Volume 7, Issue 1 (Continuously Updated 2024)
Func Disabil J 2024, 7(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sahoo S, Pradhan R. Efficacy of a Modified Thoracolumbosacral Orthosis in Adult Idiopathic Scoliosis: A Case Study. Func Disabil J 2024; 7 (1) : 265.1
URL: http://fdj.iums.ac.ir/article-1-230-en.html
URL: http://fdj.iums.ac.ir/article-1-230-en.html
1- Department of Prosthetics and Orthotics, Swami Vivekanand National Institute of Rehabilitation Training and Research, Cuttack, India. , swapna.asmile14@gmail.com
2- Department of Prosthetics and Orthotics, Swami Vivekanand National Institute of Rehabilitation Training and Research, Cuttack, India.
2- Department of Prosthetics and Orthotics, Swami Vivekanand National Institute of Rehabilitation Training and Research, Cuttack, India.
Full-Text [PDF 2379 kb]
(202 Downloads)
| Abstract (HTML) (641 Views)
Full-Text: (147 Views)
Introduction
Adult scoliosis is a spinal deformity in a skeletally mature patient with a more than 10-degree curvature of the spine which represents curve progression and spinal degeneration [1, 2]. Aebi has classified adult scoliosis into three groups: Primary degenerative scoliosis, adult idiopathic scoliosis (LIS), and secondary adult curves. The curves in adult LIS can continue to progress during adulthood after skeletal maturity especially for the one whose Cobb angle is bigger than 25 degrees [3]. Its slow and insidious evolution involves structure, function, and physiological alignment of the spine lead to asymmetrical loading which provokes further degenerative change, accelerated curve progression and postural collapse [4, 5]. More than 60 % of cases of adult scoliosis progress, particularly the curves exceeding 30° Cobbs angle at skeletal maturity, regardless of the curve pattern [6, 7]. Depending upon the timing of presentation it can be challenging to differentiate between the various types of adult scoliosis, however most patients will present with back pain accompanied by some form of progressive postural deformity [8]. In the more severe cases, patients may experience lumbar radiculopathy, myelopathy and/ or intermittent neurogenic claudication due to the advanced nature of degenerative changes [9, 10].
Adult scoliosis is a prevalent spinal deformity which can be painful and negatively impacts quality of life (QoL) [11]. It is now well established that untreated scoliosis in the adult can lead to back pain, muscle fatigue and the psychological effects of living with a visible deformity [12]. Different types of treatment are available: Scoliosis specific exercises, various type of spinal orthosis, soft or rigid and surgery. The prevailing treatment is surgery; but scoliosis specific exercises together with other type of physical treatment, such as manipulation program and spinal orthoses, have also been proposed to avoid or stop curve progression along with controlling pain [5, 13, 14]. Bridwell et al. investigated the impact on QoL of surgical and non-surgical treatments on 160 symptomatic adults with lumbar scoliosis and found that surgical treatment of adults with scoliosis resulted in significant improvement in QoL after 2 years, whereas the non-surgical treatments had no significant effect [15]. A recent systematic literature review performed by Alanazi et al. [16] entails the effects of stabilization exercises on back pain, disability and QoL in adults with scoliosis. There is sufficient evidence to support the use of bracing for adolescent LIS [17]. In contrast, there is a scarcity of literature regarding this type of treatment for adult patients. In adults, the thoracolumbosacral (TLSO) or lumbosacral orthoses (LSO) are comparable in appearance and utilize similar materials, however the purpose and proposed mechanism of action is different. Instead of trying to modulate spinal growth, as is the case in adolescent patients, the primary aim of adult bracing is to apply external forces to the spine in improving physiological spinal alignment [18]. While specific braces can improve scoliosis during growth, however, a standard for bracing in adults with scoliosis and pain reduction has not yet been determined. Physical rehabilitation and bracing in adulthood have not yet been investigated in detail. Adult spines are stiffer than adolescent spines and therefore less responsive to external corrective forces, so this type of treatment aims at moving a patient’s spine/trunk into the best possible physiological alignment with the intention of relieving symptoms that accompany postural deviation/collapse along with pain. In this study, a single case is presented; an adult woman with late-onset LIS with chronic pain. The aim of the present study is to evaluate the effectiveness of a modified design thoracolumbosacral orthosis for improving clinical outcomes regarding maintenance of posture, pain reduction and likelihood of curve progression in that patient.
Case Description
A 27-year-old female patient complained of chronic low back pain (LBP) since last 4 years, aggravated by prolonged standing or extensive walking. Sitting and recumbent positions relieved her pain. On radiographic evaluation of thoraco-lumbar spine, she was found with late onset left LIS with apex at T8 level. Earlier she was also using a custom moulded Boston TLSO for one year and then left untreated till date. Then she noticed a gradual change in her posture and severe back pain, so she reported to our institute in December 2017 for spinal rehabilitation and orthotic management. However, the Cobb angle in the thoracic spine continued to progress, leading the orthopedist to suggest surgical intervention, to avoid possible cardiopulmonary compromise in the future. Due to the fear of surgical complications, the patient turned to the conservative treatment of spinal manipulation.
