Volume 6, Issue 1 (Continuously Updated 2023)
Func Disabil J 2023, 6(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Lajevardi L, Taghizadeh G, Azad A, Ahmadi A S. Predictive Role of Ankle Muscle Strength, Pain and Activity Level in Ankle Functional Instability, Functional Mobility and Gait Speed in Individuals With Ankle Sprain. Func Disabil J 2023; 6 (1) : 268.1
URL: http://fdj.iums.ac.ir/article-1-232-en.html
URL: http://fdj.iums.ac.ir/article-1-232-en.html
1- Department of Occupational Therapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 1134 kb]
(260 Downloads)
| Abstract (HTML) (345 Views)
Full-Text: (81 Views)
Introduction
An ankle sprain is one of the most common musculoskeletal injuries so that many previous studies show that it includes about 10%-15% of all musculoskeletal injuries and 85% of athletes have experienced it at least once [1, 2]. Sprains can be external, internal, and syndesmotic, and can cause different symptoms and intensities of pain, inflammation, lower limb function, ankle functional instability, and functional mobility reduction [2, 3]. Impaired walking following injuries, such as ankle sprains severely reduces the quality of life and functional activity levels of individuals with ankle sprain injuries. In previous studies, injured students walk at least 2 100 steps less than healthy students during the day and cannot return to their workplace or school for a week [4, 5].
Many factors can predict functional mobility, walking speed, and ankle functional instability in individuals with ankle sprain. Strong evidence showed that ankle muscle strength has a significant effect on ankle functional instability, functional mobility, and walking speed in other lower limb orthopedic injuries [6-8]. In previous studies, the main cause of reduced walking speed, reduced functional mobility, and functional ankle instability in people with ankle sprains, decreased ankle muscle strength (isometric and concentric strength of ankle plantar flexors), and pain have been reported [9-13]. Pain can slow down walking and cause abnormal changes in walking [14]. The condition of ankle sprain (acute, sub-acute, and chronic sprain) can also predict the functional mobility of individuals with ankle sprain. Acute and chronic ankle sprains were considered to be crucial predictors of reduced functional mobility and can also affect the strength of trunk and hip muscles [4, 15-17].
So far, many studies have conducted the predictive role of various factors, such as history of ankle sprain, severity of sprain, and number of sprains, but none of the studies conducted so far have exclusively studied the predictive role of various factors. Among others, ankle muscle strength, pain, and activity level have not been investigated simultaneously in ankle instability, functional mobility, and walking speed in people with ankle sprain. From this point of view, this study was conducted to investigate the crucial and key effects of muscle strength, pain, and the level of activity of the individual in wide areas, including ankle instability, functional mobility, and walking speed in this common orthopedic injury.
Materials and Methods
In this study, the sample size was determined with a power of 80% and an error of 5%, and the calculations were done using SPSS software, version 22. First, 10 individuals with ankle sprain were evaluated as a pilot study, and according to the statistical data analysis obtained from the pilot study, the sample size was determined to be 140 people. Sampling was done from those who were referred to medical centers in Shiraz City.
The inclusion criteria included having an ankle sprain as diagnosed by an orthopedic specialist and medical records in the past year, at least 18 to 65 years old, scoring 24≥ in the mini-mental state examination (MMSE) to read and write Persian language and executing simple verbal commands, not suffering from neurological diseases (stroke, concussion, etc.) and other orthopedic diseases in the spine and lower limbs, except ankle sprains, including all acute and chronic degrees. It was based on the doctor’s diagnosis and the person’s report. The exclusion criteria included the patient’s non-cooperation during the test, neurological and orthopedic diseases during the test re-test interval, and the patient’s failure to return to the re-test session.
All the questionnaires and tests were conducted in a quiet hall with adequate ventilation and light and without any sharp objects, on a smooth and non-slip surface, between 4:00 PM to 10:00 PM. The order of the tests was random.
To collect data, a demographic questionnaire was used, including information, such as the duration of sprain, age, etc. Also, the manual muscle test (MMT), visual analogue scale (VAS), Persian version of the Tegner activity scale (TAS), identification of functional ankle instability (IDFAI), timed up and go (TUG), the gait speed test and MMSE were used to evaluate ankle muscle strength, pain, activity level, ankle functional instability, functional mobility, gait speed, and cognitive level, respectively:
Mini-mental state examination (MMSE)
It is a cognitive test for the elderly that takes about 5 to 10 minutes to complete. The maximum score is 30 and to enter the study, people must have a minimum score of 24 to read and execute simple verbal commands [18-21]. Construct validity, convergent validity and reliability of this test have also been reported [22].
Demographic questionnaire
This questionnaire is about the personal and demographic information of the samples, including the affected side, the duration of the disease, the direction of the sprain, the severity of the sprain, age, sex, height, the history of ankle sprain in the past year, the type of shoes at the time of the injury (loose/no lodge), education level, use/non-use of medication and other personal information, such as contact number, address and name of physician.
Manual muscle test (MMT)
Clinical evaluations of muscle function in patients with ankle sprains are often performed by relying on manual muscle strength measurement methods [5]. This test is used to evaluate the muscle strength of all types of neurological and orthopedic patients, and its reliability has been proven in various studies on patients with various orthopedic and neurological disorders [23, 24]. The diagnosis method is that the examiner gives instructions to the desired muscle to the examinee and calculates the strength of each muscle based on the following values, if there was no contraction, score 0, if muscle contraction was felt but no movement was seen, score 1, if movement was performed with the help of the examiner and in the state of removal of gravity, score 2, if the movement of the person was performed independently and with the removal of gravity, score 3, if the contraction was done with the tester’s moderate resistance, score 4, and if it was with the tester’s maximum resistance, score 5 is given [25].
Visual analogue scale (VAS)
It is a self-report instrument aimed at assessing pain intensity in clinical and research settings. The examinee should mark the intensity of his pain on an axis of 10 cm long, the closer to the beginning of the axis, the less pain he has, and the more he marks toward the end of the axis, the more intense pain he feels. This tool is effective in patients with acute and chronic pain, cancer, rheumatoid arthritis, and orthopedic diseases. The psychometric properties of this tool were also reported to be excellent [26, 27].
Tegner activity scale (TAS)
This test is used to grade the activity level of patients with various knee and ankle problems and has been psychometrically evaluated [28-30]. The test taker should rate his work and sports activities between 0 and 10 before and after the injury. Zero means inability to perform an activity and 10 means maximum performance in performing that activity (such as the players of the national football team) [29].
Identification of functional ankle instability (IDFAI)
This self-report test has 10 questions related to ankle instability, and the higher the personal score, the greater the functional instability of the ankle. The maximum score of this test is 37 and the minimum score is zero, and if the score is 10 or less, it indicates the absence of functional instability of the ankle [31]. The psychometric properties of this test have been investigated in Iran in individuals with ankle sprain and its high validity and reliability have been reported [32].
Timed up and go (TUG)
This test was designed to evaluate the mobility, balance, and movement performance of the elderly with balance disorders. This test is effective in people with Parkinson’s disease, elderly people with or without cognitive problems, lower limb amputations, cardiovascular diseases, hip fractures, rheumatoid arthritis, and osteoarthritis [33, 34]. The timing of this test starts from the time of the command to start moving and ends when the person sits down. In the elderly population, obtaining a score of less than 10 s means complete independence, less than 20 s means the ability to do most of the work alone inside and outside the home, and a score of more than 30 s means dependence in doing most of the activities. The reliability and validity of this test have been reported high [33, 35].
Gait speed
Walking speed has always been one of the most common evaluation tools in clinical environments to check the quality of walking and also to determine normal and abnormal walking and has been used as a gold standard to evaluate the validity results of many studies conducted in different patients [36-38]. The basis of scoring in this tool is time. A person’s walking speed was obtained by dividing the distance traveled by the person by the walking time. The distance traveled by a person in these studies is 2 to 20 m, and the most common distances whose validity and reliability have been checked in orthopedic and neurology patients were 6 m, 8 m, and 10 m [38-40].
Statistical methods
In this study, the Kolmograph Smirnov test was used to check the normality distribution. Multiple regression models were used to investigate the relationship between predictors and outcomes of ankle functional instability, functional mobility, and walking speed. The significance level in this study was 0.05 [41]. The obtained data were analyzed using SPSS software, version 22.
