Volume 7, Issue 1 (Continuously Updated 2024)
Func Disabil J 2024, 7(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kazemi K, Salehi R, Sanjari M A, Torkaman A. Intralimb Coordination Pattern of the Lower Limbs in Male Athletes With Allograft and Autograft Anterior Cruciate Ligament Reconstruction During Landing. Func Disabil J 2024; 7 (1) : 294.1
URL: http://fdj.iums.ac.ir/article-1-245-en.html
URL: http://fdj.iums.ac.ir/article-1-245-en.html
1- Department of Physiotherapy, Rehabilitation Research Center, School of Rehabilitation Sciences, Iranian Center of Excellence in Physiotherapy, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Physiotherapy, Rehabilitation Research Center, School of Rehabilitation Sciences, Iranian Center of Excellence in Physiotherapy, Iran University of Medical Sciences, Tehran, Iran. ,salehi200@yahoo.com
3- Department of Rehabilitation Basic Sciences, Rehabilitation Research Center, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
4- Department of Orthopedic, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Physiotherapy, Rehabilitation Research Center, School of Rehabilitation Sciences, Iranian Center of Excellence in Physiotherapy, Iran University of Medical Sciences, Tehran, Iran. ,
3- Department of Rehabilitation Basic Sciences, Rehabilitation Research Center, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
4- Department of Orthopedic, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 1199 kb]
(2917 Downloads)
| Abstract (HTML) (1290 Views)
Full-Text: (274 Views)
Introduction
An anterior cruciate ligament (ACL) tear is one of the most common knee injuries among athletes [1, 2]. This ligament plays a crucial role in knee function and thus its damage leads to immobility, damage to cartilage, and joint destruction diseases [3, 4]. In addition to the mechanical role of ACL, the stimulation of mechanical receptors within the ligament results in muscle function about the joint as a motor control toward sudden movements [5]. Damage to the anterior cruciate ligament causes a partial interruption of the afferent pathway and changes the spinal and supraspinal control of motor function, which is followed by a change in joint proprioceptive accuracy and movement strategy and patterns [6]. Therefore, this injury is considered a neurophysiological dysfunction and not just a knee skeletal-muscular injury [7, 8]. ACL injuries are more common among athletes aged 15-40 who perform activities involving knee rotation, such as soccer, handball, volleyball, and alpine skiing [9, 10].
Annually, 15% of elite athletes suffer from such injuries [10]. In the United States, about 250000 cases of ACL injuries have been reported, mostly caused by sudden, non-collision, and non-directional deceleration [9, 11].
On the other hand, non-invasive treatments in injured people usually cause common instabilities and decreased activity levels, subsequently leading to long-term injury complications [12]. Various factors, including injury pattern, injury severity, possible damages following surgery, and the probability of simultaneous tissue reparability affect the decision-making to perform surgical or non-surgical treatment procedures [13, 14]. Reconstruction of the anterior cruciate ligament is usually performed for people with a high activity level or those suffering from lateral joint laxity [14, 15]. This procedure is performed as a standard treatment to reduce instability and prevent cartilage and meniscal injuries among athletes [16]. Despite displaying an acceptable level of knee function and stability after the surgery, literature affirmed that most athletes still have some degrees of difficulty in performing coordinated movements in the operated limb [17, 18].
Landing on a limb is one of the activities causing ACL injury and this damage seems to occur during the maximum vertical force of the ground reaction [19]. An increase in vertical ground reaction force (VGRF) applied to the knee may increase anterior tibial shear force, which is one of the destructive factors for the reconstructed knee. According to Newton’s third law (action and reaction), when feet hit the ground, they apply an action force and in return, they receive the same force and reaction in the opposite direction from the ground [20]. The functional role of the lower extremity is landing, weight-bearing, and transmitting of VGRF [21]. The functional movement analysis of handball players revealed two distinct mechanisms in the case of ACL injury. One of the most common was the combination of landing with shear movement and the other was landing on a single leg causing valgus moments on the knee joint and tibia rotation position close to full extension [22]. Literature affirms that most people after ACL reconstruction will suffer from advanced osteoarthritis, re-injury, or inability to resume strength and sport-specific activities [23]. However, the risk factors for these conditions are not clear. In a natural state, the interaction of kinetic and kinematic factors causes proper coordination of segments and joints and minimizes energy consumption. In case of injuries caused by defective movements, the coordination pattern changes and this change also occurs in people with ACL reconstruction. In the dynamic system approach and kinematic analysis, the mutual effect of joints is evaluated, which provides a more comprehensive evaluation of the activity. In particular, the variability of joint coordination may determine the use or non-use of different movement strategies, revealing the system’s limitations. Variability in coordination pattern has a functional importance in movement control and makes the neuromuscular system capable of adapting to different constraints of the movement task (such as landing) in dynamic environments and maintaining stability in its consequences (speed, acceleration, and force distribution). Assessing coordination and variability phases can reveal compensatory mechanisms and describe joint excursions [23]. Furthermore, assessing coordination patterns provides comprehensive information on how the neuromuscular system organizes different degrees of freedom in movements. The variability of joint coordination is measured using the angular displacements of adjacent joints and vector coding to analyze the kinematics of the lower limb.
The results from quantifying and comparing the coordination variability between the operated and control groups can contribute to our knowledge regarding activity-related ACL injury. It is expected that by increasing our knowledge about different side effects of functional activities and returning to sports that may be related to the lack of proper coordination of joint pain, the rehabilitation program can properly organize the degrees of freedom in people with different injuries to reduce surgery-associated side effects and the rate of re-injury as well as increasing the quality level of appropriate sports activities leading to the desired direction. Therefore, this study was conducted to compare the joint coordination patterns and joint forces in people with autograft and allograft reconstruction surgery of ACL during the landing activity.
Materials and Methods
Study type and participants
This case-control study was conducted among male athletes in an age range of 18 to 35 years old who were undergoing surgery in two different groups, a minimum of 9 months and a maximum of two years have passed since their surgery. One group included athletes who underwent ACL reconstruction surgery with autograft, and the other included those who underwent reconstruction surgery with allograft. Finally, the control group was considered as healthy male athletes in the same age category.
Study sample size
Based on the pilot study that was conducted on 8 people with eligible criteria to take part in the research, G-Power software was used to calculate the study sample size based on the comparison of case and control groups. A total of 61 people were recruited for the study; among which 40 patients were considered as a case group, including 18 athletes who underwent ACL reconstruction surgery with autograft and 22 patients who underwent reconstruction surgery with allograft. Gender and sports activity levels were used to match the groups. All the athletes in different fields, including football, volleyball, basketball, and handball were engaged in sports activities that included movement and rotation challenges and landing activities. Number of participants from each activity group was matched accordingly. All people who underwent arthroscopic surgery were operated on by knee orthopaedic surgeons and were under the supervision of a sports physiotherapist to receive a full rehabilitation period. They also underwent balance training and started running about three months after the surgery. Likewise, they passed the courses of weight training, agility training, plyometrics, starts, and specialized sports activities. Then, a minimum of 9 months and a maximum of 24 months after the surgery, if they successfully could pass the muscle strength and distance jumping tests in the absence of pain and swelling, they were allowed to participate in intense sports activities and competitions without movement restrictions.
Inclusion and exclusion criteria
The inclusion criteria included all patients with unilateral anterior cruciate ligament reconstruction surgery with allograft and autograft methods, male athletes who have been a minimum of 9 months and at most 24 months since their surgery, successfully passing a series of quadriceps and hamstring strength tests and distance jumping before entering sports-specific activities under the supervision of a sports physiotherapist, and returning to pre-injury sports activities. The exclusion criteria included patients with a history of bilateral damage or surgery in the knee or meniscectomy, repair of the meniscus and lateral ligaments, pain and swelling of the soft tissue of the knee joint, and limited range of joint motion as well as patients with a history of surgery in lower limbs and spine joints in ACL reconstruction group, having metabolic-rheumatoid and neurological diseases, suffering from cardiovascular and pulmonary problems, and having obvious misalignments, such as crossed knees, bent knees and flat feet.
Study data collection
The Tegner questionnaire, developed in 1985, was initially designed for physician administration after ACL and meniscal injuries. This activity rating system, often used by patients, consists of a one-item score that ranks work and sports activities on a scale of 0 to 10. Zero signifies disability due to knee problems and 10 represents national or international level soccer [24]. Negahban et al. published the Persian translation of this questionnaire, with proven validity and reliability [25]. The second questionnaire was introduced by the International Knee Document Committee (IKDC) to examine patients’ subjective perception of performance and measure functional disability of patients in performing daily and sports activities [26]. The validity and reliability of the questionnaire have been proven, particularly in the case of ACL [26]. Furthermore, Rahimi et al. [27]. prepared and published its Persian translation for Iranian patients after ligament and meniscus surgery.
