analysis incorporating impulsivity and substance-use disorders. Schizophrenia Research. 2011; 130(1-3):234-7. [DOI:10.1016/j.schres.2011.02.024]
- Serafini G, Gonda X, Canepa G, Pompili M, Rihmer Z, Amore M, et al. Extreme sensory processing patterns show a complex association with depression, and impulsivity, alexithymia, and hopelessness. Journal of Affective Disorders. 2017; 210:249-57. [DOI:10.1016/j.jad.2016.12.019]
- Lonkar H. An overview of sensory processing disorder [Honors Theses]. Kalamazoo: Western Michigan University; 2014. [Link]
- van den Boogert F, Klein K, Spaan P, Sizoo B, Bouman YH, Hoogendijk WJ, Roza SJ. Sensory processing difficulties in psychiatric disorders: A meta-analysis. Journal of Psychiatric Research. 2022; 151:173-80. [DOI:10.1016/j.jpsychires.2022.04.020]
- Ouzir M. Impulsivity in schizophrenia: A comprehensive update. Aggression and Violent Behavior, 2013; 18(2):247-54. [DOI:10.1016/j.avb.2012.11.014]
- Sher L, Kahn RS. Suicide in schizophrenia: An educational overview. Medicina. 2019; 55(7):361. [DOI:10.3390/medicina55070361]
- Lu L, Dong M, Zhang L, Zhu XM, Ungvari GS, Ng CH, et al. Prevalence of suicide attempts in individuals with schizophrenia: A meta-analysis of observational studies. Epidemiology and Psychiatric Sciences. 2020; 29:e39. [DOI:10.1017/S2045796019000313]
- Aydın M, İlhan BÇ, Tekdemir R, Çokünlü Y, Erbasan V, Altınbaş K. Suicide attempts and related factors in schizophrenia patients. Saudi Medical Journal. 2019; 40(5):475-82. [DOI:10.15537/smj.2019.5.24153] [PMID]
- Berardelli I, Rogante E, Sarubbi S, Erbuto D, Lester D, Pompili M. The importance of suicide risk formulation in schizophrenia. Frontiers in Psychiatry. 2021; 12:779684. [DOI:10.3389/fpsyt.2021.779684]
- Bai W, Liu ZH, Jiang YY, Zhang QE, Rao WW, Cheung T, et al. Worldwide prevalence of suicidal ideation and suicide plan among people with schizophrenia: A meta-analysis and systematic review of epidemiological surveys. Translational Psychiatry. 2021; 11(1):552. [DOI:10.1038/s41398-021-01671-6]
- Halperin L, Falk-Kessler J. Schizophrenia spectrum disorders: Linking motor and process skills, sensory patterns and psychiatric symptoms. The Open Journal of Occupational Therapy. 2020; 8(1):1-13. [DOI:10.15453/2168-6408.1659]
- Zhou HY, Yang HX, Cui XL, Shi LJ, Gong JB, Lui SS, et al. Self-reported sensory responsiveness patterns in typically-developing and early-onset schizophrenia adolescents: Its relationship with schizotypal and autistic traits. Journal of Psychiatric Research. 2020; 131:255-62. [DOI:10.1016/j.jpsychires.2020.10.002]
- Hunt GE, Large MM, Cleary M, Lai HM, Saunders JB. Prevalence of comorbid substance use in schizophrenia spectrum disorders in community and clinical settings, 1990–2017: Systematic review and meta-analysis. Drug and Alcohol Dependence. 2018; 191:234-58. [DOI:10.1016/j.drugalcdep.2018.07.011]
- Kelkar P, Vankar GK, Mishra KK, John S, Ghogare AS. Prevalence of substance abuse in patients with schizophrenia. Journal of Clinical and Diagnostic Research. 2020; 14(3):VC01-5. [DOI:10.7860/JCDR/2020/43287.13577]
- Chaudhury S, Krishna Tikka S, Kumar Bakhla A. Impact of substance use disorder on presentation of schizophrenia. Dual Diagnosis. 2016. 1(2):7. [DOI:10.21767/2472-5048.100007]
- Güney E, Alnıak İ, Erkıran M. Predicting factors for non-suicidal self-injury in patients with schizophrenia spectrum disorders and the role of substance use. Asian Journal of Psychiatry. 2020; 52:102068. [DOI:10.1016/j.ajp.2020.102068]
- Lähteenvuo M, Batalla A, Luykx JJ, Mittendorfer‐Rutz E, Tanskanen A, Tiihonen J, et al. Morbidity and mortality in schizophrenia with comorbid substance use disorders. Acta Psychiatrica Scandinavica. 2021; 144(1):42-9. [DOI:10.1111/acps.13291]
- Sehgal V, Patil PS. Impulsivity, aggression and suicide risk in patients with schizophrenia: A cross-sectional study. Annals of the Romanian Society for Cell Biology, 2021; 25(1) 3426-33. [Link]
- Iancu I, Bodner E, Roitman S, Piccone Sapir A, Poreh A, Kotler M. Impulsivity, aggression and suicide risk among male schizophrenia patients. Psychopathology. 2010; 43(4):223-9. [DOI:10.1159/000313520]
Type of Study: Review Article |
Subject:
Occupational Therapy
Received: 2024/06/16 | Accepted: 2024/10/15 | Published: 2024/03/12
Received: 2024/06/16 | Accepted: 2024/10/15 | Published: 2024/03/12