Results
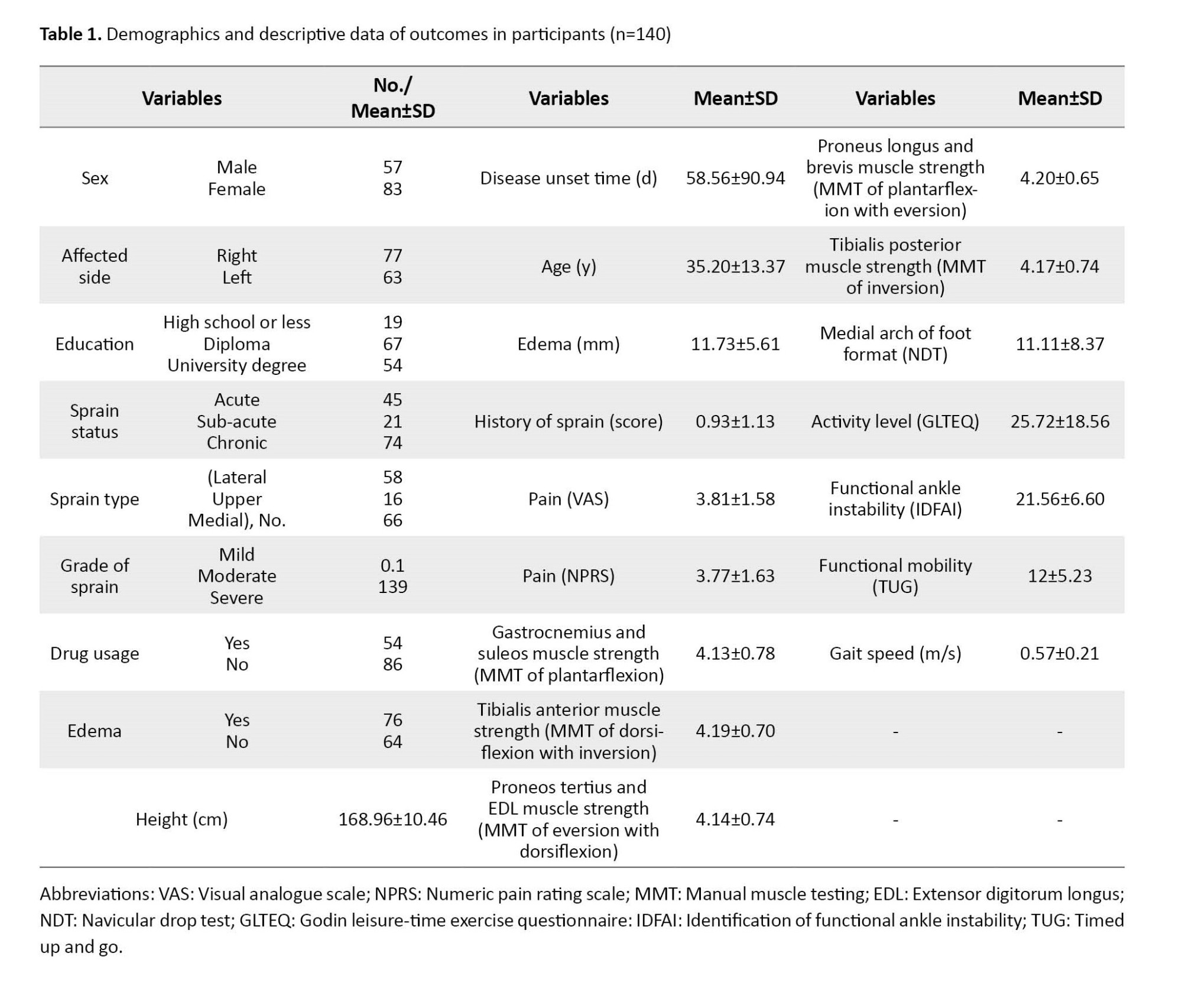
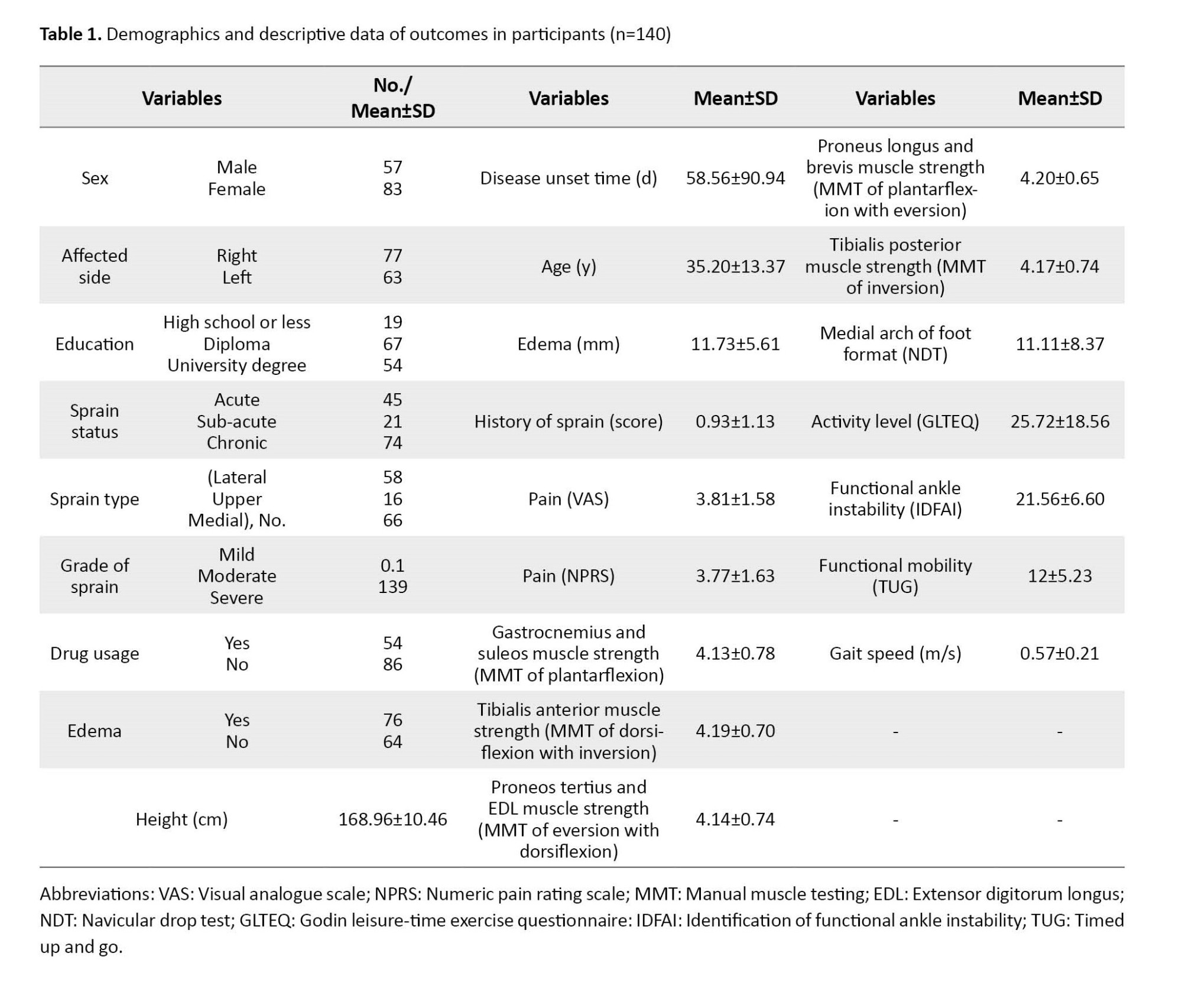
In this study, 140 samples (57 men and 83 women) participated with a Mean±SD age of 35.20±13.37 years and with a Mean±SD of the time elapsed since ankle sprain was 55.96±75.48 days. Table 1 presents demographic and clinical descriptive information.