On physical examination, a prominent left posterior rib hump was noted. In the frontal plane, by plumb line assessment she also displayed a postural asymmetry with markedly high left shoulder. A supine leg check revealed evidence of leg length inequality. Given these preliminary findings, along with the positive past history of scoliosis, a plain radiographic study was conducted to locate and calculate the nature and severity of the scoliosis. Initial standing sectional radiographs showed her Cobb angles were 40° thoracic and 33° lumbar, with the curvatures rather balanced and her angles of trunk rotation values (ATR) were 17° thoracic and 3° lumbar as measured with a Scoliometer™. Other than chronic LBP for 4 years no other severe health problems were reported during the investigation. The patient experienced daily pain at an average level of 6–7 on a visual analogue scale (VAS) of 0 (no pain) to 10 (extreme pain). She reported pain episodes, on the level of 8 to 9, once or twice in a month. During a manual trunk recompensation maneuver simulating the brace action, pain was reduced. A modified custom molded thoraco-lumbosacral orthosis and different sessions of physiotherapy for 6 weeks initially were suggested according to the present condition. Goals of treatment included: 1) Improvement of sagittal spine alignment, and 2) Reduction in pain and symptoms. The therapeutic procedure started with brief (less than 15 minutes) sessions of deep tissue massage therapy applied to the postural muscles followed by manipulative intervention, including anterior thoracic manipulation and lumbopelvic adjustments that were delivered bilaterally.
Study tools and outcome measures
The pain intensity was assessed at the low back area and was measured through VAS from 0 to 10, where 0 indicates no pain, and 10 for worst pain. The subjects were asked to make a mark on this line, and then it was measured and recorded in millimeters or centimeters.
Postural symmetry was evaluated by a plumb line method which is critical in measuring coronal balance. It requires a long spine anteroposterior radiograph. A vertical plumb line is dropped vertically from the centre of the C7 vertebral body. This usually intersects with the central sacral vertical line. The horizontal distance between the plumb line and central sacral vertical line is measured. If the plumb line passes within 2 cm of the midline, it defines neutral balance. Positive and negative balance are present when this plumb line passes to the right and left of the midline by >2 cm respectively.
Radiographic progression was the main outcome and it was analyzed as a continuous variable. The Cobb angle is the most commonly used and most accurate measurement of spinal curvature. For this feature to be assessed, it needs initial standing plain anteroposterior radiographs. Angles of ATR were measured by Scoliometer™. To evaluate the effect of treatment, all the parameters were estimated and compared before and after bracing.
Description of orthosis
The modified custom made thoraco-lumbosacral spinal orthosis consists of anterior corset front with adjustable straps attached with posterior TLSO made up of 4 mm polypropylene. The postero-superior trimlines of TLSO follows a line at convex side from 2 inches above the apex of curvature to just below the level of axillary fold along its concavity. The postero-inferior trimline extend up to the apex of gluteal bulge allowing enough sitting clearance. The lateral trimline lies just anterior to the mid axilla and mid trochanteric line on both sides. The posterior TLSO was cut into two shells (upper and lower) at the level of just distal to apex of curvature. The two shells were mechanically hinged at the side of convexity (left side) and a turn buckle mechanism including 10 mm dia 8-length threaded screw with a wing nut and hexagonal bolt were attached at the concave side (right side) adjoining two sections. A turn buckle device is a two threaded eye bolts (righthanded and lefthanded), each screwed into each end of metal frame which adjust the tension by screwing the eye bolts in or out (Figure 1).
Adult scoliosis is a spinal deformity in a skeletally mature patient with a more than 10-degree curvature of the spine which represents curve progression and spinal degeneration [1, 2]. Aebi has classified adult scoliosis into three groups: Primary degenerative scoliosis, adult idiopathic scoliosis (LIS), and secondary adult curves. The curves in adult LIS can continue to progress during adulthood after skeletal maturity especially for the one whose Cobb angle is bigger than 25 degrees [3]. Its slow and insidious evolution involves structure, function, and physiological alignment of the spine lead to asymmetrical loading which provokes further degenerative change, accelerated curve progression and postural collapse [4, 5]. More than 60 % of cases of adult scoliosis progress, particularly the curves exceeding 30° Cobbs angle at skeletal maturity, regardless of the curve pattern [6, 7]. Depending upon the timing of presentation it can be challenging to differentiate between the various types of adult scoliosis, however most patients will present with back pain accompanied by some form of progressive postural deformity [8]. In the more severe cases, patients may experience lumbar radiculopathy, myelopathy and/ or intermittent neurogenic claudication due to the advanced nature of degenerative changes [9, 10].
