Volume 6, Issue 1 (Continuously Updated 2023)
Func Disabil J 2023, 6(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kachoosangy R A, Salehi S, Almasi-Hashiani A, Beheshti S Z. The Relationship Between Balance and Fine Motor Skills in Children With Intellectual Disability. Func Disabil J 2023; 6 (1) : 275.1
URL: http://fdj.iums.ac.ir/article-1-236-en.html
URL: http://fdj.iums.ac.ir/article-1-236-en.html
1- Department of Occupational Therapy, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Department of Speech Therapy, School of Rehabilitation, Arak University of Medical Sciences, Arak, Iran.
3- Department of Epidemiology, Medicine Research Center, School of Health, Arak University of Medical Sciences, Arak, Iran.
4- Department of Occupational Therapy, School of Rehabilitation, Arak University of Medical Sciences, Arak, Iran. ,beheshti.ot@gmail.com
2- Department of Speech Therapy, School of Rehabilitation, Arak University of Medical Sciences, Arak, Iran.
3- Department of Epidemiology, Medicine Research Center, School of Health, Arak University of Medical Sciences, Arak, Iran.
4- Department of Occupational Therapy, School of Rehabilitation, Arak University of Medical Sciences, Arak, Iran. ,
Full-Text [PDF 1053 kb]
(554 Downloads)
| Abstract (HTML) (1266 Views)
Full-Text: (824 Views)
Introduction
Intellectual disability (ID) is a learning disorder that leads to an intelligence quotient (IQ) lower than 70 and defects in two or more areas of adaptive behaviors. This disorder occurs before the age of 18 years and its diagnosis is based on clinical history, level of mental ability, and level of adaptive performance [1]. Its prevalence is about 1%, which reaches 3% in school age. ID is divided into 4 categories, mild, moderate, severe, and profound based on the level of mental and adaptive function, and more than 75% of the children with ID are mild. Children with mild ID can learn reading, writing, and math up to the third to sixth grade and lead independent lives [2].
Some researchers have stated that intellectual disability can also affect other areas of development, including cognition, language, and psychosocial skills [3, 4]. Lee mentioned children with ID have more behavioral problems than other children. These behavioral problems often include attention deficit, self-harm, stereotyped behaviors, abnormal attachment, aggression, and impulsive behaviors that can prevent children with ID from participating in learning opportunities and activities of daily living (ADL) [5]. The limitations of children with ID are caused by problems in brain development [6]. Having a suitable level of motor integration can affect children’s ADL, play, education, and participation in life areas [7]. Some researchers state that children with ID have delays in gross and fine motor skills [4, 8, 9]. Sretenovic and Nedovic, after examining the movement problems of mentally disabled children, stated that the balance skills of these children are also lower than the average of other school-aged children. They suggested that corrective or preventive interventions should be considered to support and help these children perform school activities [10]. These motor defects often include defects in motor coordination, visual motor coordination, balance, and fine motor skills, so that Karande states that 27% of children with ID have postural control disorder and 92% of them have problems in fine motor skills. These children are 3 to 5 years behind other children in terms of motor development [4].
Hand as the main part of fine motor skills is effective in performing various areas of ADL and play activities as well as understanding and exploring the environment. Some studies have shown that fine motor skills have a significant relationship with social skills, self-awareness, and self-esteem in children [8, 11]. In a study of 85 children aged 6-8 years with normal development, Dehghan stated that a significant relationship was observed between fine motor skills and children’s social development. She suggested that among other effective interventions, fine motor skills can also be used to improve social skills [11].
On the other hand, balance is one of the main aspects of child movement in which children with ID experience problems [6]. Balance is defined as the ability to maintain a stable body position during various movements [10]. Children gain balance skills through ADL, games, and exercises related to this field. Correct balance performance allows the child to be aware of his position in space while moving, determine the direction and speed of his movements, and automatically correct his position and maintain his stability during various activities [12]. Postural and balance control is one of the main requirements of ADL. Acquiring, maintaining, and correcting balance during different movement situations, such as stationary and motionless positions, preparing to move, moving, and preparing to stop, are very complex abilities that are delayed and inefficient in children with ID [3, 8]. Most motor skills are developed during the preschool age, which is a critical period for learning and acquiring most movements. In this developmental period, the best way to improve motor skills is through functional exercises and exposure to suitable and sufficient balance stimuli [10].
According to the review of the studies conducted in this field, it seems that few studies have investigated the relationship between balance and fine motor skills. If this relationship exists, more comprehensive treatment programs can be used to improve each. Therefore, this study was conducted to investigate the relationship between balance and fine motor skills in children with mild intellectual disability aged 4-7 years.
Materials and Methods
Participations
The present study is a descriptive cross-sectional study. Eighty children aged 4-7 years (45 boys and 35 girls) with mild ID (intelligence quotient [IQ] 50-70) based on the school records and physician’s prescription were recruited from schools for children with special needs and occupational therapy centers in Arak City, Iran in a non-random way. They all met inclusion criteria, including the absence of any visual or hearing impairment that cannot be compensated by assistive devices, such as glasses or hearing aids, the absence of other neurological injuries, and no history of orthopedic or surgical injuries in the upper or lower limbs in the past 6 months. Those children who did not cooperate were excluded from the study. All children’s parents were asked to sign the consent form and to complete the demographic questionnaire. To maximize the response accuracy, before conducting the main assessments, the participants were familiarized with the assessment items during a short 10-minute session.