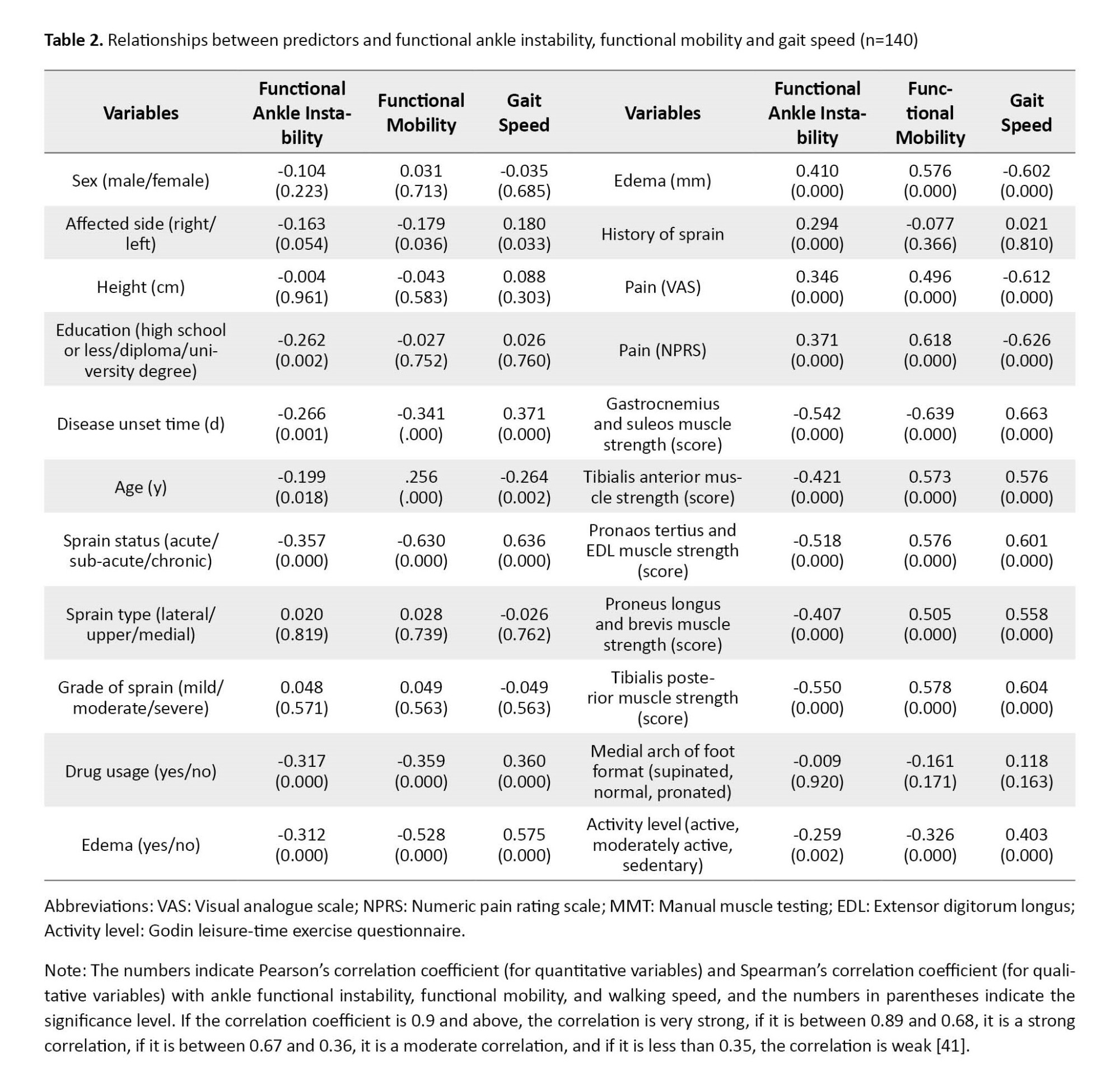
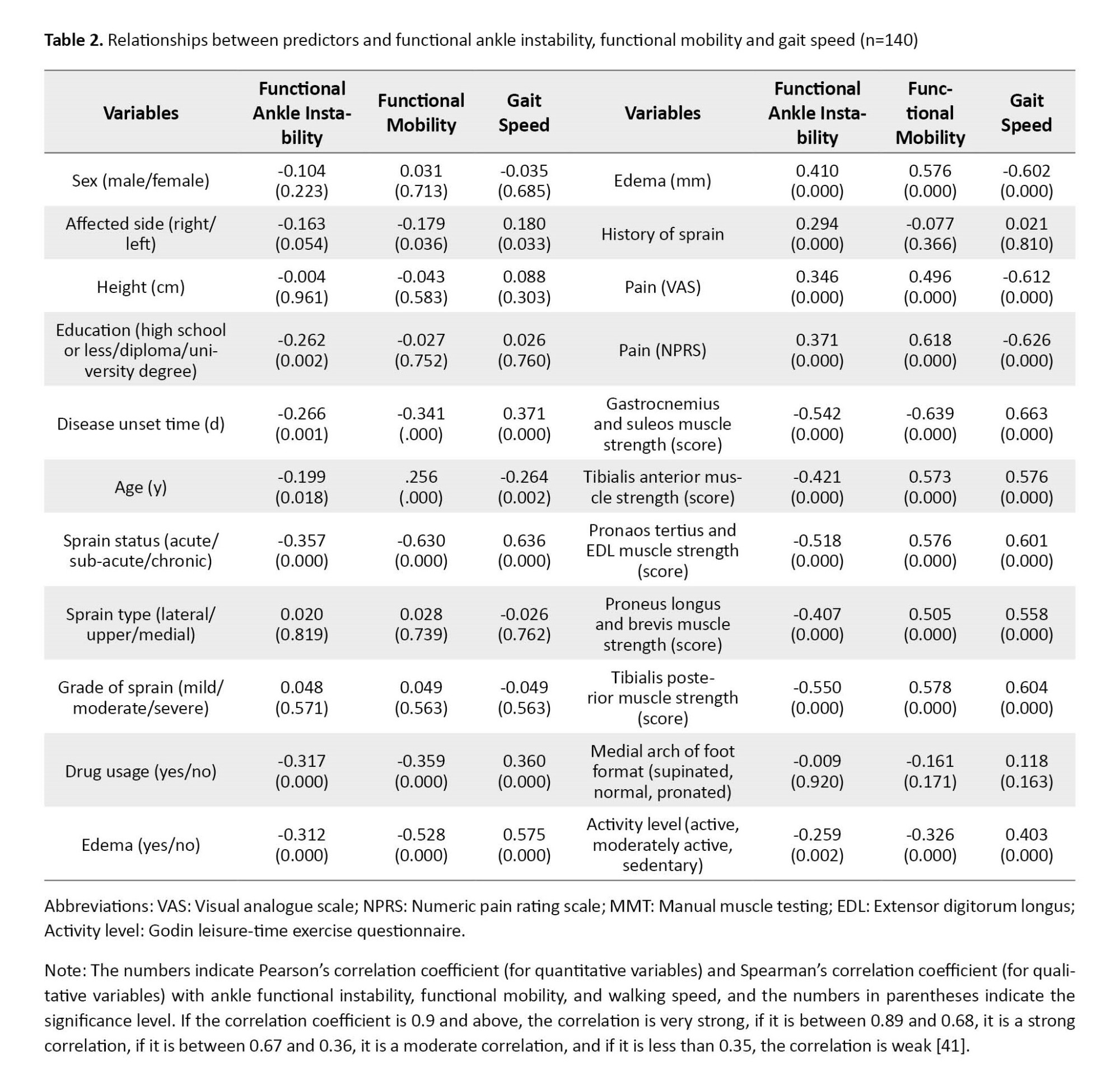
The results of the study showed a significant relationship between the affected leg, the time elapsed since sprain, age, state of sprain, use of medication, degree of swelling, pain, the strength of soleus and gastrocnemius, tibialis anterior, pronaos tertius, extensor digitorum longus, pronaos longus and brevis and tibialis posterior, the amount of medial arch of the foot, the level of physical activity with the results of functional instability of the ankle, functional mobility, and gait speed. In addition, a significant relationship was observed between the level of education and history of sprain in the last year with the degree of ankle functional instability (Table 2).