Adult scoliosis is a prevalent spinal deformity which can be painful and negatively impacts quality of life (QoL) [11]. It is now well established that untreated scoliosis in the adult can lead to back pain, muscle fatigue and the psychological effects of living with a visible deformity [12]. Different types of treatment are available: Scoliosis specific exercises, various type of spinal orthosis, soft or rigid and surgery. The prevailing treatment is surgery; but scoliosis specific exercises together with other type of physical treatment, such as manipulation program and spinal orthoses, have also been proposed to avoid or stop curve progression along with controlling pain [5, 13, 14]. Bridwell et al. investigated the impact on QoL of surgical and non-surgical treatments on 160 symptomatic adults with lumbar scoliosis and found that surgical treatment of adults with scoliosis resulted in significant improvement in QoL after 2 years, whereas the non-surgical treatments had no significant effect [15]. A recent systematic literature review performed by Alanazi et al. [16] entails the effects of stabilization exercises on back pain, disability and QoL in adults with scoliosis. There is sufficient evidence to support the use of bracing for adolescent LIS [17]. In contrast, there is a scarcity of literature regarding this type of treatment for adult patients. In adults, the thoracolumbosacral (TLSO) or lumbosacral orthoses (LSO) are comparable in appearance and utilize similar materials, however the purpose and proposed mechanism of action is different. Instead of trying to modulate spinal growth, as is the case in adolescent patients, the primary aim of adult bracing is to apply external forces to the spine in improving physiological spinal alignment [18]. While specific braces can improve scoliosis during growth, however, a standard for bracing in adults with scoliosis and pain reduction has not yet been determined. Physical rehabilitation and bracing in adulthood have not yet been investigated in detail. Adult spines are stiffer than adolescent spines and therefore less responsive to external corrective forces, so this type of treatment aims at moving a patient’s spine/trunk into the best possible physiological alignment with the intention of relieving symptoms that accompany postural deviation/collapse along with pain. In this study, a single case is presented; an adult woman with late-onset LIS with chronic pain. The aim of the present study is to evaluate the effectiveness of a modified design thoracolumbosacral orthosis for improving clinical outcomes regarding maintenance of posture, pain reduction and likelihood of curve progression in that patient.
Case Description
A 27-year-old female patient complained of chronic low back pain (LBP) since last 4 years, aggravated by prolonged standing or extensive walking. Sitting and recumbent positions relieved her pain. On radiographic evaluation of thoraco-lumbar spine, she was found with late onset left LIS with apex at T8 level. Earlier she was also using a custom moulded Boston TLSO for one year and then left untreated till date. Then she noticed a gradual change in her posture and severe back pain, so she reported to our institute in December 2017 for spinal rehabilitation and orthotic management. However, the Cobb angle in the thoracic spine continued to progress, leading the orthopedist to suggest surgical intervention, to avoid possible cardiopulmonary compromise in the future. Due to the fear of surgical complications, the patient turned to the conservative treatment of spinal manipulation.
On physical examination, a prominent left posterior rib hump was noted. In the frontal plane, by plumb line assessment she also displayed a postural asymmetry with markedly high left shoulder. A supine leg check revealed evidence of leg length inequality. Given these preliminary findings, along with the positive past history of scoliosis, a plain radiographic study was conducted to locate and calculate the nature and severity of the scoliosis. Initial standing sectional radiographs showed her Cobb angles were 40° thoracic and 33° lumbar, with the curvatures rather balanced and her angles of trunk rotation values (ATR) were 17° thoracic and 3° lumbar as measured with a Scoliometer™. Other than chronic LBP for 4 years no other severe health problems were reported during the investigation. The patient experienced daily pain at an average level of 6–7 on a visual analogue scale (VAS) of 0 (no pain) to 10 (extreme pain). She reported pain episodes, on the level of 8 to 9, once or twice in a month. During a manual trunk recompensation maneuver simulating the brace action, pain was reduced. A modified custom molded thoraco-lumbosacral orthosis and different sessions of physiotherapy for 6 weeks initially were suggested according to the present condition. Goals of treatment included: 1) Improvement of sagittal spine alignment, and 2) Reduction in pain and symptoms. The therapeutic procedure started with brief (less than 15 minutes) sessions of deep tissue massage therapy applied to the postural muscles followed by manipulative intervention, including anterior thoracic manipulation and lumbopelvic adjustments that were delivered bilaterally.
Study tools and outcome measures
The pain intensity was assessed at the low back area and was measured through VAS from 0 to 10, where 0 indicates no pain, and 10 for worst pain. The subjects were asked to make a mark on this line, and then it was measured and recorded in millimeters or centimeters.
Postural symmetry was evaluated by a plumb line method which is critical in measuring coronal balance. It requires a long spine anteroposterior radiograph. A vertical plumb line is dropped vertically from the centre of the C7 vertebral body. This usually intersects with the central sacral vertical line. The horizontal distance between the plumb line and central sacral vertical line is measured. If the plumb line passes within 2 cm of the midline, it defines neutral balance. Positive and negative balance are present when this plumb line passes to the right and left of the midline by >2 cm respectively.
Radiographic progression was the main outcome and it was analyzed as a continuous variable. The Cobb angle is the most commonly used and most accurate measurement of spinal curvature. For this feature to be assessed, it needs initial standing plain anteroposterior radiographs. Angles of ATR were measured by Scoliometer™. To evaluate the effect of treatment, all the parameters were estimated and compared before and after bracing.