Assessment tools
Peabody developmental motor scale edition 2 (PDMS-2)
Peabody developmental motor scale edition 2 (PDMS-2) was used to evaluate fine motor skills, which examines the state of motor development of children from birth to 7 years old. This tool is not dependent on gender, race, and culture, and its validity and reliability are high in the Iranian population (0.987 for the gross motor scale and 0.971 for the fine motor scale) [13]. This is composed of 6 subtests, reflexes (birth to 11 months), stationary (all age range), locomotion (all age range), object manipulation (12 months and older), grasping (all age range), and visual motor integration (all age range). This measurement was performed by occupational therapists using standard tools. Each item depended on a performance score from 0 to 2 [14]. In this study, only fine motor skill areas, including grasping and visual motor integration (VMI) scores were collected. The grasping subtest has 26 items and the visual motor integration subtest has 72 items. At the end of the evaluation of each subtest, the score related to that subtest is recorded and the final score of fine motor skills (FMS) is obtained from the total scores of all items. Considering the high number of items evaluated and to prevent the negative effects of fatigue on the results, skills were evaluated for each participant by a tester in two sessions. The instructions for each item were first given orally and practically by the tester to each participant and then asked to do it. Depending on how each item was performed, the score was recorded on a test sheet for each participant.
Bruninks-Oseretsky test of motor proficiency (BOTMP)
The purpose of the Bruninks-Oseretsky test of motor proficiency (BOTMP) is to provide a comprehensive overview of fine and gross motor skills in school-aged children and young adults. The BOTMP can also be used to develop and evaluate motor training programs. Gharaie et al. examined the validity and reliability of the BOTMP in Iran and its reliability coefficient was reported as 0.78 [15]. This test has eight subscales, running speed and agility (1 item), balance (8 items), bilateral coordination (8 items), strength (3 items), upper limb coordination (9 items), response speed (1 item), visual motor control (8 item), and upper limb speed and dexterity (8 items). In this study, balance subscale scores were collected. The score for each item is 0 (failure) and 1 (success). Finally, the total scores of fine motor skills (TFMS) obtained in 8 items are recorded as a score of the balance subtest. Participants were allowed to perform each item twice and the best result was recorded as a result of that item.
Statistical analysis
The data were analyzed using SPSS software, version 23. It was not normally distributed (Kolmogorov-Smirnov test of normality). P<0.05 was statistically significant. Then, Spearman’s correlation coefficient was used to determine the correlation between balance with the total score of fine motor skills, VMI, and grasp. The significance level was also considered as P≤0.05.
Mean±SD, range of changes, minimum, and maximum were used to analyze descriptive variables.
Results
This study was conducted on 80 children with mild intellectual disability. Table 1 presents the demographic characteristics of the sample.
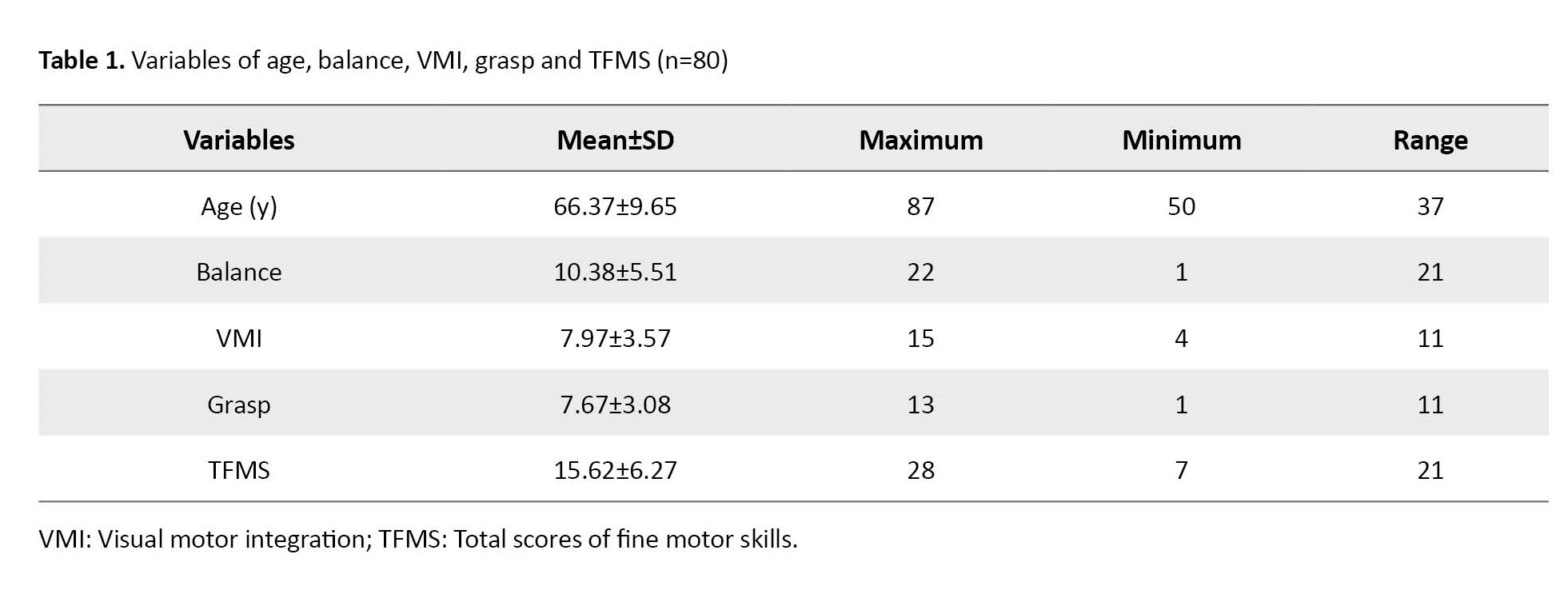
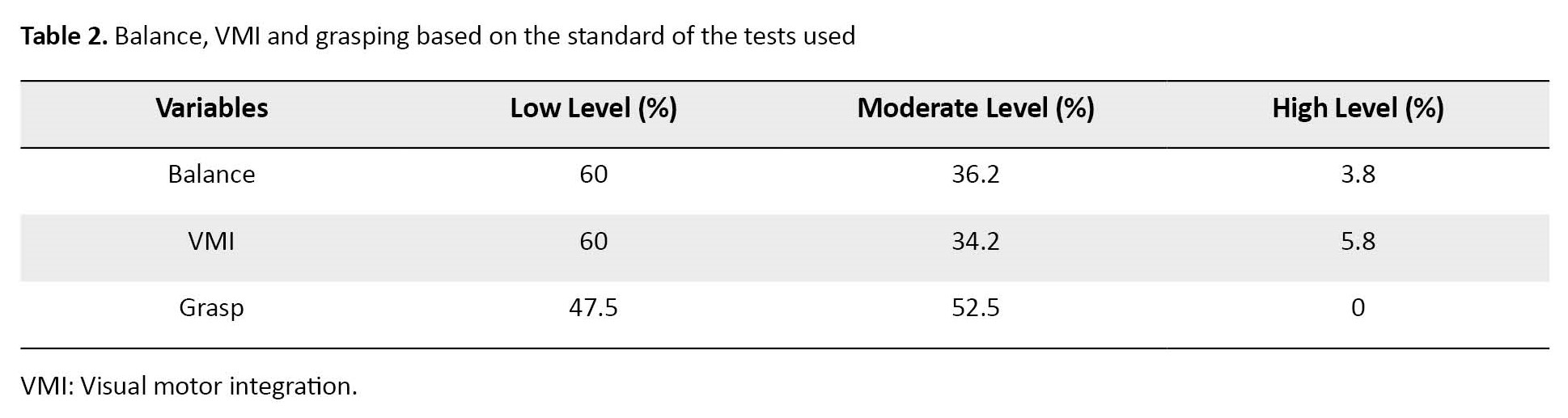
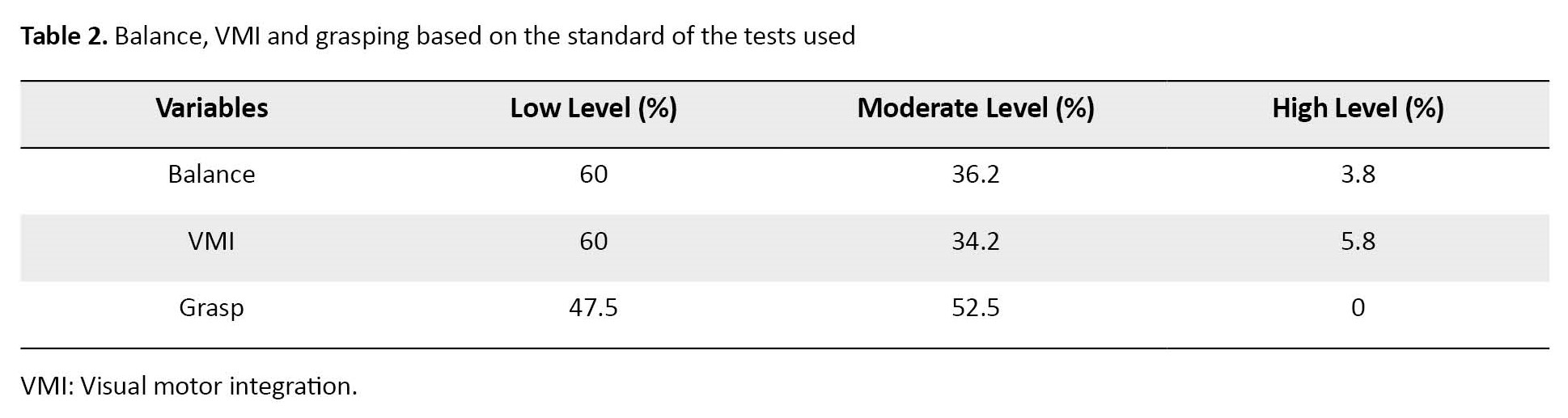
As shown, 42 female participants with an average age of 41.39±7.65 months and 38 male participants with an average age of 39.51±8.93 months participated. The Mean±SD of all variables of balance, visual motor integration, grasping and the total score of fine motor skills were 10.38±5.51, 7.97±3.57, 7.68±3.08, and 15.62±6.27. Also, the results showed that 60% of the participants were at a low level in terms of balance skills (according to the standard table of the BOTMP test). Also, 60% in terms of visual-motor integration skills and 47.5% in terms of grasping skills (according to the standard table of Peabody test) were at a low level, which is shown in Table 2.