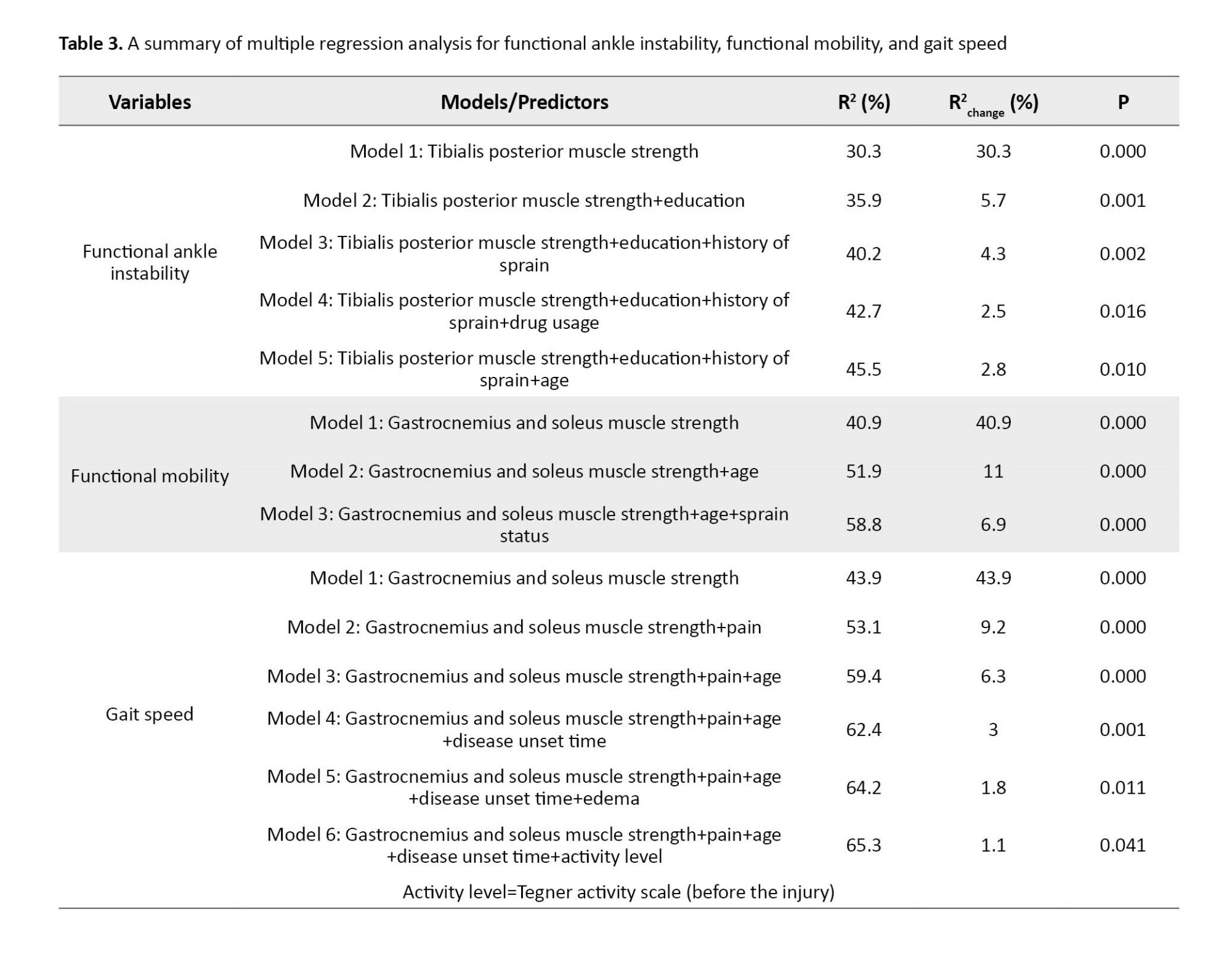
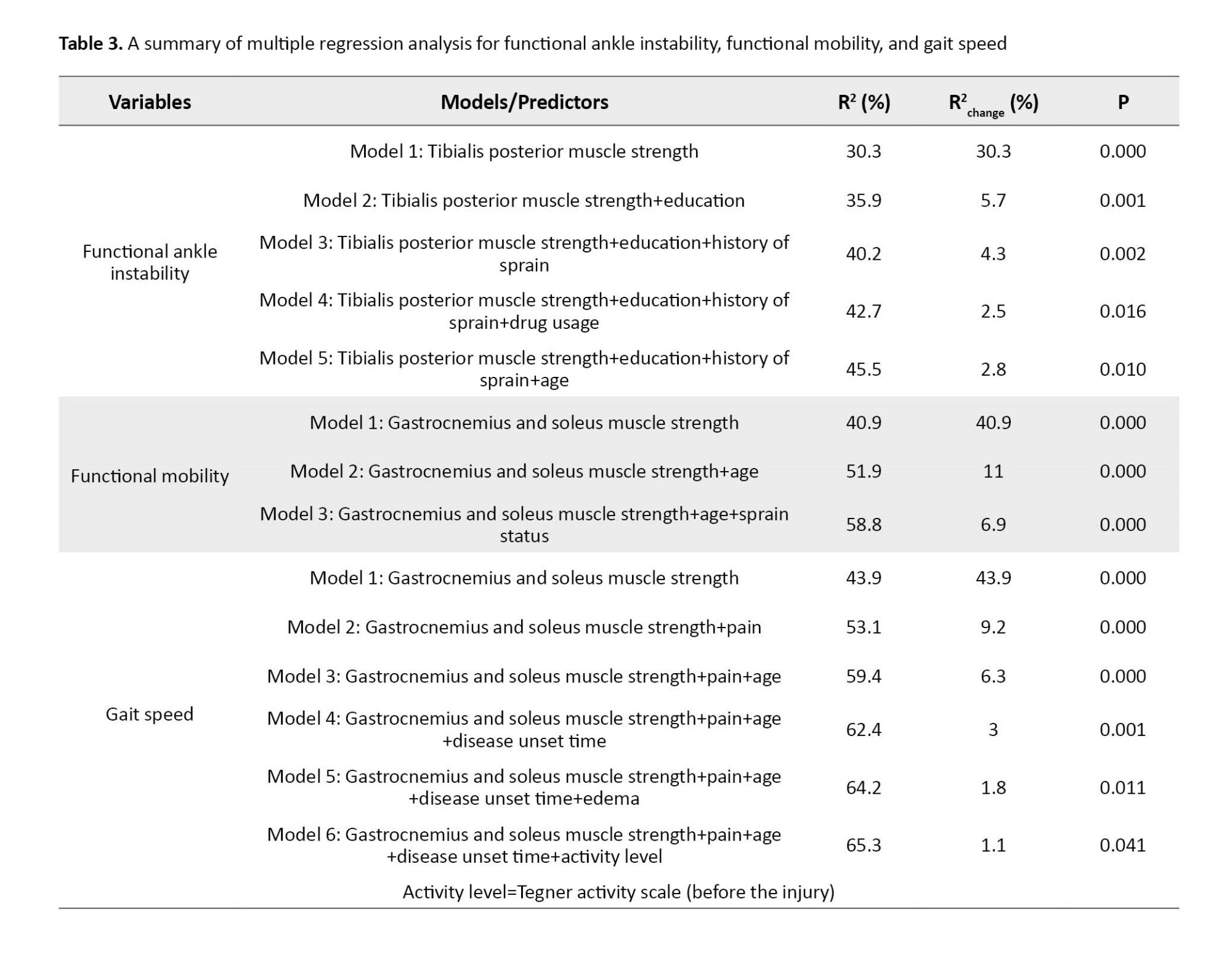
In the regression models, the predictive value for each outcome of ankle functional instability, functional mobility, and walking speed was obtained as 45.5%, 58.8%, and 65.3% of the variance, respectively. In all step models, ankle muscle strength (tibialis posterior muscle strength for ankle functional instability and soleus and gastrocnemius muscle strength for functional mobility, and gait speed) was the strongest predictor for the outcomes of ankle functional instability, functional mobility, and walking speed. For the outcome of ankle functional instability, education level, history of sprain in the last year, taking medication, and age were the second, third, fourth, and fifth crucial predictive factors, respectively. For the outcome of functional mobility, age, and sprain status were ranked as the second and third crucial predictive factors, respectively, and for the outcome of walking speed, pain factors, age, duration of illness, swelling, and physical activity level were the second, third, fourth, and fifth predictive factors, respectively (Table 3).
Discussion
This study was conducted to investigate the predictive role of ankle muscle strength, pain, and activity level in ankle functional instability, functional mobility, and gait speed in people with ankle sprains. Posterior tibialis muscle strength was the strongest predictor for functional ankle instabilities (Table 3). Letafatkar et al have mentioned the decrease in ankle muscle strength as the main cause of ankle functional instability [42]. In other studies, reduced ankle muscle strength leads to ankle functional instability [7, 8]. Education level was the second-highest predictor of functional ankle instability (Table 3). Corbett et al stated that education level is a critical determinant of evidence-based care and that people with more education have fewer sprains than others. Ankles and in case of injury due to having scientific information about how to perform timely and necessary actions after the injury, will have a faster recovery period [18].
Bulathsinhala et al. also stated that education level is one of the factors affecting functional ankle instability in the US military community and that soldiers who have more than a high school education are less likely to be seriously injured and separated from the military due to ankle sprains [19].
Having a history of ankle sprain in the last year was the third critical factor predicting ankle functional instability. One of the most common injury factors and predictors of ankle sprains in past articles is the history of ankle sprains in the last year. Having a history of at least one sprain in the last year is more effective than having a history of sprains up to two years or more than the last two years [5, 43, 44].
Age was the last predictor of ankle functional instability. Waterman and Pour Kazemi also reported that age is one of the crucial predictors of ankle functional instability [17, 20].
In this study, the strength of ankle plantar flexor muscles (gastrocnemius and soleus) was the first predictive factor of functional mobility. Meta-analysis studies showed that disturbances in the concentric strength of the ankle muscles of people with ankle sprains have been observed during plantar flexion and continuous eversion movements, which subsequently reduced their functional mobility [12, 13]. Other studies have also proven that a decrease in ankle muscle strength leads to a decrease in functional mobility in these people [7, 8]. Also, research has been conducted on the strength of the gastrocnemius and soleus muscles and it has been reported that the strength of isometric contraction of plantar flexion in people with ankle instability was lower than in healthy people [9, 10], and in the present study, the lowest strength was recorded for plantar flexors (gastrocnemius and soleus) among all ankle muscles. Age was obtained as the second predicting factor of functional mobility. With age, joint flexibility and muscle strength decrease, the ankle becomes prone to injury, and functional mobility decreases following injury [45]. In several studies, age has been reported as one of the main causes of reduced functional mobility in sprains [17, 45].