Description of orthosis
The modified custom made thoraco-lumbosacral spinal orthosis consists of anterior corset front with adjustable straps attached with posterior TLSO made up of 4 mm polypropylene. The postero-superior trimlines of TLSO follows a line at convex side from 2 inches above the apex of curvature to just below the level of axillary fold along its concavity. The postero-inferior trimline extend up to the apex of gluteal bulge allowing enough sitting clearance. The lateral trimline lies just anterior to the mid axilla and mid trochanteric line on both sides. The posterior TLSO was cut into two shells (upper and lower) at the level of just distal to apex of curvature. The two shells were mechanically hinged at the side of convexity (left side) and a turn buckle mechanism including 10 mm dia 8-length threaded screw with a wing nut and hexagonal bolt were attached at the concave side (right side) adjoining two sections. A turn buckle device is a two threaded eye bolts (righthanded and lefthanded), each screwed into each end of metal frame which adjust the tension by screwing the eye bolts in or out (Figure 1).
Lower and upper ends of turn buckle were fixed with the lower and upper section respectively to stabilize the pelvis and to maintain the proper position of turn buckle. Necessary adjustments of tension were facilitated by arrangement of wing nut and hexagonal bolt. Tightening of turn buckle stretched the concave side of curve, thus correcting the deformity. The adjusted tension was maintained by an aluminum spacer in a specified position.
Design concept
The modified custom made TLSO maintain the spinal alignment by deloading the affected spine and transferring weight from affected to non-affected area of the spine, thereby reducing pain by less effort from the paraspinal muscles (Figure 2).
Design concept
The modified custom made TLSO maintain the spinal alignment by deloading the affected spine and transferring weight from affected to non-affected area of the spine, thereby reducing pain by less effort from the paraspinal muscles (Figure 2).
The combination of axial and transverse loading is best utilized in the current spinal orthosis for scoliotic deformity correction. The axial force applied at two ends of spinal curvature is used to elongate and straighten the spine. The mechanism of angular correction by elongation is not due to tensile stress exerted in the spine but rather due to bending moment applied at various intervertebral disc spaces.
Bending moment = F X D where F = applied force and D = distance
The intervertebral disc bending moment applied at the apex of curvature increases with the increment in distance from the central axis to apex of deformity, thereby angular deformity is corrected. Transverse loading is also exerted by the spinal orthosis by the principle of reciprocal parallel forces or 3-point force system. In the scoliotic spine, one corrective force is applied at the apex of deformity and parallel forces from the opposite side of the apex of curvature which provide support and stabilization to the spine.
Bending moment at the apex of curvature = FXL
where, F = applied force and L = length
The turn buckle device along with mechanical hinge applies a static low load progressive gentle stretching force to the scoliotic spine which prevents further curve progression and maintain erect upright posture. Gradually opening the hinge on the concave side of the deformity would apply lateral and vertical forces, thereby slowly correcting the deformity. The basic principle of this method applied the idea that bending forces are required in conjunction with traction to straighten any curve. Tightening the screw causes the length to be increased between the two segments of orthosis results in more traction forces to correct the deformity in addition to the axial load.
Results
After 1 year of continuous use of spinal orthosis along with physiotherapy, the patient was re-evaluated using static spinal radiography, VAS score and plumb line method. Table 1 illustrates comparison of measured between pre-treatment and post treatment conditions after 1 year.
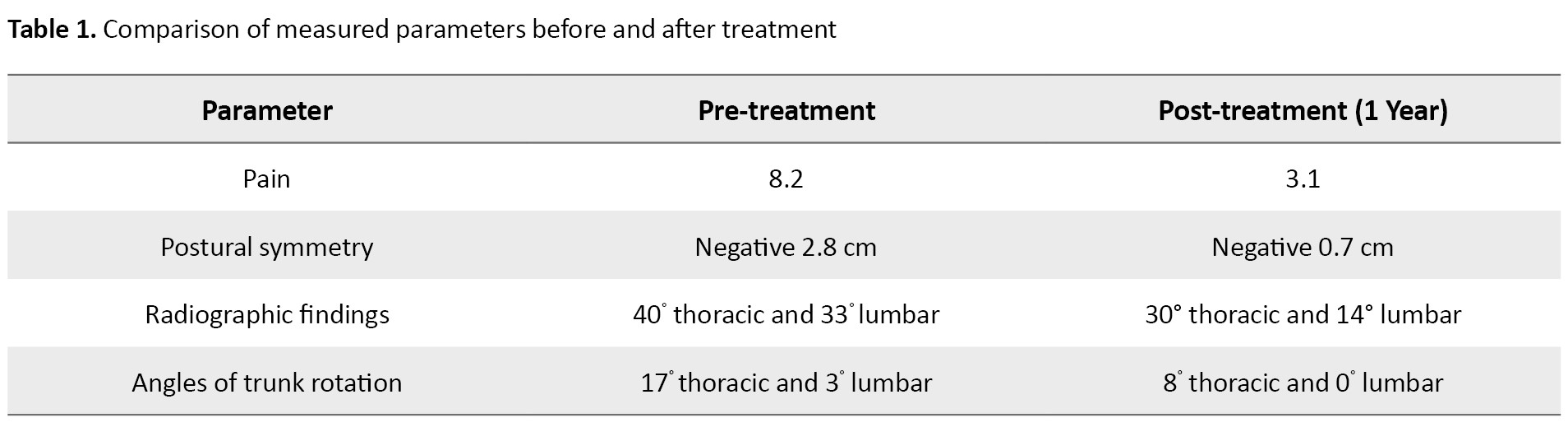
The plumb line was used as a tool to assess the symmetry in posture. According to patient statement, the combination of orthosis and exercises resulted in a dramatic improvement in her QoL. The comparison of the postural symmetry with and without orthosis showed that there was a maximum correction in erect upright posture with the even immediately after wearing the orthosis. It has been found to be quite effective in maintaining erect upright posture, thus increases the long-standing ability. In addition, she reported a decrease in her LBP from approximately VAS 8 to VAS 3 and post intervention radiographs showed an improvement in left thoracic scoliosis and coronal balance.
Discussion
Coordinated manual therapies and custom moulded spinal orthoses have been increasingly investigated in recent years for scoliosis treatment. Spinal manipulation, bracing, and rehabilitative procedures seem to alter spinal structure when applied in combination. The incidence of progression of adult scoliosis with a Cobb angle greater than 30° is 30%. However, patients with curves between 40° and 50° were preferably treated with surgical intervention [19]. In this case, curve progression stopped and reduced to 30° after 1 year treatment of combined bracing and exercises.
The spinal curvature with Cobb angle greater than 40° may be managed with bracing or surgical intervention. If bracing is continued for long term without any noticeable change, surgery will be suggested in patients with Cobb angles of greater than 40°. This study suggests the effectiveness of custom-molded modified TLSO in slowing down the progression of adult scoliosis. Considering its limited side effects, it represents an interesting treatment option and an alternative to surgery that is associated with a high rate of complications and technical difficulties related to the marginal bone quality in this population [20]. Reducing scoliotic curvatures through conservative treatment methods to avoid surgery is worthy of consideration, and combination of therapy and modified TLSO provide an additional option for treatment of adult scoliosis especially in the present scenario.
Bracing for adult scoliosis is believed to outperform observation or other nonsurgical therapies. However, some studies and reviews showed that bracing neither correct curvature of the spine nor reduce the need for surgery [21]. In the current scenario, modified design of spinal orthosis improved patient’s scoliosis markedly with reduction of pain. The over corrective force induced by earlier design TLSO (Boston) was intolerable to bear, thereby it represents a negative compliance rate of the orthosis. The new design provides a progressive correction at regular intervals till the postural symmetry is achieved. So, it indicates a positive acceptance of the patient towards the spinal orthosis.
The goal to reduce pain and to achieve normal postural alignment is achieved in this case. The findings of the review would suggest that bracing may be effective, in the short- to medium-term, for reducing pain and improving function in some adult patients. The proposed mechanism of action in this design improved physiological spinal alignment and coronal and sagittal balance which corresponds with Dubousset’s ‘cone of economy’ theory [22]. Interestingly, while improvements in Cobb angle, rib hump and sagittal/coronal balance were noted in this female patient, these changes were not uniform within or across the earlier studies because of these heterogenous outcomes among the participants [23]. It is important to note that degenerative change and normal ageing contribute to decreased flexibility and increased stiffness in the adult spine. Thus, it is plausible that the spine of an adult with scoliosis may be significantly more resistant to the influence of external corrective forces such as those being exerted by a spinal brace/orthosis. This scenario makes the goal of restoring normal spinal alignment using an orthosis more challenging in adult populations [24, 25]. The positive results observed in this case patients may therefore be the result of very small shifts created by the brace in the x, y and z axes are enough to alter symptomatology and the clinical course of spinal deformity supported by Khan et al. [26].
Hours of brace-wear may also be an important factor in adults with scoliosis. The number of hours of brace-wear reported amongst participants in the studies ranged from 2 to 23 h per day. In adolescent populations at least, that bracing outcomes are strongly influenced by compliance to brace-wear prescriptions [27]. Weiss et al. stated that spinal braces/orthoses place the patient’s trunk in a fixed position which can impair movement and restrict certain postures. So, brace wear prescriptions in earlier studies were left up to patient preference and were not successful [28]. This prompted to modify our study protocol regarding the brace-wear prescription to a minimum of 12-16 h per day for the first six months. After that point, mobilization of the spine would be allowed for the desired functional improvements in the spine.
Conclusion
The combination of orthotic and therapeutic treatment was associated with a recovery in the spinal curvature and coronal imbalance of the spine as well as backache. This suggests that modified design custom moulded TLSO is effective in the management of adult LIS. Considering its limited side effects, still it provides regular adjustments in operative time approaches and bracing should be proposed as first line treatment adjunct to physiotherapy. Moreover, it represents an acceptable alternative to surgery for patients who refused for surgery. Future long term and larger studies are essential to determine the sustainability of the early positive results.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Department of Prosthetics and Orthotics, Utkal University, Bhubaneswar, India.
Funding
The paper was extracted from a research project at the Department of Prosthetics and Orthotics, Utkal University, Bhubaneswar, India.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the patient for her timely cooperation and sincere participation in this study.
References
Bending moment = F X D where F = applied force and D = distance
The intervertebral disc bending moment applied at the apex of curvature increases with the increment in distance from the central axis to apex of deformity, thereby angular deformity is corrected. Transverse loading is also exerted by the spinal orthosis by the principle of reciprocal parallel forces or 3-point force system. In the scoliotic spine, one corrective force is applied at the apex of deformity and parallel forces from the opposite side of the apex of curvature which provide support and stabilization to the spine.
Bending moment at the apex of curvature = FXL
where, F = applied force and L = length
The turn buckle device along with mechanical hinge applies a static low load progressive gentle stretching force to the scoliotic spine which prevents further curve progression and maintain erect upright posture. Gradually opening the hinge on the concave side of the deformity would apply lateral and vertical forces, thereby slowly correcting the deformity. The basic principle of this method applied the idea that bending forces are required in conjunction with traction to straighten any curve. Tightening the screw causes the length to be increased between the two segments of orthosis results in more traction forces to correct the deformity in addition to the axial load.
Results
After 1 year of continuous use of spinal orthosis along with physiotherapy, the patient was re-evaluated using static spinal radiography, VAS score and plumb line method. Table 1 illustrates comparison of measured between pre-treatment and post treatment conditions after 1 year.
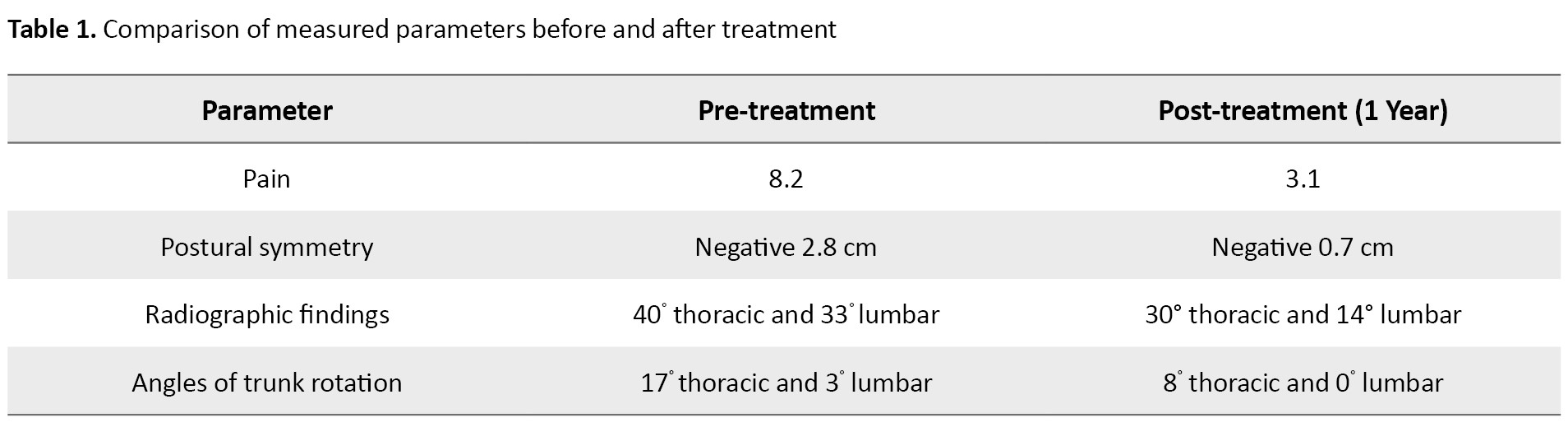
The plumb line was used as a tool to assess the symmetry in posture. According to patient statement, the combination of orthosis and exercises resulted in a dramatic improvement in her QoL. The comparison of the postural symmetry with and without orthosis showed that there was a maximum correction in erect upright posture with the even immediately after wearing the orthosis. It has been found to be quite effective in maintaining erect upright posture, thus increases the long-standing ability. In addition, she reported a decrease in her LBP from approximately VAS 8 to VAS 3 and post intervention radiographs showed an improvement in left thoracic scoliosis and coronal balance.
Discussion
Coordinated manual therapies and custom moulded spinal orthoses have been increasingly investigated in recent years for scoliosis treatment. Spinal manipulation, bracing, and rehabilitative procedures seem to alter spinal structure when applied in combination. The incidence of progression of adult scoliosis with a Cobb angle greater than 30° is 30%. However, patients with curves between 40° and 50° were preferably treated with surgical intervention [19]. In this case, curve progression stopped and reduced to 30° after 1 year treatment of combined bracing and exercises.
The spinal curvature with Cobb angle greater than 40° may be managed with bracing or surgical intervention. If bracing is continued for long term without any noticeable change, surgery will be suggested in patients with Cobb angles of greater than 40°. This study suggests the effectiveness of custom-molded modified TLSO in slowing down the progression of adult scoliosis. Considering its limited side effects, it represents an interesting treatment option and an alternative to surgery that is associated with a high rate of complications and technical difficulties related to the marginal bone quality in this population [20]. Reducing scoliotic curvatures through conservative treatment methods to avoid surgery is worthy of consideration, and combination of therapy and modified TLSO provide an additional option for treatment of adult scoliosis especially in the present scenario.
Bracing for adult scoliosis is believed to outperform observation or other nonsurgical therapies. However, some studies and reviews showed that bracing neither correct curvature of the spine nor reduce the need for surgery [21]. In the current scenario, modified design of spinal orthosis improved patient’s scoliosis markedly with reduction of pain. The over corrective force induced by earlier design TLSO (Boston) was intolerable to bear, thereby it represents a negative compliance rate of the orthosis. The new design provides a progressive correction at regular intervals till the postural symmetry is achieved. So, it indicates a positive acceptance of the patient towards the spinal orthosis.
The goal to reduce pain and to achieve normal postural alignment is achieved in this case. The findings of the review would suggest that bracing may be effective, in the short- to medium-term, for reducing pain and improving function in some adult patients. The proposed mechanism of action in this design improved physiological spinal alignment and coronal and sagittal balance which corresponds with Dubousset’s ‘cone of economy’ theory [22]. Interestingly, while improvements in Cobb angle, rib hump and sagittal/coronal balance were noted in this female patient, these changes were not uniform within or across the earlier studies because of these heterogenous outcomes among the participants [23]. It is important to note that degenerative change and normal ageing contribute to decreased flexibility and increased stiffness in the adult spine. Thus, it is plausible that the spine of an adult with scoliosis may be significantly more resistant to the influence of external corrective forces such as those being exerted by a spinal brace/orthosis. This scenario makes the goal of restoring normal spinal alignment using an orthosis more challenging in adult populations [24, 25]. The positive results observed in this case patients may therefore be the result of very small shifts created by the brace in the x, y and z axes are enough to alter symptomatology and the clinical course of spinal deformity supported by Khan et al. [26].
Hours of brace-wear may also be an important factor in adults with scoliosis. The number of hours of brace-wear reported amongst participants in the studies ranged from 2 to 23 h per day. In adolescent populations at least, that bracing outcomes are strongly influenced by compliance to brace-wear prescriptions [27]. Weiss et al. stated that spinal braces/orthoses place the patient’s trunk in a fixed position which can impair movement and restrict certain postures. So, brace wear prescriptions in earlier studies were left up to patient preference and were not successful [28]. This prompted to modify our study protocol regarding the brace-wear prescription to a minimum of 12-16 h per day for the first six months. After that point, mobilization of the spine would be allowed for the desired functional improvements in the spine.
Conclusion
The combination of orthotic and therapeutic treatment was associated with a recovery in the spinal curvature and coronal imbalance of the spine as well as backache. This suggests that modified design custom moulded TLSO is effective in the management of adult LIS. Considering its limited side effects, still it provides regular adjustments in operative time approaches and bracing should be proposed as first line treatment adjunct to physiotherapy. Moreover, it represents an acceptable alternative to surgery for patients who refused for surgery. Future long term and larger studies are essential to determine the sustainability of the early positive results.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Department of Prosthetics and Orthotics, Utkal University, Bhubaneswar, India.
Funding
The paper was extracted from a research project at the Department of Prosthetics and Orthotics, Utkal University, Bhubaneswar, India.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the patient for her timely cooperation and sincere participation in this study.
References
- Jo JY. Adult idiopathic scoliosis treated by acupuncture: A case report. J Churna Man Med Spine and Nerves. 2012;7(1):21-5. [Link]
- Aebi M. The adult scoliosis. Eur Spine J. 2005; 14(10):925-48. [DOI:10.1007/s00586-005-1053-9] [PMID]
- Zhang H, Gao Q, Wang Y, Liu S, Guo C, Tang M, et al. Clinical evaluation of indirect decompression treatments for degenerative adult idiopathic scoliosis. Arch Orthop Trauma Surg. 2011; 131(12):1639-47. [DOI:10.1007/s00402-011-1377-3] [PMID]
- Guigui P, Rillardon L. [Adult spinal deformities (French)]. Rev Prat. 2006;56(7):701-8. [PMID]
- Negrini A, Negrini MG, Donzelli S, Romano M, Zaina F, Negrini S. Scoliosis-Specific exercises can reduce the progression of severe curves in adult idiopathic scoliosis: A long-term cohort study. Scoliosis. 2015;10:20. [DOI:10.1186/s13013-015-0044-9] [PMID]
- Weinstein SL, Dolan LA, Spratt KF, Peterson KK, Spoonamore MJ, Ponseti IV. Health and function of patients with untreated idiopathic scoliosis: A 50-year natural history study. JAMA. 2003; 289(5):559-67. [DOI:10.1001/jama.289.5.559] [PMID]
- Weinstein SL. Natural history. Spine. 1999; 24(24):2592-600. [DOI:10.1097/00007632-199912150-00006] [PMID]
- Wong E, Altaf F, Oh LJ, Gray RJ. Adult degenerative lumbar scoliosis. Orthopedics. 2017; 40(6):e930-9. [DOI:10.3928/01477447-20170606-02] [PMID]
- Weiss HR, Dallmayer R. Brace treatment of spinal claudication in an adult with lumbar scoliosis-a case report. Stud Health Technol Inform. 2006; 123:586-9. [PMID]
- Buchowski JM. Adult scoliosis: Etiology and classification. Sem Spine Surg. 2009; 21(1):2-6 [DOI:10.1053/j.semss.2008.12.001]
- Palazzo C, Montigny JP, Barbot F, Bussel B, Vaugier I, Fort D, et al. Effects of bracing in adult with scoliosis: A retrospective study. Arch Phys Med Rehabil. 2017; 98(1):187-90. [DOI:10.1016/j.apmr.2016.05.019] [PMID]
- Bradford DS, Tay BK, Hu SS. Adult Scoliosis: Surgical indications, operative management, complications, and outcomes. Spine. 1999; 24(24):2617-29. [DOI:10.1097/00007632-199912150-00009] [PMID]
- Tarola GA. Manipulation for the control of back pain and curve progression in patients with skeletally mature idiopathic scoliosis: Two cases. J Manipulative Physiol Ther. 1994; 17(4):253-7. [PMID]
- Brooks WJ, Krupinski EA, Hawes MC. Reversal of childhood idiopathic scoliosis in an adult, without surgery: A case report and literature review. Scoliosis. 2009; 4:27. [DOI:10.1186/1748-7161-4-27] [PMID]
- Bridwell KH, Glassman S, Horton W, Shaffrey C, Schwab F, Zebala LP, et al. Does treatment (nonoperative and operative) improve the twoyear quality of life in patients with adult symptomatic lumbar scoliosis: A prospective multicenter evidence-based medicine study. Spine. 2009; 34(20):2171-8. [DOI:10.1097/BRS.0b013e3181a8fdc8] [PMID]
- Alanazi MH, Parent EC, Dennett E. Effect of stabilization exercise on back pain, disability and quality of life in adults with scoliosis: A systematic review. Eur J Phys Rehabil Med. 2018; 54(5):647-53. [DOI:10.23736/S1973-9087.17.05062-6] [PMID]
- Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med. 2013; 369(16):1512-21. [DOI:10.1056/NEJMoa1307337] [PMID]
- McAviney J, Mee J, Fazalbhoy A, Du Plessis J, Brown BT. A systematic literature review of spinal brace/orthosis treatment for adults with scoliosis between 1967 and 2018: Clinical outcomes and harms data. BMC Musculoskelet Disord. 2020;21(1):87.[DOI:10.1186/s12891-020-3095-x] [PMID]
- Chen KC, Chiu EH. Adolescent idiopathic scoliosis treated by spinal manipulation: A case study. J Altern Complement Med. 2008; 14(6):749-51. [DOI:10.1089/acm.2008.0054] [PMID]
- Lonstein JE. Scoliosis: Surgical versus nonsurgical treatment. Clin Orthop Relat Res. 2006; 443:248-59. [DOI:10.1097/01.blo.0000198725.54891.73] [PMID]
- Dickson RA, Weinstein SL. Bracing (and screening)-yes, or no? Bone Joint J. 1999; 81(2):193-8. [DOI:10.1302/0301-620X.81B2.0810193]
- Dubousset J. Three-dimensional analysis of the scoliotic deformity. In: Weinstein SL, editor. Pediatric spine principles and practice. New York: Raven Press; 1994. [Link]
- Diebo BG, Henry J, Lafage V, Berjano P. Sagittal deformities of the spine: Factors influencing the outcomes and complications. Eur Spine J. 2015; 24 (Suppl 1):S3-15. [DOI:10.1007/s00586-014-3653-8] [PMID]
- Galbusera F, Van Rijsbergen M, Ito K, Huyghe JM, Brayda-Bruno M, Wilke HJ. Ageing and degenerative changes of the intervertebral disc and their impact on spinal flexibility. Eur Spine J. 2014; 23:S324-32. [DOI:10.1007/s00586-014-3203-4]
- Daniels AH, Smith JS, Hiratzka J, Ames CP, Bess S, Shaffrey CI, et al. Functional limitations due to lumbar stiffness in adults with and without spinal deformity. Spine. 2015; 40(20):1599-604. [DOI:10.1097/BRS.0000000000001090] [PMID]
- Khan MJ, Srinivasan VM, Jea AH. The history of bracing for scoliosis. Clin Pediatr (Phila). 2016; 55(4):320-5. [DOI:10.1177/0009922815615829] [PMID]
- Katz DE, Herring JA, Browne RH, Kelly DM, Birch JG. Brace wear control of curve progression in adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2010; 92(6):1343-52. [DOI:10.2106/JBJS.I.01142] [PMID]
- Weiss HR, Dallmayer R, Stephan C. First results of pain treatment in scoliosis patients using a sagittal realignment brace. Stud Health Technol Inform. 2006; 123:582-5. [PMID]
Type of Study: Case Study |
Subject:
Prosthetics and Orthotics
Received: 2023/08/24 | Accepted: 2023/11/5 | Published: 2024/08/6
Received: 2023/08/24 | Accepted: 2023/11/5 | Published: 2024/08/6