Before landing, all study participants warmed up by cycling on a stationary bike and gentle stretching of the muscles of the lower limbs with very short stretches and three repetitions for each muscle group. Then to learn how to perform the test, the participants were asked to land on a 30 cm obstacle five times, with a 30-s rest between each landing [28]. Afterward, three single-limb landing attempts were performed in a random order for each limb separately. Furthermore, Qualisys 3D motion analysis system with 120 Hz frequency with six cameras and tracking markers placed on the pelvis and lower limbs were used to record kinematic information. To track, joints’ position markers were placed on the sacrum, bilateral superior posterior iliac spine, bilateral superior anterior iliac spine, greater trochanter of the femur, the lateral and medial condyles of the femur, lateral and medial malleolus of the ankle, and the first and the fifth metatarsals [17, 29]. In three landings, the joint angles of the hip, knee, and ankle were recorded for each limb and then, the range of motion of the body joints was measured by calculating the difference between the minimum and maximum range of motion of a joint. VGRF data was calculated by the Kistler force plate device with a frequency of 100 Hz and normalized based on each athlete’s weight. Kinetic information was also obtained by measuring VGRF and joint torques normalized for height and body weight.
Study data analysis
Based on the literature, 6 pairs of joint movements were selected to analyze kinematic differences [17, 18, 30]. Accordingly, hip abduction-adduction/knee abduction-adduction (HA/KA), hip abduction-adduction/knee rotation (HA/KR), hip flexion-extension/knee flexion-extension (HF/KF), hip rotation/knee abduction-adduction (HR/KA), hip rotation/knee rotation (HR/KR) and knee flexion-extension/ ankle dorsiflexion-plantar flexion (KF/ADF) were measured. Before performing the test, the method of single-leg vertical landing was explained to the participants. Then, they were asked to stand on a 30 cm obstacle 11 cm from the edge of the force plate with the ankle in a neutral position [28]. To avoid lateral movement and vertical landing on the centre of the force plane, they were also told to place their hands on the hip on both sides and the knee of their opposite limb to be in 90 degrees of flexion. With the examiner’s verbal command, participants landed on the force plate. This activity was repeated three times and was valid when the foot landed in the right place of a force plane and the balance was kept on the lower limb [28].
Information about joint angles was entered into MATLAB software, and biomechanical analysis was performed for all participants. Sparrow et al. first used this method in 1987 to measure movement coordination and included drawing axes in the angle map for adjacent points [31]. The vector coding method was used to analyze the kinematics of the lower limb and quantitatively measure the variability of the joint coordination. Likewise, the joint angles of lower limbs were calculated in landing phases.
Study statistical analysis
First, the normality of variables was checked via the Kolmogorov-Smirnov test. Descriptive data analysis was performed to capture data in terms of Mean±SD. Then, to examine the effect size in variables, partial η2 was used. A P<0.05 was considered statistically significant.
Results
Table 1 presents the study participants’ characteristics.

As the results reveal, the variables’ values in three different study groups are close to each other.
Tables 2 and 3 present the results of comparing joint coordination variability and magnitude between reconstructed autograft and allograft groups.
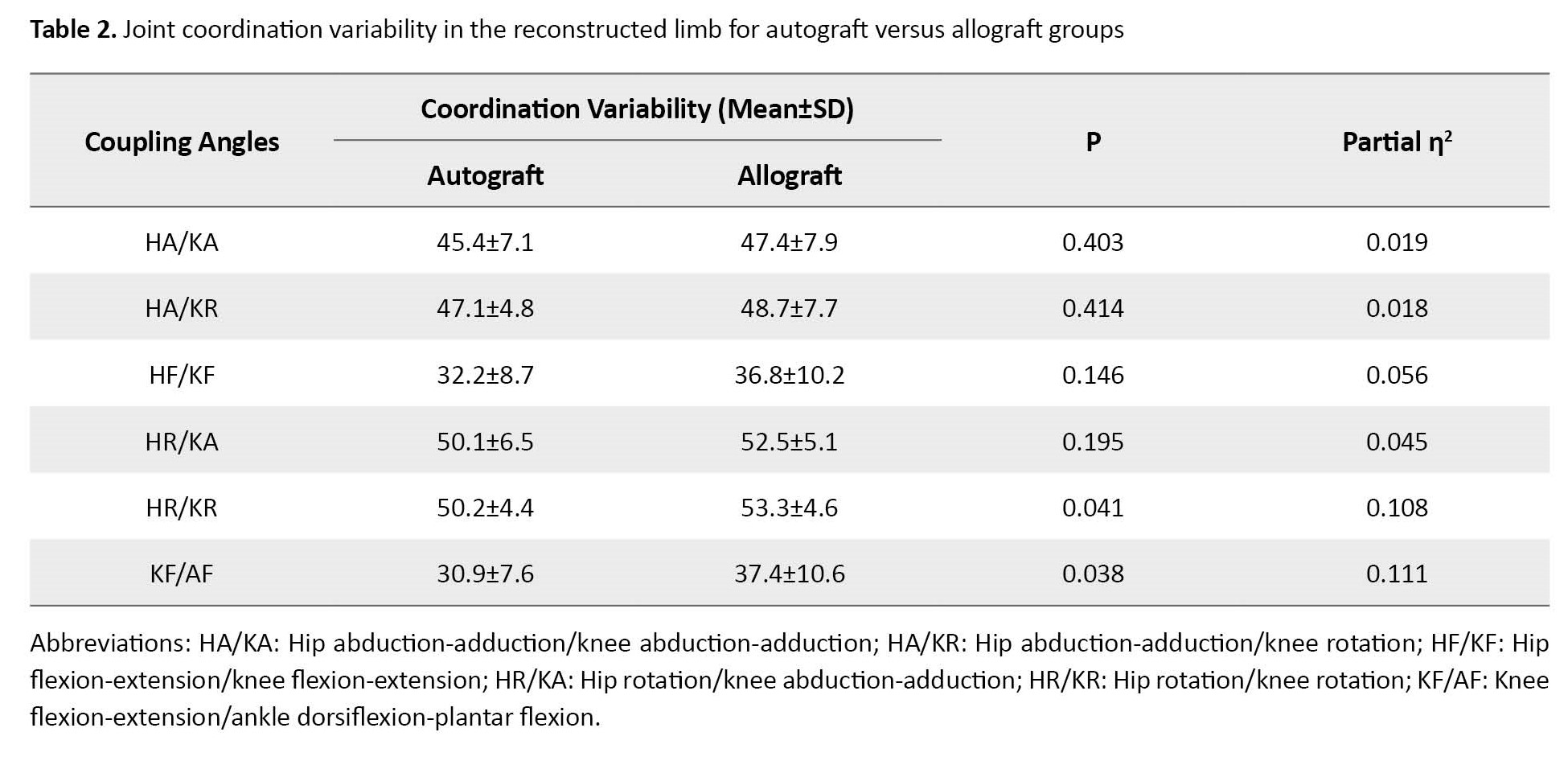

The results showed no statistically significant difference in joint coordination variability based on groups (P=0.153). However, regarding joint coordination magnitude, a statistically significant difference was observed between groups (F(6, 32)=2.51, P=0.042; Wilk’s Λ=0.680, partial η2=0.32).
Tables 4 and 5 present the results related to the comparison of joint coordination variability and magnitude between reconstructed autograft and matched limb health groups.
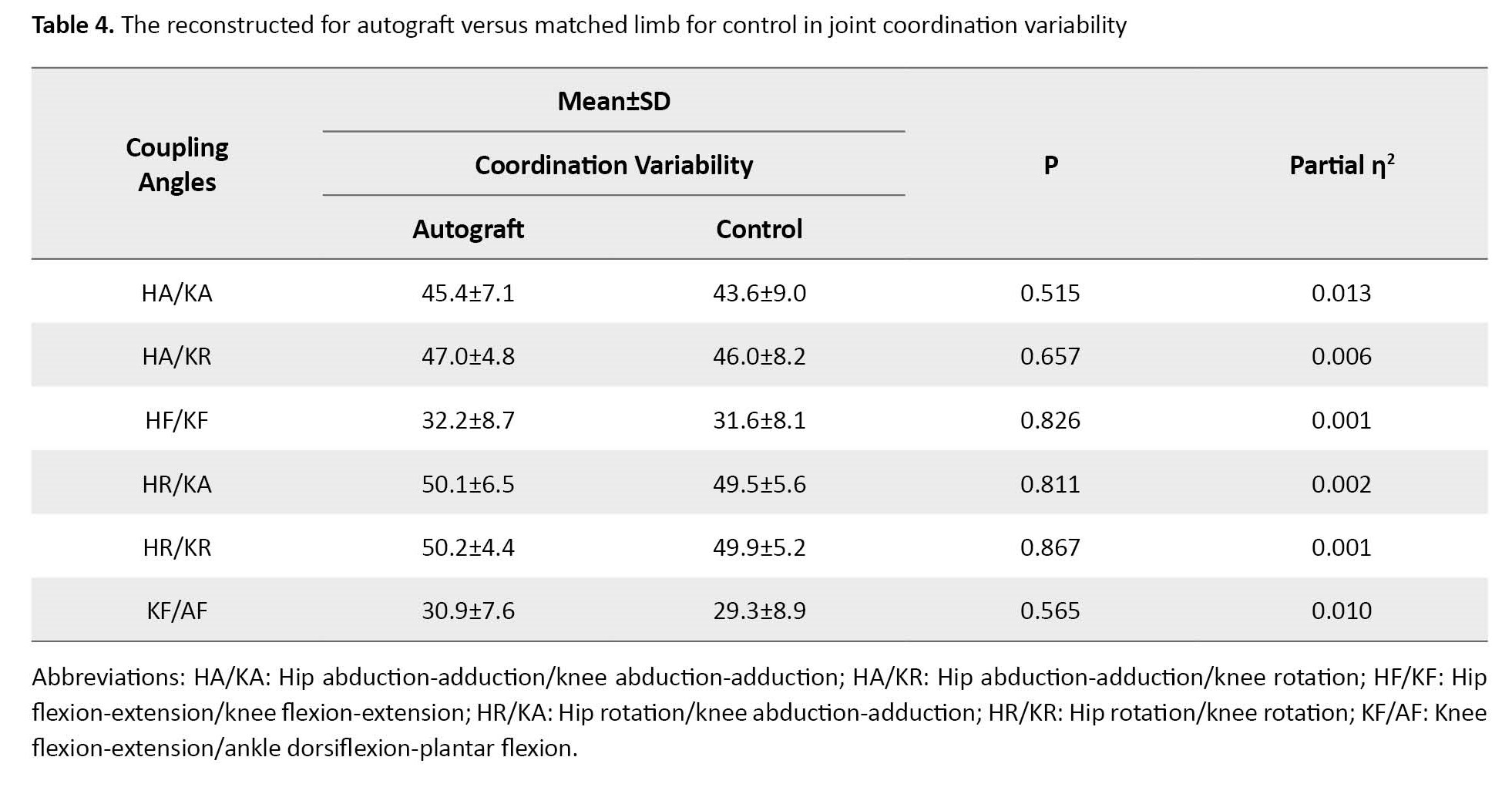

No significant difference was observed in joint coordination variability based on groups (P=0.971).
Likewise, no significant difference was found in terms of joint coordination magnitude in different study groups (P=0.476).
Tables 6 and 7 present the results related to the comparison of joint coordination variability and magnitude between reconstructed allograft and matched limb health groups.

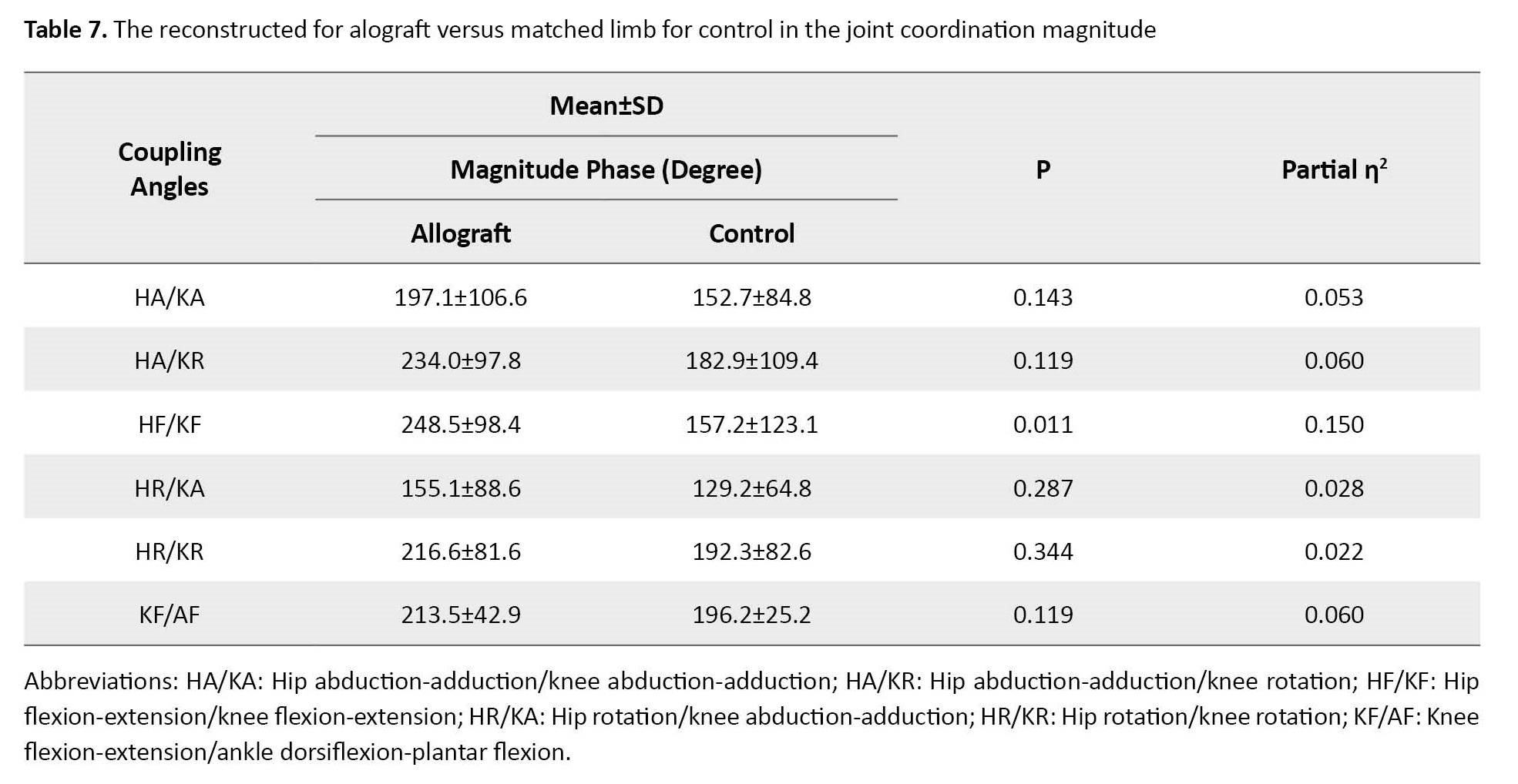
No significant difference was observed in joint coordination variability based on groups (P=0.140).
Table 7 presents a significant difference in joint coordination magnitude based on groups (F(6, 35)=2.55, P=0.037; Wilk’s Λ=0.695, partial η2=0.31).
Discussion
The goal of ACL reconstruction is to improve the function and firmness of the knee joint to return patients to pre-injury skills [32]. The clinical outcomes of this surgery have been proven successful in the literature [33]. However, despite the success rate and effective return to sport, significant considerations are observed in terms of surgery cost and decreased quality of life. Ardern et al. reported that around 63% of ACLRs can successfully return to their pre-injury sport [22]. Furthermore, some studies showed that the re-injury rate increased among individuals who underwent ACL reconstruction surgery so that the risk of first-time ACL injury was estimated at 1 per 80 people, while the re-injury risk after the reconstruction was reported to be 1 in 17 individuals [34, 35].
Two main common graft options exist for ACL reconstruction, including autograft and allograft. An autograft is a graft taken from the individual’s muscle [36-39]. While allograft is a tissue graft that is transplanted from a donor’s patellar tendon, hamstring, or intact ACL. Some advantages regarding the use of an autograft focus on no risk of body rejection or disease transmission, faster incorporation into the body, lower cost, and ready availability. On the other hand, it suffers from some drawbacks, such as procurement morbidity, donor site pain, and the need for a second surgical procedure. The benefits of using an allograft are avoiding donor site defects, fewer incisions, reduced surgical and rehabilitation time, accessibility to larger grafts in varying forms, and no weakening of the extensors or flexor digitorum apparatus. However, the allograft option has some disadvantages, including the possibility of body rejection and infection transmission from the allograft. It may also increase instability and failure to return to sport [40-42].
Evidence has shown no significant differences in clinical outcomes between autografts and allografts. Based on our study results, no significant differences were observed between the two types of graft regarding joint coordination variability. Furthermore, joint coordination magnitude between autograft and matched limbs was similar for the control group. Similarly, Hu et al. reported no significant difference between autograft and allograft in terms of clinical outcomes [43]. In most literature, failure rates were very similar in the two graft options [44]. A meta-analysis conducted in 2018 revealed similar IKDC, and Tegner scores, and failure rates between two groups [45]. Likewise, a systematic review in 2014 found no significant differences between the mentioned groups regarding failure rate, knee laxity, or coordination variability [46]. On the other hand, a randomized clinical trial revealed a remarkable allograft failure rate of 27%. The probable reason for this case may be that surgeries were performed many years ago with underdeveloped surgery and processing methods [47]. Similarly, a meta-analysis found that autografts had better clinical outcomes compared to allografts [48-50]. These discrepancies may be due to various study populations, sampling methods, statistical analyses, and research designs applied in previous literature. If a satisfactory autograft is not accessible, or if a revision ACL reconstruction is the goal, allograft can be used as an optimal option. Factors, including previous reconstruction, surgery in another leg, tunnel size, or position are also among crucial determinants for preferring allografts to autografts. In most cases, studies concluded that allograft ACL reconstruction is a safe but more expensive option that can be considered in some conditions.
Regarding the rate of ligament rupture after ACL reconstruction, Jia and Sun found a higher rate of rupture and ACL reconstruction failure in the allograft group. They believed that a faster postoperative rehabilitation course in patients with allograft may lead them to return to sports and physical activity before complete healing, which increases the risk of reinjury among them [51]. A similar study compared the graft incorporation between two graft options in an animal model. Study results revealed that autografts incorporated faster compared to allografts [52]. This may be another reason for a risk of graft failure in allograft after ACL reconstruction, suggesting more need for conservative rehabilitation in allograft reconstruction patients. Despite these variations, no statistically significant differences were approved.
One of the contributions of the present research is to compare the joint coordination variability and magnitude between reconstructed allograft and matched healthy limb, reconstructed autograft and matched healthy limb, reconstructed autograft and allograft, and finally non-reconstructed autograft and allograft. Consistent with a study conducted by Davis, our study results revealed an increased variability in the ACL reconstruction group for several joint couplings compared to the control group. These results indicated that patients with ACL reconstruction exhibit a different coordinative function in their reconstructed lower extremity compared to the control group [17]. Kiefer et al. discriminated between athletes with and without ACL reconstruction based on intralimb coordination. The ACL reconstruction group showed higher variability for the low-frequency target oscillation. The increased variability in the mentioned group was interpreted as instability in these athletes that suggested a lower proprioceptive function post-surgery [53]. Pollard et al. also found an increased lower extremity variability in an ACL reconstruction group [18]. Consistent with Kiefer et al., researchers suggested a different neuromuscular control as a reason for a higher variability in the ACL reconstruction group. They mentioned the higher variability as a risk factor for re-injury [53].
Conclusion
Study results affirmed that in clinical decision-making regarding a direct choice between allografts and autografts, clinicians should consider the efficacy of different graft options and patients’ characteristics, and the variability of joint coordination as a vital element of movement. Movement variability is an integrated part of human motor behaviour . A decrease in joint coordination variability shows a limited movement capability in individuals, which subsequently leads to malmovement strategies in a dynamic system. Lower variability in study participants has also been associated with an increased likelihood of re-injury after the ACL construction procedure. Although our result reported no significant difference between groups in joint coordination variability, having an insight into coordinative function after ACL reconstruction will help develop rehabilitation programs after the surgery as well as minimize the re-injury risk among patients. We also suggest that scholars should conduct more robust trials with valid research designs to control the results comparing ACL reconstruction with autograft and allograft.
Limitations
This study has some limitations. First, blinding patients were not used in this research, which may increase the risk of bias. Second, our study included athletes with ACL reconstruction on either the right or left side of the body, regardless of limb dominance. Third, this research procedure is accomplished in a laboratory condition and results may be different in a field.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1398.1406).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, Supervision: Reza Salehi, Mohammad Ali Sanjari; Methodology: Kasr Kazemi; Investigation, Writing – review & editing: All authors; Writing – original draft: Kasra Kazemi, Reza Salehi; Funding acquisition, Resources: Kasra Kazemi, Reza Salehi.
Conflict of interest
The authors declared no conflict of interest.
References
An anterior cruciate ligament (ACL) tear is one of the most common knee injuries among athletes [1, 2]. This ligament plays a crucial role in knee function and thus its damage leads to immobility, damage to cartilage, and joint destruction diseases [3, 4]. In addition to the mechanical role of ACL, the stimulation of mechanical receptors within the ligament results in muscle function about the joint as a motor control toward sudden movements [5]. Damage to the anterior cruciate ligament causes a partial interruption of the afferent pathway and changes the spinal and supraspinal control of motor function, which is followed by a change in joint proprioceptive accuracy and movement strategy and patterns [6]. Therefore, this injury is considered a neurophysiological dysfunction and not just a knee skeletal-muscular injury [7, 8]. ACL injuries are more common among athletes aged 15-40 who perform activities involving knee rotation, such as soccer, handball, volleyball, and alpine skiing [9, 10].
Annually, 15% of elite athletes suffer from such injuries [10]. In the United States, about 250000 cases of ACL injuries have been reported, mostly caused by sudden, non-collision, and non-directional deceleration [9, 11].
On the other hand, non-invasive treatments in injured people usually cause common instabilities and decreased activity levels, subsequently leading to long-term injury complications [12]. Various factors, including injury pattern, injury severity, possible damages following surgery, and the probability of simultaneous tissue reparability affect the decision-making to perform surgical or non-surgical treatment procedures [13, 14]. Reconstruction of the anterior cruciate ligament is usually performed for people with a high activity level or those suffering from lateral joint laxity [14, 15]. This procedure is performed as a standard treatment to reduce instability and prevent cartilage and meniscal injuries among athletes [16]. Despite displaying an acceptable level of knee function and stability after the surgery, literature affirmed that most athletes still have some degrees of difficulty in performing coordinated movements in the operated limb [17, 18].
Landing on a limb is one of the activities causing ACL injury and this damage seems to occur during the maximum vertical force of the ground reaction [19]. An increase in vertical ground reaction force (VGRF) applied to the knee may increase anterior tibial shear force, which is one of the destructive factors for the reconstructed knee. According to Newton’s third law (action and reaction), when feet hit the ground, they apply an action force and in return, they receive the same force and reaction in the opposite direction from the ground [20]. The functional role of the lower extremity is landing, weight-bearing, and transmitting of VGRF [21]. The functional movement analysis of handball players revealed two distinct mechanisms in the case of ACL injury. One of the most common was the combination of landing with shear movement and the other was landing on a single leg causing valgus moments on the knee joint and tibia rotation position close to full extension [22]. Literature affirms that most people after ACL reconstruction will suffer from advanced osteoarthritis, re-injury, or inability to resume strength and sport-specific activities [23]. However, the risk factors for these conditions are not clear. In a natural state, the interaction of kinetic and kinematic factors causes proper coordination of segments and joints and minimizes energy consumption. In case of injuries caused by defective movements, the coordination pattern changes and this change also occurs in people with ACL reconstruction. In the dynamic system approach and kinematic analysis, the mutual effect of joints is evaluated, which provides a more comprehensive evaluation of the activity. In particular, the variability of joint coordination may determine the use or non-use of different movement strategies, revealing the system’s limitations. Variability in coordination pattern has a functional importance in movement control and makes the neuromuscular system capable of adapting to different constraints of the movement task (such as landing) in dynamic environments and maintaining stability in its consequences (speed, acceleration, and force distribution). Assessing coordination and variability phases can reveal compensatory mechanisms and describe joint excursions [23]. Furthermore, assessing coordination patterns provides comprehensive information on how the neuromuscular system organizes different degrees of freedom in movements. The variability of joint coordination is measured using the angular displacements of adjacent joints and vector coding to analyze the kinematics of the lower limb.
The results from quantifying and comparing the coordination variability between the operated and control groups can contribute to our knowledge regarding activity-related ACL injury. It is expected that by increasing our knowledge about different side effects of functional activities and returning to sports that may be related to the lack of proper coordination of joint pain, the rehabilitation program can properly organize the degrees of freedom in people with different injuries to reduce surgery-associated side effects and the rate of re-injury as well as increasing the quality level of appropriate sports activities leading to the desired direction. Therefore, this study was conducted to compare the joint coordination patterns and joint forces in people with autograft and allograft reconstruction surgery of ACL during the landing activity.
Materials and Methods
Study type and participants
This case-control study was conducted among male athletes in an age range of 18 to 35 years old who were undergoing surgery in two different groups, a minimum of 9 months and a maximum of two years have passed since their surgery. One group included athletes who underwent ACL reconstruction surgery with autograft, and the other included those who underwent reconstruction surgery with allograft. Finally, the control group was considered as healthy male athletes in the same age category.
Study sample size
Based on the pilot study that was conducted on 8 people with eligible criteria to take part in the research, G-Power software was used to calculate the study sample size based on the comparison of case and control groups. A total of 61 people were recruited for the study; among which 40 patients were considered as a case group, including 18 athletes who underwent ACL reconstruction surgery with autograft and 22 patients who underwent reconstruction surgery with allograft. Gender and sports activity levels were used to match the groups. All the athletes in different fields, including football, volleyball, basketball, and handball were engaged in sports activities that included movement and rotation challenges and landing activities. Number of participants from each activity group was matched accordingly. All people who underwent arthroscopic surgery were operated on by knee orthopaedic surgeons and were under the supervision of a sports physiotherapist to receive a full rehabilitation period. They also underwent balance training and started running about three months after the surgery. Likewise, they passed the courses of weight training, agility training, plyometrics, starts, and specialized sports activities. Then, a minimum of 9 months and a maximum of 24 months after the surgery, if they successfully could pass the muscle strength and distance jumping tests in the absence of pain and swelling, they were allowed to participate in intense sports activities and competitions without movement restrictions.
Inclusion and exclusion criteria
The inclusion criteria included all patients with unilateral anterior cruciate ligament reconstruction surgery with allograft and autograft methods, male athletes who have been a minimum of 9 months and at most 24 months since their surgery, successfully passing a series of quadriceps and hamstring strength tests and distance jumping before entering sports-specific activities under the supervision of a sports physiotherapist, and returning to pre-injury sports activities. The exclusion criteria included patients with a history of bilateral damage or surgery in the knee or meniscectomy, repair of the meniscus and lateral ligaments, pain and swelling of the soft tissue of the knee joint, and limited range of joint motion as well as patients with a history of surgery in lower limbs and spine joints in ACL reconstruction group, having metabolic-rheumatoid and neurological diseases, suffering from cardiovascular and pulmonary problems, and having obvious misalignments, such as crossed knees, bent knees and flat feet.
Study data collection
The Tegner questionnaire, developed in 1985, was initially designed for physician administration after ACL and meniscal injuries. This activity rating system, often used by patients, consists of a one-item score that ranks work and sports activities on a scale of 0 to 10. Zero signifies disability due to knee problems and 10 represents national or international level soccer [24]. Negahban et al. published the Persian translation of this questionnaire, with proven validity and reliability [25]. The second questionnaire was introduced by the International Knee Document Committee (IKDC) to examine patients’ subjective perception of performance and measure functional disability of patients in performing daily and sports activities [26]. The validity and reliability of the questionnaire have been proven, particularly in the case of ACL [26]. Furthermore, Rahimi et al. [27]. prepared and published its Persian translation for Iranian patients after ligament and meniscus surgery.
Before landing, all study participants warmed up by cycling on a stationary bike and gentle stretching of the muscles of the lower limbs with very short stretches and three repetitions for each muscle group. Then to learn how to perform the test, the participants were asked to land on a 30 cm obstacle five times, with a 30-s rest between each landing [28]. Afterward, three single-limb landing attempts were performed in a random order for each limb separately. Furthermore, Qualisys 3D motion analysis system with 120 Hz frequency with six cameras and tracking markers placed on the pelvis and lower limbs were used to record kinematic information. To track, joints’ position markers were placed on the sacrum, bilateral superior posterior iliac spine, bilateral superior anterior iliac spine, greater trochanter of the femur, the lateral and medial condyles of the femur, lateral and medial malleolus of the ankle, and the first and the fifth metatarsals [17, 29]. In three landings, the joint angles of the hip, knee, and ankle were recorded for each limb and then, the range of motion of the body joints was measured by calculating the difference between the minimum and maximum range of motion of a joint. VGRF data was calculated by the Kistler force plate device with a frequency of 100 Hz and normalized based on each athlete’s weight. Kinetic information was also obtained by measuring VGRF and joint torques normalized for height and body weight.
Study data analysis
Based on the literature, 6 pairs of joint movements were selected to analyze kinematic differences [17, 18, 30]. Accordingly, hip abduction-adduction/knee abduction-adduction (HA/KA), hip abduction-adduction/knee rotation (HA/KR), hip flexion-extension/knee flexion-extension (HF/KF), hip rotation/knee abduction-adduction (HR/KA), hip rotation/knee rotation (HR/KR) and knee flexion-extension/ ankle dorsiflexion-plantar flexion (KF/ADF) were measured. Before performing the test, the method of single-leg vertical landing was explained to the participants. Then, they were asked to stand on a 30 cm obstacle 11 cm from the edge of the force plate with the ankle in a neutral position [28]. To avoid lateral movement and vertical landing on the centre of the force plane, they were also told to place their hands on the hip on both sides and the knee of their opposite limb to be in 90 degrees of flexion. With the examiner’s verbal command, participants landed on the force plate. This activity was repeated three times and was valid when the foot landed in the right place of a force plane and the balance was kept on the lower limb [28].
Information about joint angles was entered into MATLAB software, and biomechanical analysis was performed for all participants. Sparrow et al. first used this method in 1987 to measure movement coordination and included drawing axes in the angle map for adjacent points [31]. The vector coding method was used to analyze the kinematics of the lower limb and quantitatively measure the variability of the joint coordination. Likewise, the joint angles of lower limbs were calculated in landing phases.
Study statistical analysis
First, the normality of variables was checked via the Kolmogorov-Smirnov test. Descriptive data analysis was performed to capture data in terms of Mean±SD. Then, to examine the effect size in variables, partial η2 was used. A P<0.05 was considered statistically significant.
Results
Table 1 presents the study participants’ characteristics.

As the results reveal, the variables’ values in three different study groups are close to each other.
Tables 2 and 3 present the results of comparing joint coordination variability and magnitude between reconstructed autograft and allograft groups.
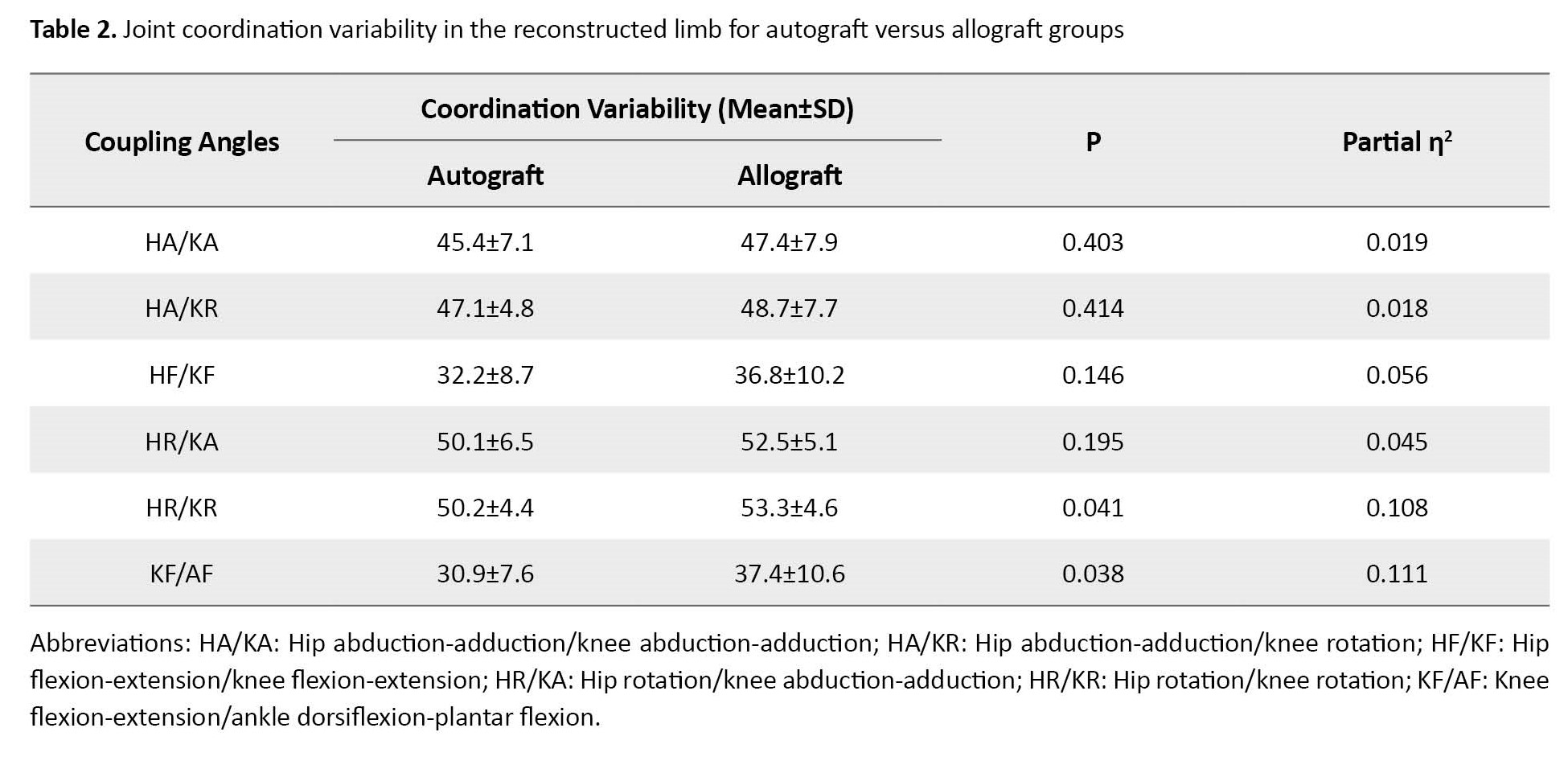

The results showed no statistically significant difference in joint coordination variability based on groups (P=0.153). However, regarding joint coordination magnitude, a statistically significant difference was observed between groups (F(6, 32)=2.51, P=0.042; Wilk’s Λ=0.680, partial η2=0.32).
Tables 4 and 5 present the results related to the comparison of joint coordination variability and magnitude between reconstructed autograft and matched limb health groups.
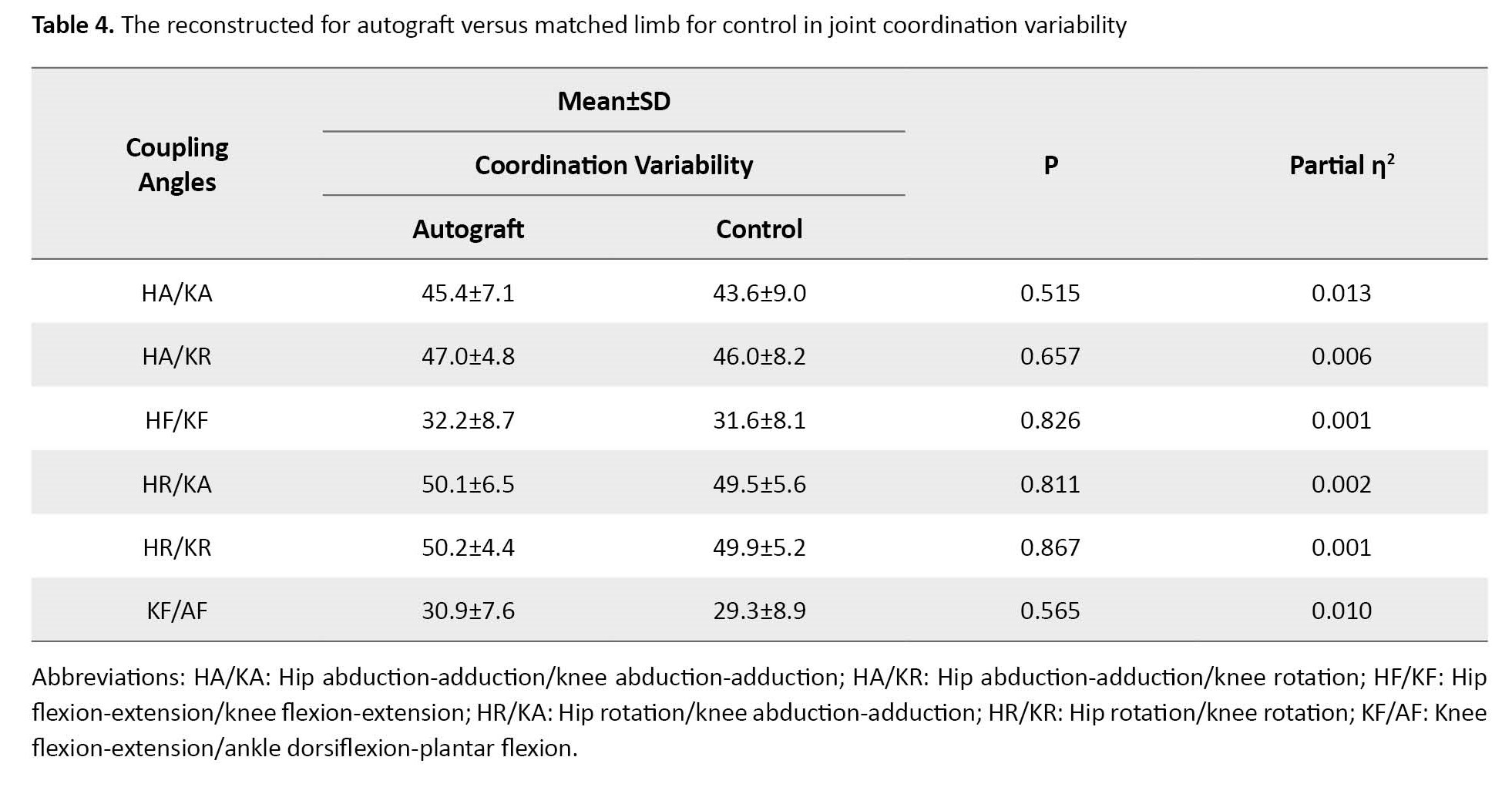

No significant difference was observed in joint coordination variability based on groups (P=0.971).
Likewise, no significant difference was found in terms of joint coordination magnitude in different study groups (P=0.476).
Tables 6 and 7 present the results related to the comparison of joint coordination variability and magnitude between reconstructed allograft and matched limb health groups.

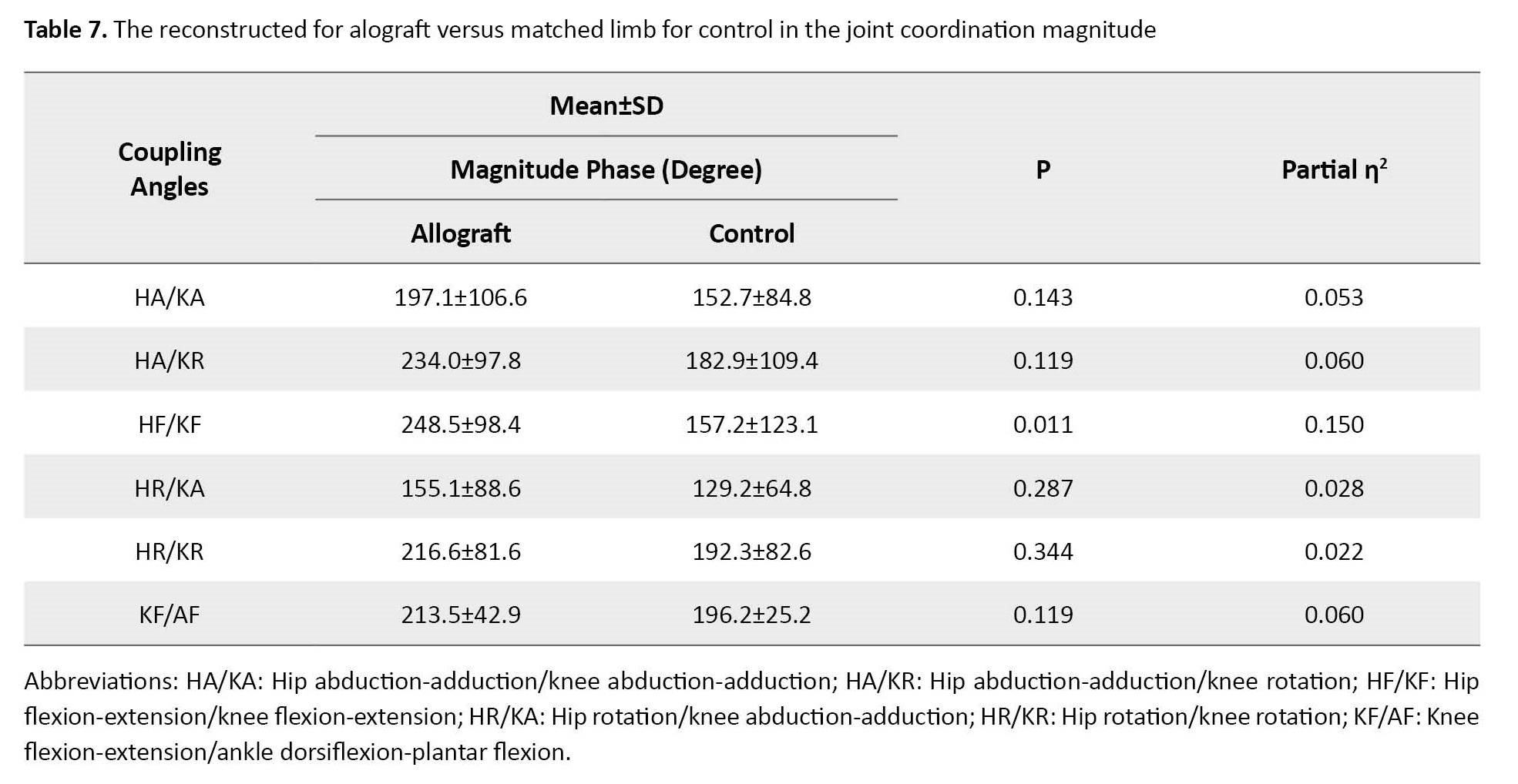
No significant difference was observed in joint coordination variability based on groups (P=0.140).
Table 7 presents a significant difference in joint coordination magnitude based on groups (F(6, 35)=2.55, P=0.037; Wilk’s Λ=0.695, partial η2=0.31).
Discussion
The goal of ACL reconstruction is to improve the function and firmness of the knee joint to return patients to pre-injury skills [32]. The clinical outcomes of this surgery have been proven successful in the literature [33]. However, despite the success rate and effective return to sport, significant considerations are observed in terms of surgery cost and decreased quality of life. Ardern et al. reported that around 63% of ACLRs can successfully return to their pre-injury sport [22]. Furthermore, some studies showed that the re-injury rate increased among individuals who underwent ACL reconstruction surgery so that the risk of first-time ACL injury was estimated at 1 per 80 people, while the re-injury risk after the reconstruction was reported to be 1 in 17 individuals [34, 35].
Two main common graft options exist for ACL reconstruction, including autograft and allograft. An autograft is a graft taken from the individual’s muscle [36-39]. While allograft is a tissue graft that is transplanted from a donor’s patellar tendon, hamstring, or intact ACL. Some advantages regarding the use of an autograft focus on no risk of body rejection or disease transmission, faster incorporation into the body, lower cost, and ready availability. On the other hand, it suffers from some drawbacks, such as procurement morbidity, donor site pain, and the need for a second surgical procedure. The benefits of using an allograft are avoiding donor site defects, fewer incisions, reduced surgical and rehabilitation time, accessibility to larger grafts in varying forms, and no weakening of the extensors or flexor digitorum apparatus. However, the allograft option has some disadvantages, including the possibility of body rejection and infection transmission from the allograft. It may also increase instability and failure to return to sport [40-42].
Evidence has shown no significant differences in clinical outcomes between autografts and allografts. Based on our study results, no significant differences were observed between the two types of graft regarding joint coordination variability. Furthermore, joint coordination magnitude between autograft and matched limbs was similar for the control group. Similarly, Hu et al. reported no significant difference between autograft and allograft in terms of clinical outcomes [43]. In most literature, failure rates were very similar in the two graft options [44]. A meta-analysis conducted in 2018 revealed similar IKDC, and Tegner scores, and failure rates between two groups [45]. Likewise, a systematic review in 2014 found no significant differences between the mentioned groups regarding failure rate, knee laxity, or coordination variability [46]. On the other hand, a randomized clinical trial revealed a remarkable allograft failure rate of 27%. The probable reason for this case may be that surgeries were performed many years ago with underdeveloped surgery and processing methods [47]. Similarly, a meta-analysis found that autografts had better clinical outcomes compared to allografts [48-50]. These discrepancies may be due to various study populations, sampling methods, statistical analyses, and research designs applied in previous literature. If a satisfactory autograft is not accessible, or if a revision ACL reconstruction is the goal, allograft can be used as an optimal option. Factors, including previous reconstruction, surgery in another leg, tunnel size, or position are also among crucial determinants for preferring allografts to autografts. In most cases, studies concluded that allograft ACL reconstruction is a safe but more expensive option that can be considered in some conditions.
Regarding the rate of ligament rupture after ACL reconstruction, Jia and Sun found a higher rate of rupture and ACL reconstruction failure in the allograft group. They believed that a faster postoperative rehabilitation course in patients with allograft may lead them to return to sports and physical activity before complete healing, which increases the risk of reinjury among them [51]. A similar study compared the graft incorporation between two graft options in an animal model. Study results revealed that autografts incorporated faster compared to allografts [52]. This may be another reason for a risk of graft failure in allograft after ACL reconstruction, suggesting more need for conservative rehabilitation in allograft reconstruction patients. Despite these variations, no statistically significant differences were approved.
One of the contributions of the present research is to compare the joint coordination variability and magnitude between reconstructed allograft and matched healthy limb, reconstructed autograft and matched healthy limb, reconstructed autograft and allograft, and finally non-reconstructed autograft and allograft. Consistent with a study conducted by Davis, our study results revealed an increased variability in the ACL reconstruction group for several joint couplings compared to the control group. These results indicated that patients with ACL reconstruction exhibit a different coordinative function in their reconstructed lower extremity compared to the control group [17]. Kiefer et al. discriminated between athletes with and without ACL reconstruction based on intralimb coordination. The ACL reconstruction group showed higher variability for the low-frequency target oscillation. The increased variability in the mentioned group was interpreted as instability in these athletes that suggested a lower proprioceptive function post-surgery [53]. Pollard et al. also found an increased lower extremity variability in an ACL reconstruction group [18]. Consistent with Kiefer et al., researchers suggested a different neuromuscular control as a reason for a higher variability in the ACL reconstruction group. They mentioned the higher variability as a risk factor for re-injury [53].
Conclusion
Study results affirmed that in clinical decision-making regarding a direct choice between allografts and autografts, clinicians should consider the efficacy of different graft options and patients’ characteristics, and the variability of joint coordination as a vital element of movement. Movement variability is an integrated part of human motor behaviour . A decrease in joint coordination variability shows a limited movement capability in individuals, which subsequently leads to malmovement strategies in a dynamic system. Lower variability in study participants has also been associated with an increased likelihood of re-injury after the ACL construction procedure. Although our result reported no significant difference between groups in joint coordination variability, having an insight into coordinative function after ACL reconstruction will help develop rehabilitation programs after the surgery as well as minimize the re-injury risk among patients. We also suggest that scholars should conduct more robust trials with valid research designs to control the results comparing ACL reconstruction with autograft and allograft.
Limitations
This study has some limitations. First, blinding patients were not used in this research, which may increase the risk of bias. Second, our study included athletes with ACL reconstruction on either the right or left side of the body, regardless of limb dominance. Third, this research procedure is accomplished in a laboratory condition and results may be different in a field.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1398.1406).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, Supervision: Reza Salehi, Mohammad Ali Sanjari; Methodology: Kasr Kazemi; Investigation, Writing – review & editing: All authors; Writing – original draft: Kasra Kazemi, Reza Salehi; Funding acquisition, Resources: Kasra Kazemi, Reza Salehi.
Conflict of interest
The authors declared no conflict of interest.
References
- Gage BE, McIlvain NM, Collins CL, Fields SK, Comstock RD. Epidemiology of 6.6 million knee injuries presenting to United States emergency departments from 1999 through 2008. Academic Emergency Medicine. 2012; 19(4):378-85. [DOI:10.1111/j.1553-2712.2012.01315.x] [PMID]
- Myrer JW, Schulthies SS, Fellingham GW. Relative and absolute reliability of the KT-2000 arthrometer for uninjured knees. Testing at 67, 89, 134, and 178 N and manual maximum forces. The American Journal of Sports Medicine. 1996; 24(1):104-8. [DOI:10.1177/036354659602400119] [PMID]
- Holm I, Oiestad BE, Risberg MA, Aune AK. No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon-bone autograft: A randomized study with 10-year follow-up. The American Journal of Sports Medicine. 2010; 38(3):448-54. [DOI:10.1177/0363546509350301] [PMID]
- Sajovic M, Strahovnik A, Dernovsek MZ, Skaza K. Quality of life and clinical outcome comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: An 11-year follow-up of a randomized controlled trial. The American Journal of Sports Medicine. 2011; 39(10):2161-9. [DOI:10.1177/0363546511411702] [PMID]
- Zimny ML, Schutte M, Dabezies E. Mechanoreceptors in the human anterior cruciate ligament. The Anatomical Record. 1986; 214(2):204-9. [DOI:10.1002/ar.1092140216] [PMID]
- Decker LM, Moraiti C, Stergiou N, Georgoulis AD. New insights into anterior cruciate ligament deficiency and reconstruction through the assessment of knee kinematic variability in terms of nonlinear dynamics. Knee Surgery, Sports Traumatology, Arthroscopy 2011; 19(10):1620-33. [DOI:10.1007/s00167-011-1484-2] [PMID]
- Courtney CA, Rine RM. Central somatosensory changes associated with improved dynamic balance in subjects with anterior cruciate ligament deficiency. Gait Posture. 2006; 24(2):190-5. [DOI:10.1016/j.gaitpost.2005.08.006] [PMID]
- Kapreli E, Athanasopoulos S, Gliatis J, Papathanasiou M, Peeters R, Strimpakos N, et al. Anterior cruciate ligament deficiency causes brain plasticity: A functional MRI study. The American Journal of Sports Medicine. 2009; 37(12):2419-26. [DOI:10.1177/0363546509343201] [PMID]
- Moses B, Orchard J, Orchard J. Systematic review: Annual incidence of ACL injury and surgery in various populations. Research in Sports Medicine. 2012; 20(3-4):157-79. [DOI:10.1080/15438627.2012.680633] [PMID]
- Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007; 23(12):1320-5.e6. [DOI:10.1016/j.arthro.2007.07.003] [PMID]
- Swenson DM, Collins CL, Best TM, Flanigan DC, Fields SK, Comstock RD. Epidemiology of knee injuries among U.S. high school athletes, 2005/2006-2010/2011. Medicine and Science in Sports and Exercisec. 2013; 45(3):462-9. [DOI:10.1249/MSS.0b013e318277acca] [PMID] [PMCID]
- Micheo W, Hernández L, Seda C. Evaluation, management, rehabilitation, and prevention of anterior cruciate ligament injury: Current concepts. PM & R. 2010; 2(10):935-44. [DOI:10.1016/j.pmrj.2010.06.014] [PMID]
- Costa-Paz M, Ayerza MA, Tanoira I, Astoul J, Muscolo DL. Spontaneous healing in complete ACL ruptures: A clinical and MRI study. Clinical Orthopaedics and Related Research. 2012; 470(4):979-85. [DOI:10.1007/s11999-011-1933-8] [PMID] [PMCID]
- Delincé P, Ghafil D. Anterior cruciate ligament tears: Conservative or surgical treatment? A critical review of the literature. Knee Surgery, Sports Traumatology, Arthroscopy. 2012; 20(1):48-61. [DOI:10.1007/s00167-011-1614-x] [PMID]
- Kostogiannis I, Ageberg E, Neuman P, Dahlberg L, Fridén T, Roos H. Activity level and subjective knee function 15 years after anterior cruciate ligament injury: A prospective, longitudinal study of nonreconstructed patients. The American Journal of Sports Medicine. 2007; 35(7):1135-43. [DOI:10.1177/0363546507299238] [PMID]
- Hurley ET, Calvo-Gurry M, Withers D, Farrington SK, Moran R, Moran CJ. Quadriceps tendon autograft in anterior cruciate ligament reconstruction: A systematic review. Arthroscopy. 2018; 34(5):1690-8. [DOI:10.1016/j.arthro.2018.01.046] [PMID]
- Davis K, Williams JL, Sanford BA, Zucker-Levin A. Assessing lower extremity coordination and coordination variability in individuals with anterior cruciate ligament reconstruction during walking. Gait & Posture. 2019; 67:154-9. [DOI:10.1016/j.gaitpost.2018.10.010] [PMID]
- Pollard CD, Stearns KM, Hayes AT, Heiderscheit BC. Altered lower extremity movement variability in female soccer players during side-step cutting after anterior cruciate ligament reconstruction. The American Journal of Sports Medicine. 2015; 43(2):460-5. [DOI:10.1177/0363546514560153] [PMID]
- McNair PJ, Marshall RN. Landing characteristics in subjects with normal and anterior cruciate ligament deficient knee joints. Archives of Physical Medicine and Rehabilitation. 1994; 75(5):584-9. [DOI:10.1016/S0003-9993(21)01624-5] [PMID]
- Winter DA. Biomechanics and motor control of human movement. Hoboken: Wiley ; 2009. [Link]
- Lin HC, Hsu HC, Lu TW. Bilateral changes in ground reaction forces in patients with unilateral anterior cruciate ligament deficiency during stair locomotion. Journal of Mechanics. 27(3):437-45. [DOI:10.1017/jmech.2011.46]
- Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: An updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. British Journal of Sports Medicine. 2014; 48(21):1543-52. [DOI:10.1136/bjsports-2013-093398] [PMID]
- Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: A systematic review and meta-analysis. The American Journal of Sports Medicine. 2016; 44(7):1861-76. [DOI:10.1177/0363546515621554] [PMID] [PMCID]
- Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. The American Journal of Sports Medicine. 2009; 37(5):890-7.[DOI:10.1177/0363546508330143] [PMID]
- Negahban H, Mostafaee N, Sohani SM, Mazaheri M, Goharpey S, Salavati M, et al. Reliability and validity of the tegner and marx activity rating scales in Iranian patients with anterior cruciate ligament injury. Disabil Rehabil. 2011; 33(23-24):2305-10. [DOI:10.3109/09638288.2011.570409] [PMID]
- Irrgang JJ, Anderson AF, Boland AL, Harner CD, Neyret P, Richmond JC, et al. Responsiveness of the international knee documentation committee subjective knee form. The American Journal of Sports Medicine. 2006; 34(10):1567-73. [DOI:10.1177/0363546506288855] [PMID]
- Rahimi A, Nowrouzi A, Sohani SM. [The validity and reliability of the persian version of the international knee documentation committee (IKDC) questionnaire in Iranian patients after acl and meniscal surgeries (Persian)]. Archives of Rehabilitation. 2013;14(2):116-24. [Link]
- Vairo GL, Myers JB, Sell TC, Fu FH, Harner CD, Lephart SM. Neuromuscular and biomechanical landing performance subsequent to ipsilateral semitendinosus and gracilis autograft anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy. 2008; 16(1):2-14. [DOI:10.1007/s00167-007-0427-4] [PMID]
- Sanford BA, Williams JL, Zucker-Levin A, Mihalko WM. Asymmetric ground reaction forces and knee kinematics during squat after anterior cruciate ligament (ACL) reconstruction. The Knee. 2016; 23(5):820-5. [DOI:10.1016/j.knee.2015.11.001] [PMID]
- Gribbin TC, Slater LV, Herb CC, Hart JM, Chapman RM, Hertel J, et al. Differences in hip-knee joint coupling during gait after anterior cruciate ligament reconstruction. Clinical Biomechanics. 2016; 32:64-71. [DOI:10.1016/j.clinbiomech.2016.01.006] [PMID]
- Sparrow WA, Donovan E, van Emmerik R, Barry EB. Using relative motion plots to measure changes in intra-limb and inter-limb coordination. Journal of Motor Behavior. 1987; 19(1):115-29. [DOI:10.1080/00222895.1987.10735403] [PMID]
- Anderson MJ, Browning WM 3rd, Urband CE, Kluczynski MA, Bisson LJ. A systematic summary of systematic reviews on the topic of the anterior cruciate ligament. Orthopaedic Journal of Sports Medicine. 2016; 4(3):2325967116634074. [DOI:10.1177/2325967116634074] [PMID] [PMCID]
- Deehan D, Salmon LJ, Webb VJ, Davies A, Pinczewski L. Endoscopic reconstruction of the anterior cruciate ligament with an ipsilateral patellar tendon autograft. Bone & Joint Journal. 2000; 82(7):984-91. [DOI:10.1302/0301-620X.82B7.0820984]
- Wright RW, Dunn WR, Amendola A, Andrish JT, Bergfeld J, Kaeding CC, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: A prospective MOON cohort study. The American Journal of Sports Medicine. 2007; 35(7):1131-4. [DOI:10.1177/0363546507301318] [PMID]
- Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clinical Journal of Sport Medicine. 2012; 22(2):116-21. [DOI:10.1097/JSM.0b013e318246ef9e] [PMID] [PMCID]
- Poolman RW, Abouali JA, Conter HJ, Bhandari M. Overlapping systematic reviews of anterior cruciate ligament reconstruction comparing hamstring autograft with bone-patellar tendon-bone autograft: Why are they different? The Journal of Bone and Joint Surgery. American Volume. 2007; 89(7):1542-52. [DOI:10.2106/JBJS.F.01292] [PMID]
- Slone HS, Romine SE, Premkumar A, Xerogeanes JW. Quadriceps tendon autograft for anterior cruciate ligament reconstruction: A comprehensive review of current literature and systematic review of clinical results. Arthroscopy. 2015; 31(3):541-54. [DOI:10.1016/j.arthro.2014.11.010] [PMID]
- Lephart SM, Kocher MS, Harner CD, Fu FH. Quadriceps strength and functional capacity after anterior cruciate ligament reconstruction. Patellar tendon autograft versus allograft. The American Journal of Sports Medicine. 1993; 21(5):738-43. [DOI:10.1177/036354659302100519] [PMID]
- Peterson RK, Shelton WR, Bomboy AL. Allograft versus autograft patellar tendon anterior cruciate ligament reconstruction: A 5-year follow-up. Arthroscopy. 2001; 17(1):9-13. [DOI:10.1053/jars.2001.19965] [PMID]
- Balsly CR, Cotter AT, Williams LA, Gaskins BD, Moore MA, Wolfinbarger L Jr. Effect of low dose and moderate dose gamma irradiation on the mechanical properties of bone and soft tissue allografts. Cell and Tissue Banking. 2008; 9(4):289-98. [DOI:10.1007/s10561-008-9069-0] [PMID]
- Chechik O, Amar E, Khashan M, Lador R, Eyal G, Gold A. An international survey on anterior cruciate ligament reconstruction practices. International Orthopaedics. 2013; 37(2):201-6. [DOI:10.1007/s00264-012-1611-9] [PMID] [PMCID]
- Fu F, Christel P, Miller MD, Johnson DL. Graft selection for anterior cruciate ligament reconstruction. Instructional Course Lectures. 2009; 58:337-54. [PMID]
- Hu J, Qu J, Xu D, Zhou J, Lu H. Allograft versus autograft for anterior cruciate ligament reconstruction: An up-to-date meta-analysis of prospective studies. International Orthopaedics. 2013; 37(2):311-20. [DOI:10.1007/s00264-012-1720-5] [PMID] [PMCID]
- Bottoni CR, Smith EL, Shaha J, Shaha SS, Raybin SG, Tokish JM, et al. Autograft versus allograft anterior cruciate ligament reconstruction: A prospective, randomized clinical study with a minimum 10-year follow-up. The American Journal of Sports Medicine. 2015; 43(10):2501-9. [DOI:10.1177/0363546515596406] [PMID]
- Wang S, Zhang C, Cai Y, Lin X. Autograft or allograft? Irradiated or not? A contrast between autograft and allograft in anterior cruciate ligament reconstruction: A meta-analysis. Arthroscopy. 2018; 34(12):3258-65. [DOI:10.1016/j.arthro.2018.06.053] [PMID]
- Mariscalco MW, Magnussen RA, Mehta D, Hewett TE, Flanigan DC, Kaeding CC. Autograft versus nonirradiated allograft tissue for anterior cruciate ligament reconstruction: A systematic review. The American Journal of Sports Medicine. 2014; 42(2):492-9. [DOI:10.1177/0363546513497566] [PMID] [PMCID]
- Mistry H, Metcalfe A, Colquitt J, Loveman E, Smith NA, Royle P, et al. Autograft or allograft for reconstruction of anterior cruciate ligament: A health economics perspective. Knee Surgery, Sports Traumatology, Arthroscopy. 2019; 27(6):1782-90. [DOI:10.1007/s00167-019-05436-z] [PMID] [PMCID]
- Prodromos C, Joyce B, Shi K. A meta-analysis of stability of autografts compared to allografts after anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopyc. 2007; 15(7):851-6. [DOI:10.1007/s00167-007-0328-6] [PMID]
- Zeng C, Gao SG, Li H, Yang T, Luo W, Li YS, et al. Autograft versus allograft in anterior cruciate ligament reconstruction: A meta-analysis of randomized controlled trials and systematic review of overlapping systematic reviews. Arthroscopy. 2016; 32(1):153-63.e18. [DOI:10.1016/j.arthro.2015.07.027] [PMID]
- Yao LW, Wang Q, Zhang L, Zhang C, Zhang B, Zhang YJ, et al. Patellar tendon autograft versus patellar tendon allograft in anterior cruciate ligament reconstruction: A systematic review and meta-analysis. European Journal of Orthopaedic Surgery & Traumatology. 2015; 25(2):355-65. [DOI:10.1007/s00590-014-1481-5] [PMID]
- Jia YH, Sun PF. Comparison of clinical outcome of autograft and allograft reconstruction for anterior cruciate ligament tears. Chinese Medical Journal. 2015; 128(23):3163-6. [DOI:10.4103/0366-6999.170265] [PMID] [PMCID]
- Gobbi A, Francisco R. Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: A prospective clinical investigation. Knee Surgery, Sports Traumatology, Arthroscopy. 2006; 14(10):1021-8. [DOI:10.1007/s00167-006-0050-9] [PMID]
- Kiefer AW, Ford KR, Paterno MV, Schmitt LC, Myer GD, Riley MA, et al. Inter-segmental postural coordination measures differentiate athletes with ACL reconstruction from uninjured athletes. Gait & Posture. 2013; 37(2):149-53. [DOI:10.1016/j.gaitpost.2012.05.005] [PMID] [PMCID]
Type of Study: Research |
Subject:
Physiotherapy
Received: 2024/01/21 | Accepted: 2024/01/28 | Published: 2024/03/7
Received: 2024/01/21 | Accepted: 2024/01/28 | Published: 2024/03/7