Ankle sprain status (acute/sub-acute/chronic) was the third crucial predictor of functional mobility. Severe sprains (grade two and three) up to the first 15 days after the injury are called acute sprains, up to 5 weeks after the injury are called sub-acute sprains, and more than 5 weeks after the injury are called chronic sprains [46-49]. Previous studies have proven that if the sprain condition is chronic, then the strength of the hip muscles decreases and the functional mobility decreases too [7, 16]. McCann et al. reported that chronic ankle sprains lead to decreased lumbopelvic stability and decreased trunk muscle strength during functional activities [8]. According to the study conducted by Hertel, students with chronic sprains walk at least 2 100 steps less than healthy students during the day [5]. Miklovich et al stated the condition of acute ankle sprain as a critical predictor of reduced functional mobility and added that after the injury, movement patterns change during functional activities [15].
In this study, the strength of the ankle plantar flexor muscles (gastrocnemius and soleus) was found to be the first predictor of gait speed, and the strength of the mentioned muscles was reduced especially in the plantar flexion movement after an ankle sprain. This evidence indicated the special role of ankle muscle strength in improving walking speed in people with ankle sprains. Previous studies have proven that the main reason for the decrease in gait speed in these people is the decrease in ankle muscle strength [11, 16]. Pain was the second vital predictor of walking speed reduction after ankle muscle strength. Pain is one of the crucial symptoms in most chronic musculoskeletal diseases. Most patients with chronic ankle instability seek treatment due to persistent pain. Melzack’s neuro matrix theory of pain showed that in chronic pain conditions, the cause of pain is not exclusively related to the impulses produced by sensory nerves following injury, swelling, or other injuries at the site of injury [50], but the main cause of pain is the neuro matrix outputs. The neuro matrix is a neural network that is widely distributed in the brain and chronic mental and physical stress with chronic pain can also reduce the patient’s ability and interest to engage in functional activities [51]. Therefore, many factors affect a person’s feeling of pain. In the past, extensive studies have been conducted on the relationship between pain and gait speed.
Pont and Armand have pointed out the effect of pain on reducing gait speed [11, 14]. Age was the third predictor of walking speed. Previous studies reported that walking speed decreases with age in people with ankle sprains [16, 45]. Substituting hip movements instead of knee bending is one of the main causes of walking speed reduction due to aging [52]. The duration of the sprain was the fourth crucial predictor of walking speed. Willems, Pourkazmi, and Hertel reported that the closer the time of the last injury to the ankle, the more likely the functional instability of the ankle is, and the more likely the person is to lose their foot due to the recent injury placed inside the plaster and functional mobility and gait speed decrease due to the use of aids, such as casts [5, 17, 43]. The person’s activity level before the injury was obtained as the last significant predictor of gait speed.
Previous studies showed that the higher the level of activity before the injury, the higher the probability of injury, and the lower the gait speed after the injury [11, 15]. Although in our study, the activity level was a predictor of walking speed, some other studies have mentioned the activity level as a predictor of ankle functional instability [17, 21]. In other studies, conflicts exist in the research results, for example, Holland et al. reported that the activity level of rural adolescents with sprained ankles was higher than the activity level of healthy rural adolescents [44], while Donavan et al. reported no significant difference between the level of physical activity of adolescents with functional ankle instability and healthy adolescents [53]. According to the researcher, since in many ankle sprain studies, the activity level of individuals was recorded by self-report tests [5], the activity level may be reported exaggeratedly and caused errors in the evaluation.
However, the present study had some limitations that should be considered in future studies. We recommend that in future studies, all the evaluations performed on the affected leg should be performed on the healthy leg so that information related to both legs can be obtained and compared. Also, other information, such as the ankle sprain mechanism should be investigated, whether the person’s foot was injured during sports or daily life activities. In this way, the prevalence percentage of ankle sprain in the athletes of the society can also be obtained.
Conclusion
The results of this study showed that the strength of the tibialis posterior muscle, the education level, having a history of sprain in the last year, and age were the vital factors predicting the functional instability of the ankle. Also, plantar flexor muscle strength, age, and sprain status were respectively the vital predictors of functional mobility. And finally, plantar flexor muscle strength, pain, age, duration of sprain, and activity level before the injury were also vital predictors of walking speed.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1400.1238). All participants read the consent form and agreed.
Funding
The paper was extracted from the master's thesis of Amir Seyedahmadi, approved by Department of Occupational Therapy, School of Rehabilitation Sciences, Iran University of Medical Sciences.
Authors' contributions
Conceptualization: Laleh Lajevardi, Ghorban Taghizadeh and Amir Seyedahmadi; Methodology:Ghorban Taghizadeh and Laleh Lajevardi; Investigation: Amir Seyedahmadi; Writing, review & editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors express their gratitude to the copyright holder for providing the questionnaire and to all the patients who participated in the study.
References
An ankle sprain is one of the most common musculoskeletal injuries so that many previous studies show that it includes about 10%-15% of all musculoskeletal injuries and 85% of athletes have experienced it at least once [1, 2]. Sprains can be external, internal, and syndesmotic, and can cause different symptoms and intensities of pain, inflammation, lower limb function, ankle functional instability, and functional mobility reduction [2, 3]. Impaired walking following injuries, such as ankle sprains severely reduces the quality of life and functional activity levels of individuals with ankle sprain injuries. In previous studies, injured students walk at least 2 100 steps less than healthy students during the day and cannot return to their workplace or school for a week [4, 5].
Many factors can predict functional mobility, walking speed, and ankle functional instability in individuals with ankle sprain. Strong evidence showed that ankle muscle strength has a significant effect on ankle functional instability, functional mobility, and walking speed in other lower limb orthopedic injuries [6-8]. In previous studies, the main cause of reduced walking speed, reduced functional mobility, and functional ankle instability in people with ankle sprains, decreased ankle muscle strength (isometric and concentric strength of ankle plantar flexors), and pain have been reported [9-13]. Pain can slow down walking and cause abnormal changes in walking [14]. The condition of ankle sprain (acute, sub-acute, and chronic sprain) can also predict the functional mobility of individuals with ankle sprain. Acute and chronic ankle sprains were considered to be crucial predictors of reduced functional mobility and can also affect the strength of trunk and hip muscles [4, 15-17].
So far, many studies have conducted the predictive role of various factors, such as history of ankle sprain, severity of sprain, and number of sprains, but none of the studies conducted so far have exclusively studied the predictive role of various factors. Among others, ankle muscle strength, pain, and activity level have not been investigated simultaneously in ankle instability, functional mobility, and walking speed in people with ankle sprain. From this point of view, this study was conducted to investigate the crucial and key effects of muscle strength, pain, and the level of activity of the individual in wide areas, including ankle instability, functional mobility, and walking speed in this common orthopedic injury.
Materials and Methods
In this study, the sample size was determined with a power of 80% and an error of 5%, and the calculations were done using SPSS software, version 22. First, 10 individuals with ankle sprain were evaluated as a pilot study, and according to the statistical data analysis obtained from the pilot study, the sample size was determined to be 140 people. Sampling was done from those who were referred to medical centers in Shiraz City.
The inclusion criteria included having an ankle sprain as diagnosed by an orthopedic specialist and medical records in the past year, at least 18 to 65 years old, scoring 24≥ in the mini-mental state examination (MMSE) to read and write Persian language and executing simple verbal commands, not suffering from neurological diseases (stroke, concussion, etc.) and other orthopedic diseases in the spine and lower limbs, except ankle sprains, including all acute and chronic degrees. It was based on the doctor’s diagnosis and the person’s report. The exclusion criteria included the patient’s non-cooperation during the test, neurological and orthopedic diseases during the test re-test interval, and the patient’s failure to return to the re-test session.
All the questionnaires and tests were conducted in a quiet hall with adequate ventilation and light and without any sharp objects, on a smooth and non-slip surface, between 4:00 PM to 10:00 PM. The order of the tests was random.
To collect data, a demographic questionnaire was used, including information, such as the duration of sprain, age, etc. Also, the manual muscle test (MMT), visual analogue scale (VAS), Persian version of the Tegner activity scale (TAS), identification of functional ankle instability (IDFAI), timed up and go (TUG), the gait speed test and MMSE were used to evaluate ankle muscle strength, pain, activity level, ankle functional instability, functional mobility, gait speed, and cognitive level, respectively:
Mini-mental state examination (MMSE)
It is a cognitive test for the elderly that takes about 5 to 10 minutes to complete. The maximum score is 30 and to enter the study, people must have a minimum score of 24 to read and execute simple verbal commands [18-21]. Construct validity, convergent validity and reliability of this test have also been reported [22].