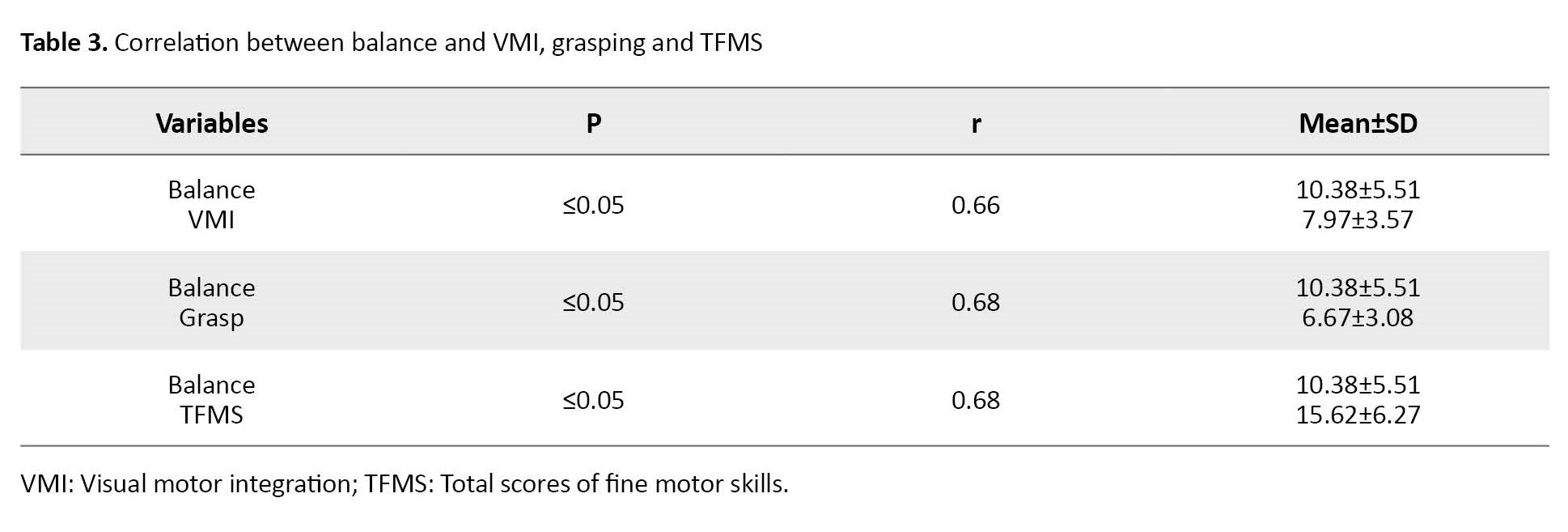
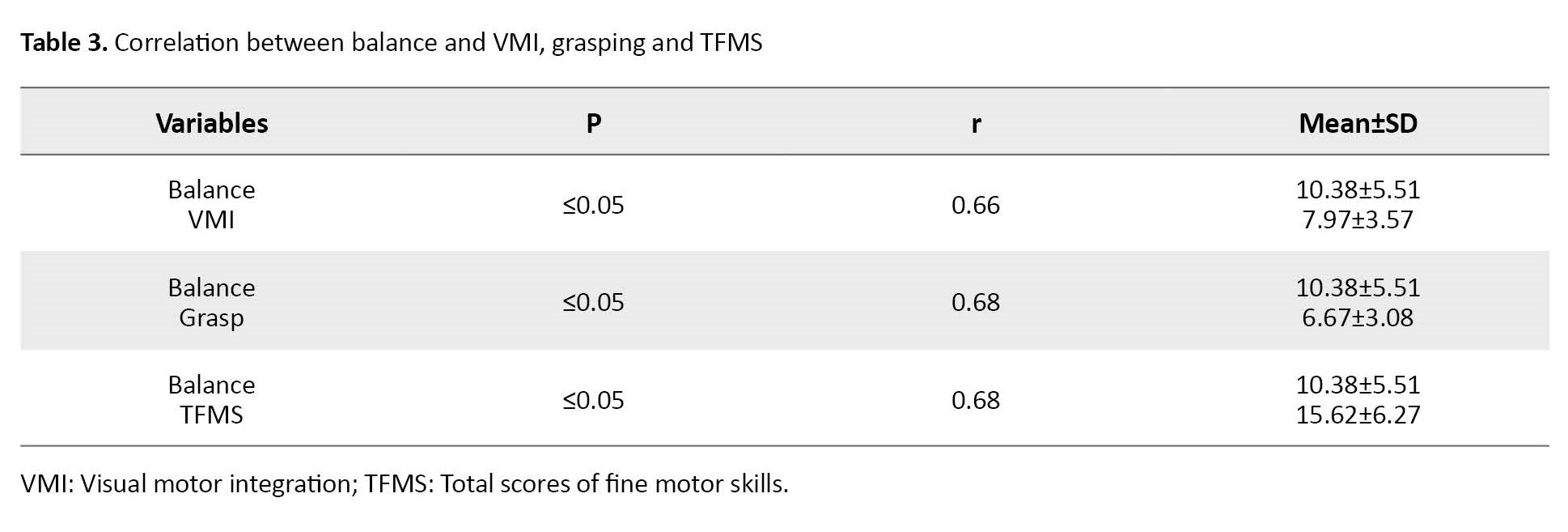
Spearman’s correlation coefficient was used to measure the relationship between balance and VMI, grasp, and TFMS. The data in Table 3 shows a significant relationship between balance and these variables (P≤0.05 for all variables).
Discussion
The present study was conducted to investigate the existence of a positive relationship between balance and VMI, grasping, and fine motor skills in children with mild ID. The results showed that 60% of the participants were at a low level in terms of balance skills, 60% in terms of VMI, and 47.5% in terms of grasping skills. The main point of this study was that a significant positive relationship is observed between all variables.
Fine motor skills are a crucial part of motor skills. Human uniqueness lies in the development of the brain and its cortex, and due to the control of the brain cortex on the complex movements of the hand, a large part of the motor cortex of the brain is dedicated to hand movements. Any degree of inability in the fine motor skills of the hand can hurt the person’s relationship with the environment. Therefore, many studies have investigated fine motor skills in different groups. Research has shown that a significant percentage of children with mental disabilities are at low levels in terms of motor skills. In 2013, Rintala examined the motor skills of 20 children with mild ID and found that children with mild ID were 3 to 4 years behind the normal group in motor skills [16]. In 2008, Wuang assessed the hand motor skills of children with mild intellectual disabilities using the motor assessment battery for children test and concluded that these children had severe hand function impairments [17]. In 2010, Vuijk et al. examined the gross and fine motor skills of children with intellectual disability and borderline mental functioning. They assessed balance, postural control, dextrity, and visual motor skills. They also concluded that these children had obvious problems in maintaining balance and controlling body position, as well as fine motor skills, which was consistent with the results of the present study [18]. Savage and Watkinson also achieved similar results [19, 20]. These results showed that children with mental disabilities who have good balance also have good movement skills. Balance ability and VMI are associated with increased accuracy and stability of eye movements that occur with age. Also, in children, the most reliable source of perceptual information for balance control is environmental information processed through visual cues [21, 22]. In 2006, Wrotniak et al. showed a positive and significant relationship between motor skills, visual motor coordination, and the development of gross motor skills in healthy adolescents [20].
Gross motor skills are movements that are performed by the large muscles of the legs, and arms and with the balance of the whole body. Fine motor skills involve finer and more precise movements performed by the smaller muscles of the hands and fingers. Gross motor skills, including balance, and fine motor skills often develop together, and more varied gross motor skills can develop fine motor skills. This positive correlation, which was also shown in the present study, can be caused by the simultaneous development of gross motor skills and fine motor skills. In 2012, Atilgan conducted a study on 9-year-old children with normal development and examined the relationship between static and dynamic balance with hand-eye coordination and bilateral hand coordination. He stated that a high positive correlation is observed between hand skills and balance in children with normal development. He suggested that in addition to strengthening gross motor skills, such as muscle strength, exercises related to improving fine motor skills can also be used to improve balance [3]. In this study, we obtained similar results regarding children with ID. Haga et al. in 2008 evaluated movement and balance components in a group of school children and reported a significant relationship between balance and manual skills [23]. Hatzitaki et al. found a significant positive relationship between balance parameters and some visual motor tests, reaction time, and depth perception, which is consistent with the results of the present study [21].
Conclusion
The results of this study showed a strong relationship between fine motor skills and balance in children with intellectual disability. This issue may affect the planning of interventions to improve any of the areas of fine motor skills or balance.
Limitation
In the field of examining the relationship between balance and fine motor skills in children with intellectual disability, limited studies were conducted, which made the interpretation of the results of the present study challenging.
Recommendation
This study was conducted only on children with mild intellectual disability. It is suggested to conduct further studies in this field in children with different degrees of mental disability as well as other disorders, such as autism spectrum disorder or developmental coordination disorder.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Arak University of Medical Sciences (Code: IR.ARAKMU.REC.1399.151). All the parents of children participating in the study read and signed a written consent form.
Funding
This article is the result of a research project (Grant No.: 3647), funded by the Research and Technology Vice-Chancellor of Arak University of Medical Sciences.
Authors' contributions
Conceptualization, Supervision: Seyedeh Zeinab Beheshti, Reihaneh Askary Kachoosangy; Methodology: AmirAlmasi‑Hashiani; Writing -reviewing & editing: All authers; Writing original draft: Sousan salehi, Seyedeh zeinab Beheshti; Funding acquisition: Seyedeh zeinab Beheshti.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors appreciate and thank the respectable management of the Arak Exceptional Education Organization.
References
Intellectual disability (ID) is a learning disorder that leads to an intelligence quotient (IQ) lower than 70 and defects in two or more areas of adaptive behaviors. This disorder occurs before the age of 18 years and its diagnosis is based on clinical history, level of mental ability, and level of adaptive performance [1]. Its prevalence is about 1%, which reaches 3% in school age. ID is divided into 4 categories, mild, moderate, severe, and profound based on the level of mental and adaptive function, and more than 75% of the children with ID are mild. Children with mild ID can learn reading, writing, and math up to the third to sixth grade and lead independent lives [2].
Some researchers have stated that intellectual disability can also affect other areas of development, including cognition, language, and psychosocial skills [3, 4]. Lee mentioned children with ID have more behavioral problems than other children. These behavioral problems often include attention deficit, self-harm, stereotyped behaviors, abnormal attachment, aggression, and impulsive behaviors that can prevent children with ID from participating in learning opportunities and activities of daily living (ADL) [5]. The limitations of children with ID are caused by problems in brain development [6]. Having a suitable level of motor integration can affect children’s ADL, play, education, and participation in life areas [7]. Some researchers state that children with ID have delays in gross and fine motor skills [4, 8, 9]. Sretenovic and Nedovic, after examining the movement problems of mentally disabled children, stated that the balance skills of these children are also lower than the average of other school-aged children. They suggested that corrective or preventive interventions should be considered to support and help these children perform school activities [10]. These motor defects often include defects in motor coordination, visual motor coordination, balance, and fine motor skills, so that Karande states that 27% of children with ID have postural control disorder and 92% of them have problems in fine motor skills. These children are 3 to 5 years behind other children in terms of motor development [4].
Hand as the main part of fine motor skills is effective in performing various areas of ADL and play activities as well as understanding and exploring the environment. Some studies have shown that fine motor skills have a significant relationship with social skills, self-awareness, and self-esteem in children [8, 11]. In a study of 85 children aged 6-8 years with normal development, Dehghan stated that a significant relationship was observed between fine motor skills and children’s social development. She suggested that among other effective interventions, fine motor skills can also be used to improve social skills [11].
On the other hand, balance is one of the main aspects of child movement in which children with ID experience problems [6]. Balance is defined as the ability to maintain a stable body position during various movements [10]. Children gain balance skills through ADL, games, and exercises related to this field. Correct balance performance allows the child to be aware of his position in space while moving, determine the direction and speed of his movements, and automatically correct his position and maintain his stability during various activities [12]. Postural and balance control is one of the main requirements of ADL. Acquiring, maintaining, and correcting balance during different movement situations, such as stationary and motionless positions, preparing to move, moving, and preparing to stop, are very complex abilities that are delayed and inefficient in children with ID [3, 8]. Most motor skills are developed during the preschool age, which is a critical period for learning and acquiring most movements. In this developmental period, the best way to improve motor skills is through functional exercises and exposure to suitable and sufficient balance stimuli [10].
According to the review of the studies conducted in this field, it seems that few studies have investigated the relationship between balance and fine motor skills. If this relationship exists, more comprehensive treatment programs can be used to improve each. Therefore, this study was conducted to investigate the relationship between balance and fine motor skills in children with mild intellectual disability aged 4-7 years.
Materials and Methods
Participations
The present study is a descriptive cross-sectional study. Eighty children aged 4-7 years (45 boys and 35 girls) with mild ID (intelligence quotient [IQ] 50-70) based on the school records and physician’s prescription were recruited from schools for children with special needs and occupational therapy centers in Arak City, Iran in a non-random way. They all met inclusion criteria, including the absence of any visual or hearing impairment that cannot be compensated by assistive devices, such as glasses or hearing aids, the absence of other neurological injuries, and no history of orthopedic or surgical injuries in the upper or lower limbs in the past 6 months. Those children who did not cooperate were excluded from the study. All children’s parents were asked to sign the consent form and to complete the demographic questionnaire. To maximize the response accuracy, before conducting the main assessments, the participants were familiarized with the assessment items during a short 10-minute session.
Assessment tools
Peabody developmental motor scale edition 2 (PDMS-2)
Peabody developmental motor scale edition 2 (PDMS-2) was used to evaluate fine motor skills, which examines the state of motor development of children from birth to 7 years old. This tool is not dependent on gender, race, and culture, and its validity and reliability are high in the Iranian population (0.987 for the gross motor scale and 0.971 for the fine motor scale) [13]. This is composed of 6 subtests, reflexes (birth to 11 months), stationary (all age range), locomotion (all age range), object manipulation (12 months and older), grasping (all age range), and visual motor integration (all age range). This measurement was performed by occupational therapists using standard tools. Each item depended on a performance score from 0 to 2 [14]. In this study, only fine motor skill areas, including grasping and visual motor integration (VMI) scores were collected. The grasping subtest has 26 items and the visual motor integration subtest has 72 items. At the end of the evaluation of each subtest, the score related to that subtest is recorded and the final score of fine motor skills (FMS) is obtained from the total scores of all items. Considering the high number of items evaluated and to prevent the negative effects of fatigue on the results, skills were evaluated for each participant by a tester in two sessions. The instructions for each item were first given orally and practically by the tester to each participant and then asked to do it. Depending on how each item was performed, the score was recorded on a test sheet for each participant.
Bruninks-Oseretsky test of motor proficiency (BOTMP)
The purpose of the Bruninks-Oseretsky test of motor proficiency (BOTMP) is to provide a comprehensive overview of fine and gross motor skills in school-aged children and young adults. The BOTMP can also be used to develop and evaluate motor training programs. Gharaie et al. examined the validity and reliability of the BOTMP in Iran and its reliability coefficient was reported as 0.78 [15]. This test has eight subscales, running speed and agility (1 item), balance (8 items), bilateral coordination (8 items), strength (3 items), upper limb coordination (9 items), response speed (1 item), visual motor control (8 item), and upper limb speed and dexterity (8 items). In this study, balance subscale scores were collected. The score for each item is 0 (failure) and 1 (success). Finally, the total scores of fine motor skills (TFMS) obtained in 8 items are recorded as a score of the balance subtest. Participants were allowed to perform each item twice and the best result was recorded as a result of that item.
Statistical analysis
The data were analyzed using SPSS software, version 23. It was not normally distributed (Kolmogorov-Smirnov test of normality). P<0.05 was statistically significant. Then, Spearman’s correlation coefficient was used to determine the correlation between balance with the total score of fine motor skills, VMI, and grasp. The significance level was also considered as P≤0.05.
Mean±SD, range of changes, minimum, and maximum were used to analyze descriptive variables.
Results
This study was conducted on 80 children with mild intellectual disability. Table 1 presents the demographic characteristics of the sample.
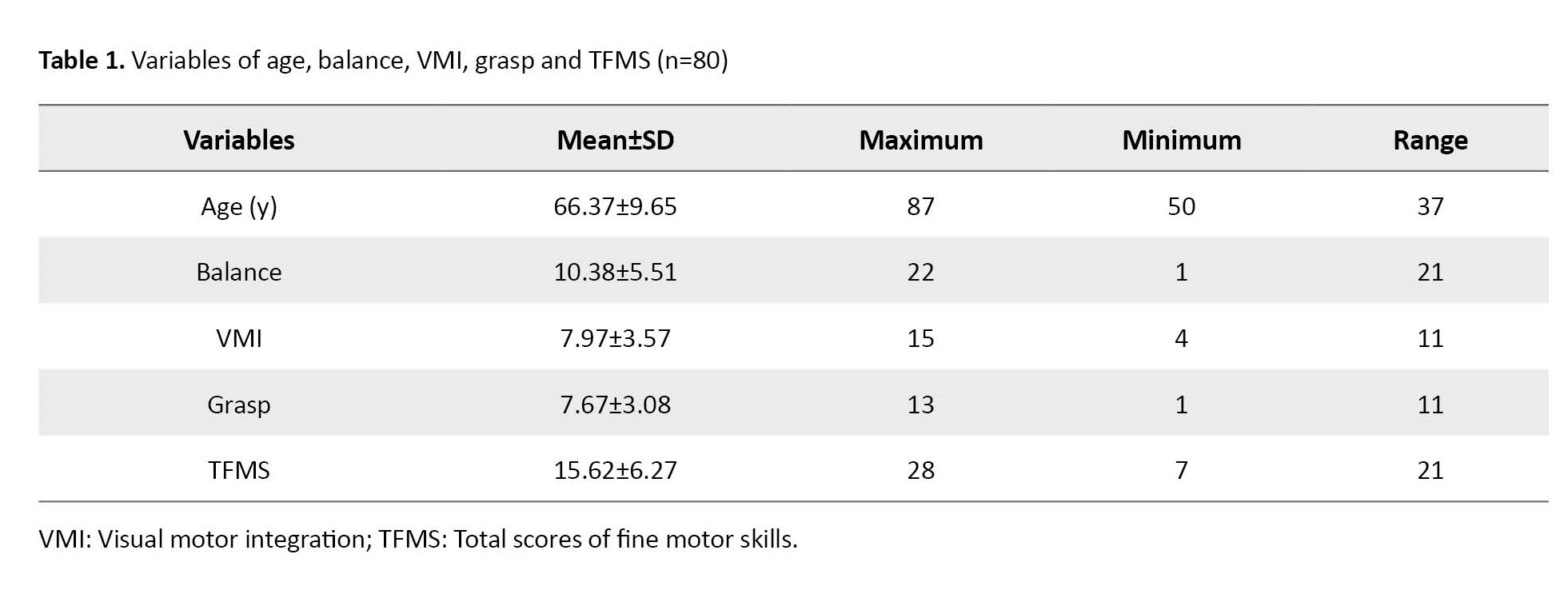
As shown, 42 female participants with an average age of 41.39±7.65 months and 38 male participants with an average age of 39.51±8.93 months participated. The Mean±SD of all variables of balance, visual motor integration, grasping and the total score of fine motor skills were 10.38±5.51, 7.97±3.57, 7.68±3.08, and 15.62±6.27. Also, the results showed that 60% of the participants were at a low level in terms of balance skills (according to the standard table of the BOTMP test). Also, 60% in terms of visual-motor integration skills and 47.5% in terms of grasping skills (according to the standard table of Peabody test) were at a low level, which is shown in Table 2.
Spearman’s correlation coefficient was used to measure the relationship between balance and VMI, grasp, and TFMS. The data in Table 3 shows a significant relationship between balance and these variables (P≤0.05 for all variables).
Discussion
The present study was conducted to investigate the existence of a positive relationship between balance and VMI, grasping, and fine motor skills in children with mild ID. The results showed that 60% of the participants were at a low level in terms of balance skills, 60% in terms of VMI, and 47.5% in terms of grasping skills. The main point of this study was that a significant positive relationship is observed between all variables.
Fine motor skills are a crucial part of motor skills. Human uniqueness lies in the development of the brain and its cortex, and due to the control of the brain cortex on the complex movements of the hand, a large part of the motor cortex of the brain is dedicated to hand movements. Any degree of inability in the fine motor skills of the hand can hurt the person’s relationship with the environment. Therefore, many studies have investigated fine motor skills in different groups. Research has shown that a significant percentage of children with mental disabilities are at low levels in terms of motor skills. In 2013, Rintala examined the motor skills of 20 children with mild ID and found that children with mild ID were 3 to 4 years behind the normal group in motor skills [16]. In 2008, Wuang assessed the hand motor skills of children with mild intellectual disabilities using the motor assessment battery for children test and concluded that these children had severe hand function impairments [17]. In 2010, Vuijk et al. examined the gross and fine motor skills of children with intellectual disability and borderline mental functioning. They assessed balance, postural control, dextrity, and visual motor skills. They also concluded that these children had obvious problems in maintaining balance and controlling body position, as well as fine motor skills, which was consistent with the results of the present study [18]. Savage and Watkinson also achieved similar results [19, 20]. These results showed that children with mental disabilities who have good balance also have good movement skills. Balance ability and VMI are associated with increased accuracy and stability of eye movements that occur with age. Also, in children, the most reliable source of perceptual information for balance control is environmental information processed through visual cues [21, 22]. In 2006, Wrotniak et al. showed a positive and significant relationship between motor skills, visual motor coordination, and the development of gross motor skills in healthy adolescents [20].
Gross motor skills are movements that are performed by the large muscles of the legs, and arms and with the balance of the whole body. Fine motor skills involve finer and more precise movements performed by the smaller muscles of the hands and fingers. Gross motor skills, including balance, and fine motor skills often develop together, and more varied gross motor skills can develop fine motor skills. This positive correlation, which was also shown in the present study, can be caused by the simultaneous development of gross motor skills and fine motor skills. In 2012, Atilgan conducted a study on 9-year-old children with normal development and examined the relationship between static and dynamic balance with hand-eye coordination and bilateral hand coordination. He stated that a high positive correlation is observed between hand skills and balance in children with normal development. He suggested that in addition to strengthening gross motor skills, such as muscle strength, exercises related to improving fine motor skills can also be used to improve balance [3]. In this study, we obtained similar results regarding children with ID. Haga et al. in 2008 evaluated movement and balance components in a group of school children and reported a significant relationship between balance and manual skills [23]. Hatzitaki et al. found a significant positive relationship between balance parameters and some visual motor tests, reaction time, and depth perception, which is consistent with the results of the present study [21].
Conclusion
The results of this study showed a strong relationship between fine motor skills and balance in children with intellectual disability. This issue may affect the planning of interventions to improve any of the areas of fine motor skills or balance.
Limitation
In the field of examining the relationship between balance and fine motor skills in children with intellectual disability, limited studies were conducted, which made the interpretation of the results of the present study challenging.
Recommendation
This study was conducted only on children with mild intellectual disability. It is suggested to conduct further studies in this field in children with different degrees of mental disability as well as other disorders, such as autism spectrum disorder or developmental coordination disorder.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Arak University of Medical Sciences (Code: IR.ARAKMU.REC.1399.151). All the parents of children participating in the study read and signed a written consent form.
Funding
This article is the result of a research project (Grant No.: 3647), funded by the Research and Technology Vice-Chancellor of Arak University of Medical Sciences.
Authors' contributions
Conceptualization, Supervision: Seyedeh Zeinab Beheshti, Reihaneh Askary Kachoosangy; Methodology: AmirAlmasi‑Hashiani; Writing -reviewing & editing: All authers; Writing original draft: Sousan salehi, Seyedeh zeinab Beheshti; Funding acquisition: Seyedeh zeinab Beheshti.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors appreciate and thank the respectable management of the Arak Exceptional Education Organization.
References
- Jeoung B. Motor proficiency differences among students with intellectual disabilities, autism, and developmental disability. J Exerc Rehabil. 2018; 14(2):275-81. [DOI:10.12965/jer.1836046.023] [PMID] [PMCID]
- McKenzie K, Milton M, Smith G, Ouellette-Kuntz H. Systematic review of the prevalence and incidence of intellectual disabilities: Current trends and issues. Curr Dev Disord Rep. 2016; 3(2):104-15. [DOI:10.1007/s40474-016-0085-7]
- Atilgan OE. Relationships between perceptual-motor skills and postural balance in nine years old boys. Educ Res Rev. 2012; 7(24):517-25. [DOI:10.5897/ERR12.082]
- Karande S, Kanchan S, Kulkarni M. Clinical and psychoeducational profile of children with borderline intellectual functioning. Indian J Pediatr. 2008; 75(8):795-800. [DOI:10.1007/s12098-008-0101-y] [PMID]
- Lee Y, Jeoung B. The relationship between the behavior problems and motor skills of students with intellectual disability. J Exerc Rehabil. 2016; 12(6):598-603. [DOI:10.12965/jer.1632854.427] [PMID] [PMCID]
- Enkelaar L, Smulders E, van Schrojenstein Lantman-de Valk H, Geurts AC, Weerdesteyn V. A review of balance and gait capacities in relation to falls in persons with intellectual disability. Res Dev Disabl. 2012; 33(1):291-306. [DOI:10.1016/j.ridd.2011.08.028] [PMID]
- Houwen S, Visser L, van der Putten A, Vlaskamp C. The interrelationships between motor, cognitive, and language development in children with and without intellectual and developmental disabilities. Res Dev Disabl. 2016; 53-54:19-31. [DOI:10.1016/j.ridd.2016.01.012] [PMID]
- Piek JP, Baynam GB, Barrett NC. The relationship between fine and gross motor ability, self-perceptions and self-worth in children and adolescents. Hum Mov Sci. 2006; 25(1):65-75. [DOI:10.1016/j.humov.2005.10.011] [PMID]
- Hartman E, Houwen S, Scherder E, Visscher C. On the relationship between motor performance and executive functioning in children with intellectual disabilities. J Intellect Disabil Res. 2010; 54(5):468-77. [DOI:10.1111/j.1365-2788.2010.01284.x] [PMID]
- Sretenović I, Nedović G, Đorđević S. Assessment of balance in younger school age children with intellectual disability. Phys Educ Sport. 2018; 16(3):687-96. [DOI:10.22190/FUPES171010061S]
- Dehghan L, Mirzakhani N, Rezaee M, Tabatabaee M. The relationship between fine motor skills and social development and maturation. Iran Rehabil J. 2017; 15(4):407-14. [DOI:10.29252/nrip.irj.15.4.407]
- Mao HY, Kuo LC, Yang AL, Su CT. Balance in children with attention deficit hyperactivity disorder-combined type. Res Dev Disabl. 2014; 35(6):1252-8. [DOI:10.1016/j.ridd.2014.03.020] [PMID]
- Derakhshan-Rad SAR, Sazmand AH. [Standardization of peabody developmental motor scales in children aged 60-71 months in Shiraz (Persian)]. Arch Rehabil. 2011; 11(4):35-41. [Link]
- Naserizade A, Raji P, Mousavi ST, Hakim Shoushtari M, Baghestani A. [Comparison of motor skills in At-risk with autism spectrum disorder children with autism spectrum disorder and typical development children (Persian)]. J Med Counc Iran. 2019; 37(4):242-8. [Link]
- Gharaei E, Shojaei M, Daneshfar A. The validity and reliability of the bruininks–oseretsky test of motor proficiency, 2nd edition brief form, in preschool children. Ann Appl Sport Sci. 2019; 7(2):3-12. [DOI:10.29252/aassjournal.7.2.3]
- Rintala P, Loovis EM. Measuring motor skills in Finnish children with intellectual disabilities. Percept Mot Skills. 2013; 116(1):294-303. [DOI:10.2466/25.10.PMS.116.1.294-303] [PMID]
- Wuang YP, Wang CC, Huang MH, Su CY. Profiles and cognitive predictors of motor functions among early school-age children with mild intellectual disabilities. J Intellect Disabil Res. 2008; 52(12):1048-60. [DOI:10.1111/j.1365-2788.2008.01096.x] [PMID]
- Vuijk PJ, Hartman E, Scherder E, Visscher C. Motor performance of children with mild intellectual disability and borderline intellectual functioning. J Intellect Disabil Res. 2010; 54(11):955-65. [DOI:10.1111/j.1365-2788.2010.01318.x] [PMID]
- Savage R. Cerebellar tasks do not distinguish between children with developmental dyslexia and children with intellectual disability. Child Neuropsychol. 2007; 13(5):389-407. [DOI:10.1080/13825580600966375] [PMID]
- Wrotniak BH, Epstein LH, Dorn JM, Jones KE, Kondilis VA. The relationship between motor proficiency and physical activity in children. Pediatrics. 2006; 118(6):e1758-65. [DOI:10.1542/peds.2006-0742] [PMID]
- Hatzitaki V, Zisi V, Kollias I, Kioumourtzoglou E. Perceptual-motor contributions to static and dynamic balance control in children. J Mot Behav. 2002; 34(2):161-70. [DOI:10.1080/00222890209601938] [PMID]
- Mallau S, Vaugoyeau M, Assaiante C. Postural strategies and sensory integration: No turning point between childhood and adolescence. Plos One. 2010; 5(9):e13078. [DOI:10.1371/journal.pone.0013078] [PMID] [PMCID]
- Haga M. The relationship between physical fitness and motor competence in children. Child. 2008; 34(3):329-34. [DOI:10.1111/j.1365-2214.2008.00814.x] [PMID]
Type of Study: Research |
Subject:
Occupational Therapy
Received: 2023/12/2 | Accepted: 2024/01/7 | Published: 2023/02/7
Received: 2023/12/2 | Accepted: 2024/01/7 | Published: 2023/02/7