Demographic questionnaire
This questionnaire is about the personal and demographic information of the samples, including the affected side, the duration of the disease, the direction of the sprain, the severity of the sprain, age, sex, height, the history of ankle sprain in the past year, the type of shoes at the time of the injury (loose/no lodge), education level, use/non-use of medication and other personal information, such as contact number, address and name of physician.
Manual muscle test (MMT)
Clinical evaluations of muscle function in patients with ankle sprains are often performed by relying on manual muscle strength measurement methods [5]. This test is used to evaluate the muscle strength of all types of neurological and orthopedic patients, and its reliability has been proven in various studies on patients with various orthopedic and neurological disorders [23, 24]. The diagnosis method is that the examiner gives instructions to the desired muscle to the examinee and calculates the strength of each muscle based on the following values, if there was no contraction, score 0, if muscle contraction was felt but no movement was seen, score 1, if movement was performed with the help of the examiner and in the state of removal of gravity, score 2, if the movement of the person was performed independently and with the removal of gravity, score 3, if the contraction was done with the tester’s moderate resistance, score 4, and if it was with the tester’s maximum resistance, score 5 is given [25].
Visual analogue scale (VAS)
It is a self-report instrument aimed at assessing pain intensity in clinical and research settings. The examinee should mark the intensity of his pain on an axis of 10 cm long, the closer to the beginning of the axis, the less pain he has, and the more he marks toward the end of the axis, the more intense pain he feels. This tool is effective in patients with acute and chronic pain, cancer, rheumatoid arthritis, and orthopedic diseases. The psychometric properties of this tool were also reported to be excellent [26, 27].
Tegner activity scale (TAS)
This test is used to grade the activity level of patients with various knee and ankle problems and has been psychometrically evaluated [28-30]. The test taker should rate his work and sports activities between 0 and 10 before and after the injury. Zero means inability to perform an activity and 10 means maximum performance in performing that activity (such as the players of the national football team) [29].
Identification of functional ankle instability (IDFAI)
This self-report test has 10 questions related to ankle instability, and the higher the personal score, the greater the functional instability of the ankle. The maximum score of this test is 37 and the minimum score is zero, and if the score is 10 or less, it indicates the absence of functional instability of the ankle [31]. The psychometric properties of this test have been investigated in Iran in individuals with ankle sprain and its high validity and reliability have been reported [32].
Timed up and go (TUG)
This test was designed to evaluate the mobility, balance, and movement performance of the elderly with balance disorders. This test is effective in people with Parkinson’s disease, elderly people with or without cognitive problems, lower limb amputations, cardiovascular diseases, hip fractures, rheumatoid arthritis, and osteoarthritis [33, 34]. The timing of this test starts from the time of the command to start moving and ends when the person sits down. In the elderly population, obtaining a score of less than 10 s means complete independence, less than 20 s means the ability to do most of the work alone inside and outside the home, and a score of more than 30 s means dependence in doing most of the activities. The reliability and validity of this test have been reported high [33, 35].
Gait speed
Walking speed has always been one of the most common evaluation tools in clinical environments to check the quality of walking and also to determine normal and abnormal walking and has been used as a gold standard to evaluate the validity results of many studies conducted in different patients [36-38]. The basis of scoring in this tool is time. A person’s walking speed was obtained by dividing the distance traveled by the person by the walking time. The distance traveled by a person in these studies is 2 to 20 m, and the most common distances whose validity and reliability have been checked in orthopedic and neurology patients were 6 m, 8 m, and 10 m [38-40].
Statistical methods
In this study, the Kolmograph Smirnov test was used to check the normality distribution. Multiple regression models were used to investigate the relationship between predictors and outcomes of ankle functional instability, functional mobility, and walking speed. The significance level in this study was 0.05 [41]. The obtained data were analyzed using SPSS software, version 22.
Results
In this study, 140 samples (57 men and 83 women) participated with a Mean±SD age of 35.20±13.37 years and with a Mean±SD of the time elapsed since ankle sprain was 55.96±75.48 days. Table 1 presents demographic and clinical descriptive information.
The results of the study showed a significant relationship between the affected leg, the time elapsed since sprain, age, state of sprain, use of medication, degree of swelling, pain, the strength of soleus and gastrocnemius, tibialis anterior, pronaos tertius, extensor digitorum longus, pronaos longus and brevis and tibialis posterior, the amount of medial arch of the foot, the level of physical activity with the results of functional instability of the ankle, functional mobility, and gait speed. In addition, a significant relationship was observed between the level of education and history of sprain in the last year with the degree of ankle functional instability (Table 2).
In the regression models, the predictive value for each outcome of ankle functional instability, functional mobility, and walking speed was obtained as 45.5%, 58.8%, and 65.3% of the variance, respectively. In all step models, ankle muscle strength (tibialis posterior muscle strength for ankle functional instability and soleus and gastrocnemius muscle strength for functional mobility, and gait speed) was the strongest predictor for the outcomes of ankle functional instability, functional mobility, and walking speed. For the outcome of ankle functional instability, education level, history of sprain in the last year, taking medication, and age were the second, third, fourth, and fifth crucial predictive factors, respectively. For the outcome of functional mobility, age, and sprain status were ranked as the second and third crucial predictive factors, respectively, and for the outcome of walking speed, pain factors, age, duration of illness, swelling, and physical activity level were the second, third, fourth, and fifth predictive factors, respectively (Table 3).
Discussion
This study was conducted to investigate the predictive role of ankle muscle strength, pain, and activity level in ankle functional instability, functional mobility, and gait speed in people with ankle sprains. Posterior tibialis muscle strength was the strongest predictor for functional ankle instabilities (Table 3). Letafatkar et al have mentioned the decrease in ankle muscle strength as the main cause of ankle functional instability [42]. In other studies, reduced ankle muscle strength leads to ankle functional instability [7, 8]. Education level was the second-highest predictor of functional ankle instability (Table 3). Corbett et al stated that education level is a critical determinant of evidence-based care and that people with more education have fewer sprains than others. Ankles and in case of injury due to having scientific information about how to perform timely and necessary actions after the injury, will have a faster recovery period [18].
Bulathsinhala et al. also stated that education level is one of the factors affecting functional ankle instability in the US military community and that soldiers who have more than a high school education are less likely to be seriously injured and separated from the military due to ankle sprains [19].
Having a history of ankle sprain in the last year was the third critical factor predicting ankle functional instability. One of the most common injury factors and predictors of ankle sprains in past articles is the history of ankle sprains in the last year. Having a history of at least one sprain in the last year is more effective than having a history of sprains up to two years or more than the last two years [5, 43, 44].
Age was the last predictor of ankle functional instability. Waterman and Pour Kazemi also reported that age is one of the crucial predictors of ankle functional instability [17, 20].
In this study, the strength of ankle plantar flexor muscles (gastrocnemius and soleus) was the first predictive factor of functional mobility. Meta-analysis studies showed that disturbances in the concentric strength of the ankle muscles of people with ankle sprains have been observed during plantar flexion and continuous eversion movements, which subsequently reduced their functional mobility [12, 13]. Other studies have also proven that a decrease in ankle muscle strength leads to a decrease in functional mobility in these people [7, 8]. Also, research has been conducted on the strength of the gastrocnemius and soleus muscles and it has been reported that the strength of isometric contraction of plantar flexion in people with ankle instability was lower than in healthy people [9, 10], and in the present study, the lowest strength was recorded for plantar flexors (gastrocnemius and soleus) among all ankle muscles. Age was obtained as the second predicting factor of functional mobility. With age, joint flexibility and muscle strength decrease, the ankle becomes prone to injury, and functional mobility decreases following injury [45]. In several studies, age has been reported as one of the main causes of reduced functional mobility in sprains [17, 45].
Ankle sprain status (acute/sub-acute/chronic) was the third crucial predictor of functional mobility. Severe sprains (grade two and three) up to the first 15 days after the injury are called acute sprains, up to 5 weeks after the injury are called sub-acute sprains, and more than 5 weeks after the injury are called chronic sprains [46-49]. Previous studies have proven that if the sprain condition is chronic, then the strength of the hip muscles decreases and the functional mobility decreases too [7, 16]. McCann et al. reported that chronic ankle sprains lead to decreased lumbopelvic stability and decreased trunk muscle strength during functional activities [8]. According to the study conducted by Hertel, students with chronic sprains walk at least 2 100 steps less than healthy students during the day [5]. Miklovich et al stated the condition of acute ankle sprain as a critical predictor of reduced functional mobility and added that after the injury, movement patterns change during functional activities [15].
In this study, the strength of the ankle plantar flexor muscles (gastrocnemius and soleus) was found to be the first predictor of gait speed, and the strength of the mentioned muscles was reduced especially in the plantar flexion movement after an ankle sprain. This evidence indicated the special role of ankle muscle strength in improving walking speed in people with ankle sprains. Previous studies have proven that the main reason for the decrease in gait speed in these people is the decrease in ankle muscle strength [11, 16]. Pain was the second vital predictor of walking speed reduction after ankle muscle strength. Pain is one of the crucial symptoms in most chronic musculoskeletal diseases. Most patients with chronic ankle instability seek treatment due to persistent pain. Melzack’s neuro matrix theory of pain showed that in chronic pain conditions, the cause of pain is not exclusively related to the impulses produced by sensory nerves following injury, swelling, or other injuries at the site of injury [50], but the main cause of pain is the neuro matrix outputs. The neuro matrix is a neural network that is widely distributed in the brain and chronic mental and physical stress with chronic pain can also reduce the patient’s ability and interest to engage in functional activities [51]. Therefore, many factors affect a person’s feeling of pain. In the past, extensive studies have been conducted on the relationship between pain and gait speed.
Pont and Armand have pointed out the effect of pain on reducing gait speed [11, 14]. Age was the third predictor of walking speed. Previous studies reported that walking speed decreases with age in people with ankle sprains [16, 45]. Substituting hip movements instead of knee bending is one of the main causes of walking speed reduction due to aging [52]. The duration of the sprain was the fourth crucial predictor of walking speed. Willems, Pourkazmi, and Hertel reported that the closer the time of the last injury to the ankle, the more likely the functional instability of the ankle is, and the more likely the person is to lose their foot due to the recent injury placed inside the plaster and functional mobility and gait speed decrease due to the use of aids, such as casts [5, 17, 43]. The person’s activity level before the injury was obtained as the last significant predictor of gait speed.
Previous studies showed that the higher the level of activity before the injury, the higher the probability of injury, and the lower the gait speed after the injury [11, 15]. Although in our study, the activity level was a predictor of walking speed, some other studies have mentioned the activity level as a predictor of ankle functional instability [17, 21]. In other studies, conflicts exist in the research results, for example, Holland et al. reported that the activity level of rural adolescents with sprained ankles was higher than the activity level of healthy rural adolescents [44], while Donavan et al. reported no significant difference between the level of physical activity of adolescents with functional ankle instability and healthy adolescents [53]. According to the researcher, since in many ankle sprain studies, the activity level of individuals was recorded by self-report tests [5], the activity level may be reported exaggeratedly and caused errors in the evaluation.
However, the present study had some limitations that should be considered in future studies. We recommend that in future studies, all the evaluations performed on the affected leg should be performed on the healthy leg so that information related to both legs can be obtained and compared. Also, other information, such as the ankle sprain mechanism should be investigated, whether the person’s foot was injured during sports or daily life activities. In this way, the prevalence percentage of ankle sprain in the athletes of the society can also be obtained.
Conclusion
The results of this study showed that the strength of the tibialis posterior muscle, the education level, having a history of sprain in the last year, and age were the vital factors predicting the functional instability of the ankle. Also, plantar flexor muscle strength, age, and sprain status were respectively the vital predictors of functional mobility. And finally, plantar flexor muscle strength, pain, age, duration of sprain, and activity level before the injury were also vital predictors of walking speed.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1400.1238). All participants read the consent form and agreed.
Funding
The paper was extracted from the master's thesis of Amir Seyedahmadi, approved by Department of Occupational Therapy, School of Rehabilitation Sciences, Iran University of Medical Sciences.
Authors' contributions
Conceptualization: Laleh Lajevardi, Ghorban Taghizadeh and Amir Seyedahmadi; Methodology:Ghorban Taghizadeh and Laleh Lajevardi; Investigation: Amir Seyedahmadi; Writing, review & editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors express their gratitude to the copyright holder for providing the questionnaire and to all the patients who participated in the study.
References
- Garrick JG. The frequency of injury, mechanism of injury, and epidemiology of ankle sprains. Am J Sports Med. 1977; 5(6):241-2. [DOI:10.1177/036354657700500606] [PMID]
- Herzog MM, Kerr ZY, Marshall SW, Wikstrom EA. Epidemiology of ankle sprains and chronic ankle instability. J Athl Train. 2019; 54(6):603-10. [DOI:10.4085/1062-6050-447-17] [PMID] [PMCID]
- Binkley JM, Stratford PW, Lott SA, Riddle DL; North American Orthopaedic Rehabilitation Research Network. The Lower Extremity Functional Scale (LEFS): Scale development, measurement properties, and clinical application. Phys Ther. 1999; 79(4):371-83. [DOI:10.1037/t35109-000]
- Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: A systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014; 44(1):123-40. [DOI:10.1007/s40279-013-0102-5] [PMID]
- Hertel J, Corbett RO. An updated model of chronic ankle instability. J Athl Train. 2019; 54(6):572-88. [DOI:10.4085/1062-6050-344-18] [PMID] [PMCID]
- Han S, Cheng G, Xu P. Three-dimensional lower extremity kinematics of Chinese during activities of daily living. J Back Musculoskelet Rehabil. 2015; 28(2):327-34. [DOI:10.3233/BMR-140523] [PMID]
- McCann RS, Bolding BA, Terada M, Kosik KB, Crossett ID, Gribble PA. Isometric hip strength and dynamic stability of individuals with chronic ankle instability. J Athl Train. 2018; 53(7):672-8. [DOI:10.4085/1062-6050-238-17] [PMID] [PMCID]
- McCann RS, Johnson K, Suttmiller AMB. Lumbopelvic stability and trunk muscle contractility of individuals with chronic ankle instability. Int J Sports Phys Ther. 2021; 16(3):741-8. [DOI:10.26603/001c.22132] [PMID] [PMCID]
- Fraser JJ, Koldenhoven RM, Jaffri AH, Park JS, Saliba SF, Hart JM, et al. Foot impairments contribute to functional limitation in individuals with ankle sprain and chronic ankle instability. Knee Surg Sports Traumatol Arthrosc. 2020; 28:1600-10. [DOI:10.1007/s00167-018-5028-x] [PMID]
- Donnelly L, Donovan L, Hart JM, Hertel J. Eversion strength and surface electromyography measures with and without chronic ankle instability measured in 2 positions. Foot Ankle Int. 2017; 38(7):769-78. [DOI:10.1177/1071100717701231] [PMID]
- Punt IM, Ziltener JL, Laidet M, Armand S, Allet L. Gait and physical impairments in patients with acute ankle sprains who did not receive physical therapy. PM R. 2015; 7(1):34-41. [DOI:10.1016/j.pmrj.2014.06.014] [PMID]
- Arnold BL, Linens SW, de la Motte SJ, Ross SE. Concentric evertor strength differences and functional ankle instability: A meta-analysis. J Athl Train. 2009; 44(6):653-62. [DOI:10.4085/1062-6050-44.6.653] [PMID] [PMCID]
- Thompson C, Schabrun S, Romero R, Bialocerkowski A, van Dieen J, Marshall P. Factors contributing to chronic ankle instability: A systematic review and meta-analysis of systematic reviews. Sports Med. 2018; 48(1):189-205 [DOI:10.1007/s40279-017-0781-4] [PMID]
- Punt IM, Armand S, Ziltener JL, Allet L. Effect of Wii Fit™ exercise therapy on gait parameters in ankle sprain patients: A randomized controlled trial. Gait Posture. 2017; 58:52-8. [DOI:10.1016/j.gaitpost.2017.06.284] [PMID]
- Miklovic TM, Donovan L, Protzuk OA, Kang MS, Feger MA. Acute lateral ankle sprain to chronic ankle instability: A pathway of dysfunction. Phys Sportsmed. 2018; 46(1):116-22. [DOI:10.1080/00913847.2018.1409604] [PMID]
- DeJong AF, Koldenhoven RM, Hart JM, Hertel J. Gluteus medius dysfunction in females with chronic ankle instability is consistent at different walking speeds. Clin Biomech (Bristol, Avon). 2020; 73:140-8. [DOI:10.1016/j.clinbiomech.2020.01.013] [PMID]
- Pourkazemi F, Hiller CE, Raymond J, Nightingale EJ, Refshauge KM. Predictors of chronic ankle instability after an index lateral ankle sprain: A systematic review. J Sci Med Sport. 2014; 17(6):568-73. [DOI:10.1016/j.jsams.2014.01.005] [PMID]
- Corbett RO, Harris PC, Vela L, Saliba SA, Hertel J. Athletic trainers' perceptions of treating and managing patients with ankle sprains. J Athl Train. 2021; 56(9):967-72. [DOI:10.4085/325-20] [PMID] [PMCID]
- Bulathsinhala L, Hill OT, Scofield DE, Haley TF, Kardouni JR. Epidemiology of ankle sprains and the risk of separation from service in U.S. Army soldiers. J Orthop Sports Phys Ther. 2015 Jun;45(6):477-84. [DOI:10.2519/jospt.2015.5733] [PMID]
- Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ Jr. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010; 92(13):2279-84. [DOI:10.2106/JBJS.I.01537] [PMID]
- Doherty C, Bleakley C, Hertel J, Caulfield B, Ryan J, Delahunt E. Recovery from a first-time lateral ankle sprain and the predictors of chronic ankle instability: A prospective cohort analysis. Am J Sports Med. 2016; 44(4):995-1003. [DOI:10.1177/0363546516628870] [PMID]
- Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975; 12(3):189-98. [DOI:10.1016/0022-3956(75)90026-6] [PMID]
- Schmitt WH Jr, Cuthbert SC. Common errors and clinical guidelines for manual muscle testing: "The arm test" and other inaccurate procedures. Chiropr Osteopat. 2008; 16:16. [DOI:10.1186/1746-1340-16-16] [PMID] [PMCID]
- Florence JM, Pandya S, King WM, Robison JD, Baty J, Miller JP, et al. Intrarater reliability of manual muscle test (Medical Research Council Scale) grades in Duchenne's muscular dystrophy. Phys Ther. 1992; 72(2):115-22; discussion 122-6. [DOI:10.1093/ptj/72.2.115] [PMID]
- Avers D, Brown M. Daniels and Worthingham’s Muscle Testing, first South Asia edition e book: Techniques of manual examination and performance testing; Amsterdam: Elsevier; 2018. [Link]
- DeLoach LJ, Higgins MS, Caplan AB, Stiff JL. The visual analog scale in the immediate postoperative period: Intrasubject variability and correlation with a numeric scale. Anesth Analg. 1998; 86(1):102-6. [DOI:10.1097/00000539-199801000-00020]
- Collins SL, Moore RA, McQuay HJ. The visual analogue pain intensity scale: What is moderate pain in millimetres? Pain. 1997; 72(1-2):95-7. [DOI:10.1016/S0304-3959(97)00005-5] [PMID]
- Negahban H, Mostafaee N, Sohani SM, Mazaheri M, Goharpey S, Salavati M, et al. Reliability and validity of the Tegner and Marx activity rating scales in Iranian patients with anterior cruciate ligament injury. Disability and rehabilitation. 2011; 33(22-23):2305-10. [DOI:10.3109/09638288.2011.570409] [PMID]
- Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985; 198:42-9. [DOI:10.1097/00003086-198509000-00007]
- Halasi T, Kynsburg A, Tállay A, Berkes I. Development of a new activity score for the evaluation of ankle instability. Am J Sports Med. 2004; 32(4):899-908. [DOI:10.1177/0363546503262181] [PMID]
- Simon J, Donahue M, Docherty C. Development of the Identification of Functional Ankle Instability (IdFAI). Foot Ankle Int. 2012; 33(9):755-63. [DOI:10.3113/FAI.2012.0755] [PMID]
- Mohamadi S, Dadgoo M, Ebrahimi I, Salavati M, Saeedi A, Valiollahi B. Translation, cross-cultural adaptation, reliability, and validity of the Identification of Functional Ankle Instability Questionnaire in Persian speaking participants with a history of ankle sprain. Disabil Rehabil. 2019; 41(16):1931-6. [DOI:10.1080/09638288.2018.1452053] [PMID]
- Podsiadlo D, Richardson S. The timed "Up & Go": A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991; 39(2):142-8. [DOI:10.1111/j.1532-5415.1991.tb01616.x] [PMID]
- Rockwood K, Awalt E, Carver D, MacKnight C. Feasibility and measurement properties of the functional reach and the timed up and go tests in the Canadian study of health and aging. J Gerontol A Biol Sci Med Sci. 2000; 55(2):M70-3. [DOI:10.1093/gerona/55.2.M70] [PMID]
- Christopher A, Kraft E, Olenick H, Kiesling R, Doty A. The reliability and validity of the Timed Up and Go as a clinical tool in individuals with and without disabilities across a lifespan: A systematic review. Disabil Rehabil. 2021; 43(13):1799-813. [DOI:10.1080/09638288.2019.1682066] [PMID]
- Potter JM, Evans AL, Duncan G. Gait speed and activities of daily living function in geriatric patients. Arch Phys Med Rehabil. 1995; 76(11):997-9. [DOI:10.1016/S0003-9993(95)81036-6] [PMID]
- Salbach NM, Mayo NE, Higgins J, Ahmed S, Finch LE, Richards CL. Responsiveness and predictability of gait speed and other disability measures in acute stroke. Arch Phys Med Rehabil. 2001; 82(9):1204-12. [DOI:10.1053/apmr.2001.24907] [PMID]
- Fransen M, Crosbie J, Edmonds J. Reliability of gait measurements in people with osteoarthritis of the knee. Phys Ther. 1997; 77(9):944-53. [DOI:10.1093/ptj/77.9.944] [PMID]
- Evans MD, Goldie PA, Hill KD. Systematic and random error in repeated measurements of temporal and distance parameters of gait after stroke. Arch Phys Med Rehabil. 1997; 78(7):725-9. [DOI:10.1016/S0003-9993(97)90080-0] [PMID]
- Liston RA, Brouwer BJ. Reliability and validity of measures obtained from stroke patients using the Balance Master. Arch Phys Med Rehabil. 1996; 77(5):425-30. [DOI:10.1016/S0003-9993(96)90028-3] [PMID]
- Taylor R. Interpretation of the correlation coefficient: A basic review. J Diagn Med Sonogr. 1990; 6(1):35-9. [DOI:10.1177/875647939000600106]
- Letafatkar A, Hadadnezhad M, Shojaedin S, Mohamadi E. Relationship between functional movement screening score and history of injury. Int J Sports Phys Ther. 2014; 9(1):21-7. [PMID] [PMCID]
- Willems T, Witvrouw E, Verstuyft J, Vaes P, De Clercq D. Proprioception and muscle strength in subjects with a history of ankle sprains and chronic instability. J Athl Train. 2002; 37(4):487-93. [PMID] [PMCID]
- Holland B, Needle AR, Battista RA, West ST, Christiana RW. Physical activity levels among rural adolescents with a history of ankle sprain and chronic ankle instability. PLoS One. 2019; 14(4):e0216243. [DOI:10.1371/journal.pone.0216243] [PMID] [PMCID]
- Vandervoort AA, Chesworth BM, Cunningham DA, Paterson DH, Rechnitzer PA, Koval JJ. Age and sex effects on mobility of the human ankle. J Gerontol. 1992; 47(1):M17-21. [DOI:10.1093/geronj/47.1.M17] [PMID]
- Petrella RJ, Petrella MJ, Cogliano A. Periarticular hyaluronic acid in acute ankle sprain. Clin J Sport Med. 2007; 17(4):251-7. [DOI:10.1097/JSM.0b013e3180f6169f] [PMID]
- Ivins D. Acute ankle sprain: An update. Am Fam Physician. 2006;74(10):1714-20. [Link]
- Gribble PA, Delahunt E, Bleakley C, Caulfield B, Docherty CL, Fourchet F, et al. Selection criteria for patients with chronic ankle instability in controlled research: A position statement of the International Ankle Consortium. J Orthop Sports Phys Ther. 2013; 43(8):585-91. [DOI:10.2519/jospt.2013.0303] [PMID]
- Sitler M, Ryan J, Wheeler B, McBride J, Arciero R, Anderson J, Horodyski M. The efficacy of a semirigid ankle stabilizer to reduce acute ankle injuries in basketball. A randomized clinical study at west point. Am J Sports Med. 1994; 22(4):454-61. [DOI:10.1177/036354659402200404] [PMID]
- Melzack R. Pain and the neuromatrix in the brain. J Dent Educ. 2001; 65(12):1378-82. [DOI:10.1002/j.0022-0337.2001.65.12.tb03497.x] [PMID]
- Melzack R. Pain--An overview. Acta Anaesthesiol Scand. 1999; 43(9):880-4. [DOI:10.1034/j.1399-6576.1999.430903.x] [PMID]
- Riley PO, DellaCroce U, Kerrigan DC. Effect of age on lower extremity joint moment contributions to gait speed. Gait Posture. 2001; 14(3):264-70. [DOI:10.1016/S0966-6362(01)00133-3] [PMID]
- Donovan L, Hetzel S, Laufenberg CR, McGuine TA. Prevalence and impact of chronic ankle instability in adolescent athletes. Orthop J Sports Med. 2020; 8(2):2325967119900962. [DOI:10.1177/2325967119900962] [PMID] [PMCID]
Type of Study: Research |
Subject:
Occupational Therapy
Received: 2023/09/6 | Accepted: 2023/09/27 | Published: 2023/02/20
Received: 2023/09/6 | Accepted: 2023/09/27 | Published: 2023/02/20
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |