Volume 6, Issue 1 (Continuously Updated 2023)
Func Disabil J 2023, 6(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Jiryaei Z. Designing, Manufacturing, and Checking the Accuracy of an Audio Biofeedback Device for Controlling the Angle of the Wrist in Stroke People: A Pilot Study. Func Disabil J 2023; 6 (1) : 226.1
URL: http://fdj.iums.ac.ir/article-1-228-en.html
URL: http://fdj.iums.ac.ir/article-1-228-en.html
Student Research Committee, School of Rehabilitation, Iran University of Medical Science, Tehran, Iran. , Jiryaei.Z@gmail.com
Full-Text [PDF 1422 kb]
(420 Downloads)
| Abstract (HTML) (1470 Views)
Full-Text: (596 Views)
Introduction
Stroke may lead to disabilities in daily activities [1]. Loss of function, especially in hand, leads to severe physical and mental disabilities that affect daily activities, including working conditions and quality of life [2]. The prevalence of stroke in developed countries is about 100-300 cases per 100 000 people per year [3]. Studies have shown that stroke is the third cause of disability [4]. A total of 45% of elderly people with stroke are severely unable to perform daily functions.
Adherence to exercise programs is usually a challenge for therapists. Its effectiveness of some factors, including the exercise protocol and patient participation [5]. Despite the effect of exercise and exercise therapy on physical and social health for the elderly with disabilities, participating in exercise and exercise therapy is still weak among them [6, 7]. Campbell et al. showed that non-compliance with physiotherapy is common. From the patient’s perspective, the decision to comply or not to comply is rational but often unpredictable by therapists or researchers [8]. Less participation in exercise and therapeutic exercise may correlate to general factors, such as fear of adverse consequences and lack of motivation [6, 7].
Using supervised exercise sessions, referring patients for regular consultation with a physician, or attending group exercise classes may help ensure long-term exercise compliance and improve therapeutic outcomes [4]. Referring patients to clinics or group sessions to do therapeutic exercises is costly and time-consuming and is not always available for elderly patients [9, 10]. Regarding the importance of health protocols in the COVID-19 epidemic, especially for the elderly, a method is required to do therapeutic exercises at home without attending medical centers [9].
Due to physical and cognitive disorders, it is often difficult and costly for people who have suffered a stroke to access on-site rehabilitation. Telerehabilitation offers the opportunity to promote the rehabilitation process [11]. According to other recent studies, telerehabilitation shows a positive impact on patients’ compliance and adherence [12, 13] because the patients’ opinions are crucial [14]. This trial contributes to the scientific-based knowledge regarding the effects of telerehabilitation and the increase in participation. Complicating and challenging exercises lead to non-adherence to treatment [15].
In addition, based on the International Organization for Standardization, the usability of using the product to achieve particular goals, effectiveness, efficiency, and user satisfaction are considered in a certain scope [16]. In the current study, one of the most critical steps was “usability” testing to collect empirical data from users and learn the usage, efficiency, tool durability, and safety [17], useful for identifying problems with existing tools. According to Nielsen, usability testing of five users should identify up to 80% of potential problems with a particular tool [18, 19]. Williams stated that the level of patients’ satisfaction can show its quality, i.e. the higher quality, the higher patient satisfaction [20].
The present study was conducted to develop a tool based on audio biofeedback and increase the rate of participation in therapeutic exercise, i.e. people with stroke do their therapeutic exercises with high attractiveness under the practices and standards considered by the therapist at home.
Materials and Methods
Audio biofeedback (Figure 1) is an invention (registration No A61B 5/00) (Attachment). The device included an audio biofeedback box (including battery, sound alarm, on and off switch, and two LED lamps), connecting wire (including two connecting cables, two connecting wires, and two rotating plates to adjust the joint angle, each consisting of a mercury lamp), joint strap (one strap with velcro, one magnet to connect to the rotating plates of the lamp). Two small lamps were placed on both sides of the sound alarm and turned on and off when the alarm turned on and off; therefore they were as visual biofeedback.
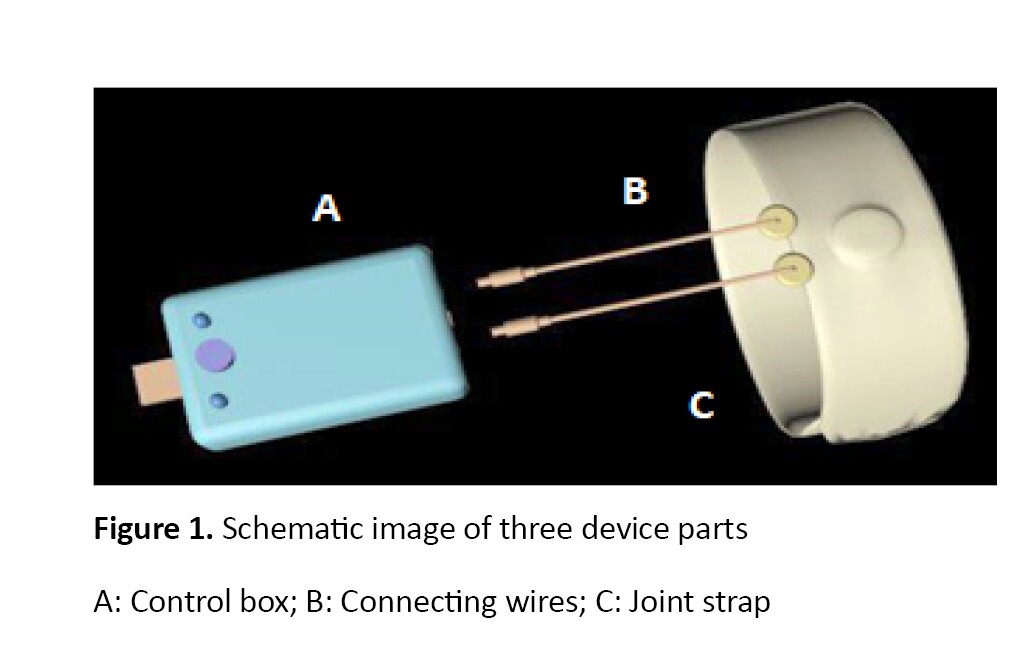
Figure 2 shows the biofeedback box. The two rotating plates were used to adjust the angles. After the wrist reached the desired angle, the alarm was turned on and sounded.

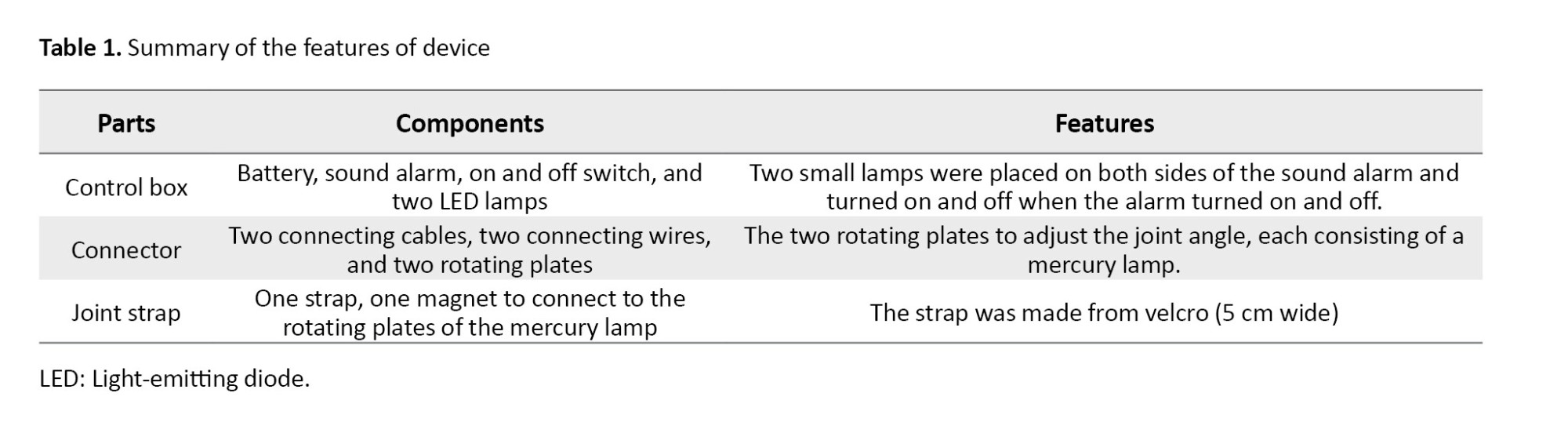
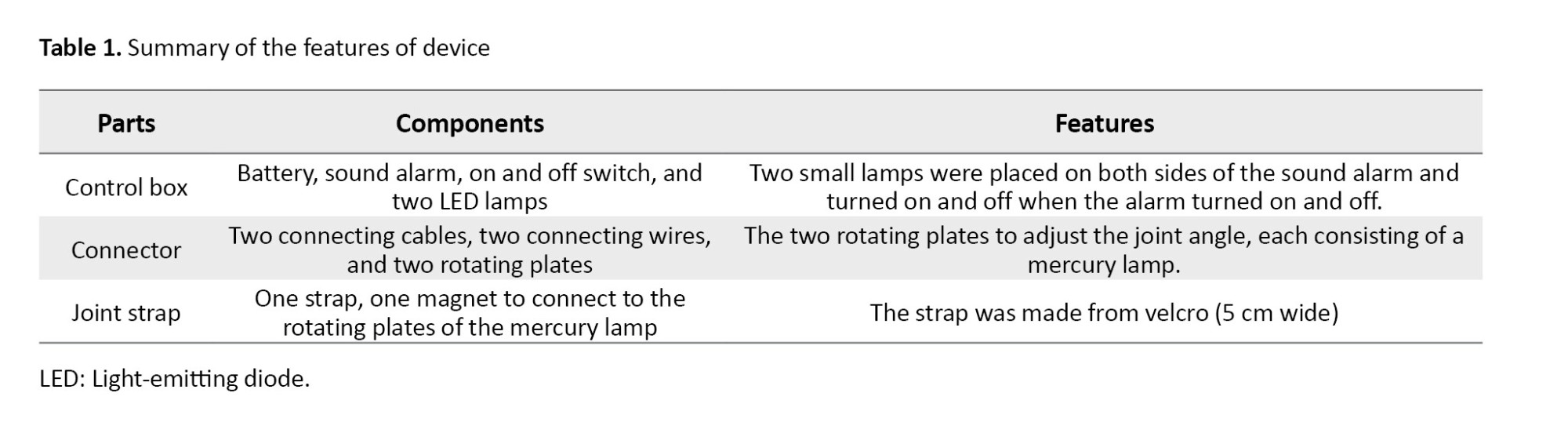
Table 1 presents the summary of the device features.
Study design and participants
This pilot study was conducted at Iran University of Medical Sciences. A total of 28 healthy students were included from Iran University of Medical Sciences. The participants were selected based on convenience and non-probability sampling method and the inclusion criteriaincluded aged 18 to 25 years, no pain in upper limbs, no spasticity in upper limbs, no disability in upper limbs, and a full range of motion (ROM) of the wrist. The exclusion criteria included unwillingness to continue the test. Table 2 presents the subjects’ age, weight, height, and size of wrist before the study. A sample size was estimated by G-power software and according to a power of 95%, and a one-sided significance level of 0.05. A sample size of 28 healthy people was needed [21].

Data collection
For all participants, the following outcome measurements were evaluated, demographic data, wrist size, responsiveness in ROM of the wrist, time of device responsiveness, and participants’ satisfaction. Primary outcome measures were the device feasibility in wrist ROM and device feasibility time; the secondary outcome measure was participants’ satisfaction with the device process (please see attachments) [19, 22].
At first, the evaluator asked each participant to sit on a chair. Second, the evaluator tied the strap to his wrist. Third, the evaluator rotated the two small rotating plates to the desired amount in the counterclockwise direction and then asked each volunteer to move the wrist in the extension and the flexion. When the tool warned, i.e. the movement was done in the correct direction.
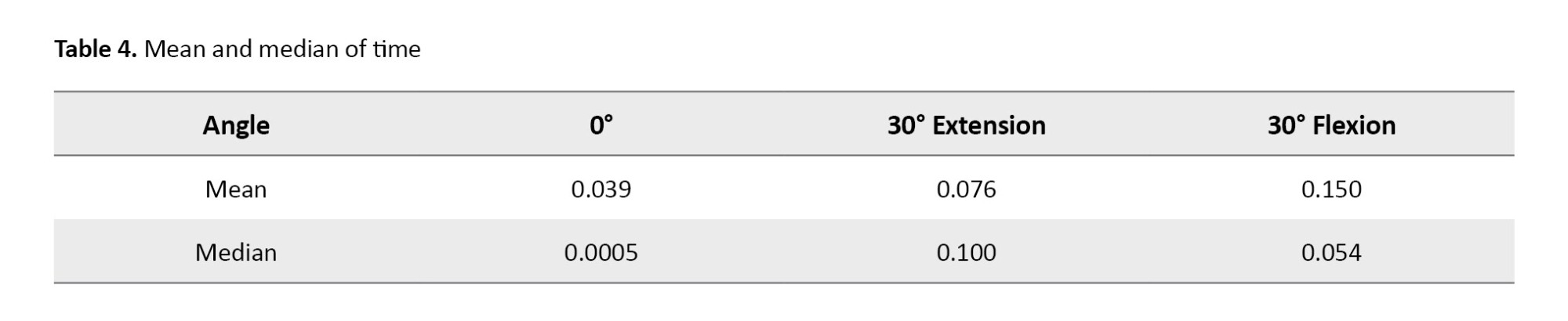
The researcher considered three angles 0°, 30° extension, and 30° flexion. The evaluator set the device at each angle and asked participants to move their wrists at certain angles and keep those till the tool was warned. When the device was warned, the evaluator measured the participants’ wrist angle. The evaluator measured the time between the time the wrist reached certain angles, and when the device warned as the time of device responsiveness. To decrease errors, the evaluator repeated all of the tests three times. In the end, the evaluator asked participants to fill up the satisfaction questionnaire on five-point Likert scale [19, 22].
Results
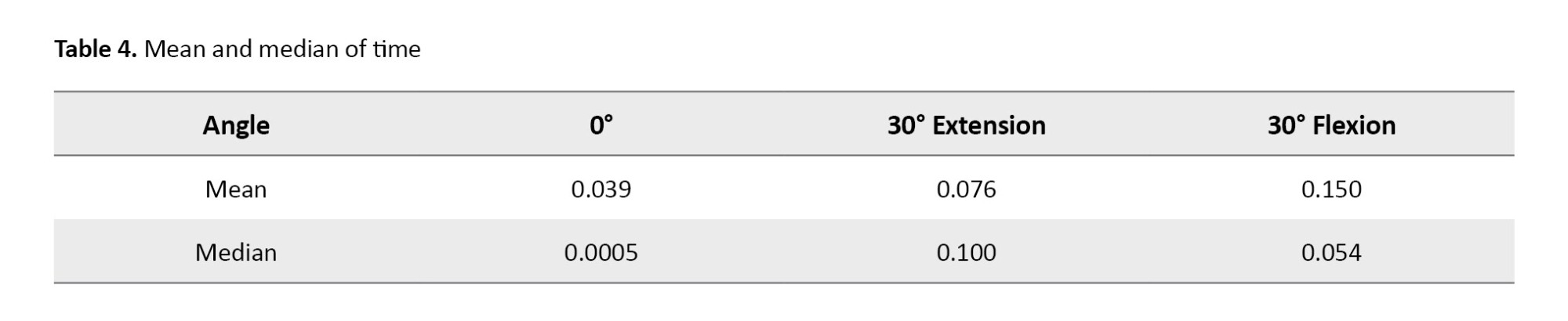
The results showed that the device was efficient for all participants in 0°. Two participants did not show the correct angle in the 30°flexion by the device. Also, two participants did not show the 30° extension correctly by the device. Tables 3 and 4 present the result of device feasibility and responsibility of time. The results of the Fridman test showed no significant difference between the three-time trials (P=0.110) for each angle. Figure 1 shows the average score for each item of the satisfaction questionnaire. A score above the optimal threshold (2.5) was considered for each question.

Discussion
Telerehabilitation has attracted more attention from society (the research community and the commercial market) [23]. The results showed that the audio biofeedback device is efficient in the evaluated angles. Also, the device gave feedback in less than 15 hundredths of a second. The results of this study are beneficial for rehabilitation centers and clinics.
Based on the results of the satisfaction questionnaire, all participants were assigned a score higher than the optimal threshold for every question. The highest score was 5 (the easy learning of the tool), it means the device has a simple process for its users. Therefore, many users who cannot understand complex devices easily perform exercises with the studied device. Since exercise with the device designed in this study does not require any clinical travel and high costs, it has better follow-up of patients with stroke and other disabilities in the wrist in doing therapeutic exercises and saving time with better availability.
Nowadays, due to outbreaks of pandemic diseases, telerehabilitation has attracted the attention of many disabled people, therapists, and researchers [11]. In this article, the researcher tried to aid the telerehabilitation process by introducing a biofeedback tool. In a similar study, the effect of the two methods (traditional and trace tool method) was compared in the therapeutic exercises on pain and ROM in patients with knee osteoarthritis. The results revealed a significant difference between the intervention and control groups regarding the ROM of knee flexion. Furthermore, the result of the satisfaction questionnaire showed a significant difference between the two groups, with a higher median score in the intervention group than in the control group [24].
Marin-Pardo et al. developed a telerehabilitation biofeedback system for muscle training for people suffering post-stroke. The system was a portable stroke telerehabilitation at home, therapist-driven, personalized, and gamified training. They evaluated the systems’s performance in training tasks on a person with a stroke. The results showed that the participant reported no perceived discomfort, pain, or fatigue, and no adverse events were observed during any sessions using the system. Values of calculated individuated activity of the extensor muscle showed a significant increase over time (P<0.001) [25]. However, this system needed a laptop and several sensors to save signals on the electromyography system. Despite this, authors tried to develop a low-cost system, but it is relatively expensive and complicated for some people with low comprehension.
Blair et al. invented a physical therapy device (patent number US8721569 B2) to perform the physical therapy exercise. Users should move their limbs in such a manner to track light from the light emitter on the tracking pattern and perform physical therapy exercises [26]. Although the procedure of this device was not complicated, the users should place their foot on a box to perform exercises to have a proper position during the exercises. Since, some patients cannot stand independently, and it may be fatiguing for them, this device may not be suitable for many patients.
Priester et al. developed a joint angle indication system (patent number US6890312 B1). The joint angle indication system provided information about the angular relationship between a first body part and a second body part. The system included several joint angle variation sensors that vary based on the joint angle between the first and second arm members. An audio biofeedback circuit generated a first feedback signal when the joint angle was less than or equal to the first angle, generated a second feedback signal when the joint angle was greater than or equal to the second angle, and generated no feedback signal when the joint angle was less than the second angle and more significant than the first angle [27]. Although based on our current knowledge, no study was found to show the effect of this device on performing therapeutic exercises in patients, it seems that this device determines the joint angles correctly, and users can perform the exercises at the precisely determined angle. However, this device was limited to use in the upper limbs, and for use in other joints, it requires a specific design of the device and cuffs.
Since the researcher has conducted the present study during the COVID-19 period, some limitations, such as the absence of the control group and only evaluation of clinical outcomes, not laboratory outcomes were met. The long-term effect of the studied tool on participants in the exercises resulted in confirming the tools effectiveness. Additionally, the effect of the audio biofeedback device should be investigated during therapeutic exercises in groups of patients with musculoskeletal disorders who require ongoing therapeutic exercises.
It suggests the use of audio biofeedback tool to perform movements in other joints. It is suggested that future studies should compare the methods of performing therapeutic exercises with the biofeedback tool with traditional methods in a clinical trial study.
Conclusion
The present pilot study has shown that the proposed audio biofeedback device is feasible, safe, and acceptable. The biofeedback tool seduced the participants to complete therapeutic exercises. Employing the audio biofeedback tool for children, the elderly, and people with low attention and concentration can attract attention and increase participation in therapeutic exercises. Also, it seems that the use of the tool can help complete complicated exercises at certain angles.
Ethical Considerations
Compliance with ethical guidelines
The ethical code of the present study was IR.IUMS.REC.1398.1141 which was obtained from the Ethics Committee of Iran University of Medical Sciences. In addition, the objectives of the study were fully explained to the participants and then the written informed consent form was provided to the participants.
Funding
This research was supported by the research project funded by Iran University of Medical Sciences, Tehran, Iran.
Conflict of interest
The author declared no conflict of interest.
Acknowledgments
The author also thanks the Iran University of Medical Sciences for partially funding this study.
References
Stroke may lead to disabilities in daily activities [1]. Loss of function, especially in hand, leads to severe physical and mental disabilities that affect daily activities, including working conditions and quality of life [2]. The prevalence of stroke in developed countries is about 100-300 cases per 100 000 people per year [3]. Studies have shown that stroke is the third cause of disability [4]. A total of 45% of elderly people with stroke are severely unable to perform daily functions.
Adherence to exercise programs is usually a challenge for therapists. Its effectiveness of some factors, including the exercise protocol and patient participation [5]. Despite the effect of exercise and exercise therapy on physical and social health for the elderly with disabilities, participating in exercise and exercise therapy is still weak among them [6, 7]. Campbell et al. showed that non-compliance with physiotherapy is common. From the patient’s perspective, the decision to comply or not to comply is rational but often unpredictable by therapists or researchers [8]. Less participation in exercise and therapeutic exercise may correlate to general factors, such as fear of adverse consequences and lack of motivation [6, 7].
Using supervised exercise sessions, referring patients for regular consultation with a physician, or attending group exercise classes may help ensure long-term exercise compliance and improve therapeutic outcomes [4]. Referring patients to clinics or group sessions to do therapeutic exercises is costly and time-consuming and is not always available for elderly patients [9, 10]. Regarding the importance of health protocols in the COVID-19 epidemic, especially for the elderly, a method is required to do therapeutic exercises at home without attending medical centers [9].
Due to physical and cognitive disorders, it is often difficult and costly for people who have suffered a stroke to access on-site rehabilitation. Telerehabilitation offers the opportunity to promote the rehabilitation process [11]. According to other recent studies, telerehabilitation shows a positive impact on patients’ compliance and adherence [12, 13] because the patients’ opinions are crucial [14]. This trial contributes to the scientific-based knowledge regarding the effects of telerehabilitation and the increase in participation. Complicating and challenging exercises lead to non-adherence to treatment [15].
In addition, based on the International Organization for Standardization, the usability of using the product to achieve particular goals, effectiveness, efficiency, and user satisfaction are considered in a certain scope [16]. In the current study, one of the most critical steps was “usability” testing to collect empirical data from users and learn the usage, efficiency, tool durability, and safety [17], useful for identifying problems with existing tools. According to Nielsen, usability testing of five users should identify up to 80% of potential problems with a particular tool [18, 19]. Williams stated that the level of patients’ satisfaction can show its quality, i.e. the higher quality, the higher patient satisfaction [20].
The present study was conducted to develop a tool based on audio biofeedback and increase the rate of participation in therapeutic exercise, i.e. people with stroke do their therapeutic exercises with high attractiveness under the practices and standards considered by the therapist at home.
Materials and Methods
Audio biofeedback (Figure 1) is an invention (registration No A61B 5/00) (Attachment). The device included an audio biofeedback box (including battery, sound alarm, on and off switch, and two LED lamps), connecting wire (including two connecting cables, two connecting wires, and two rotating plates to adjust the joint angle, each consisting of a mercury lamp), joint strap (one strap with velcro, one magnet to connect to the rotating plates of the lamp). Two small lamps were placed on both sides of the sound alarm and turned on and off when the alarm turned on and off; therefore they were as visual biofeedback.
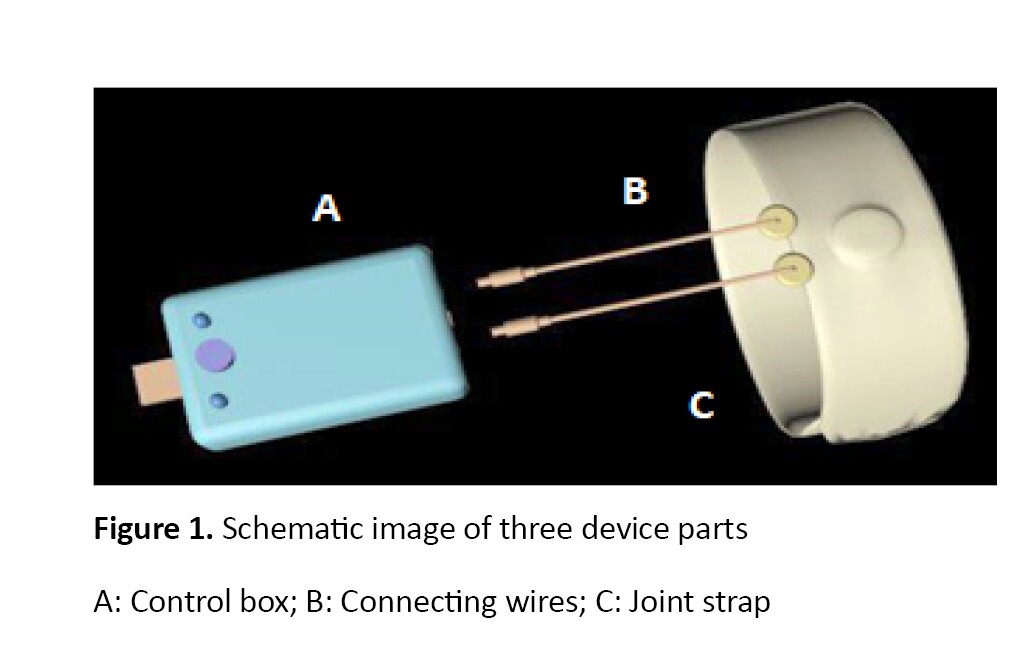
Figure 2 shows the biofeedback box. The two rotating plates were used to adjust the angles. After the wrist reached the desired angle, the alarm was turned on and sounded.

Table 1 presents the summary of the device features.
Study design and participants
This pilot study was conducted at Iran University of Medical Sciences. A total of 28 healthy students were included from Iran University of Medical Sciences. The participants were selected based on convenience and non-probability sampling method and the inclusion criteriaincluded aged 18 to 25 years, no pain in upper limbs, no spasticity in upper limbs, no disability in upper limbs, and a full range of motion (ROM) of the wrist. The exclusion criteria included unwillingness to continue the test. Table 2 presents the subjects’ age, weight, height, and size of wrist before the study. A sample size was estimated by G-power software and according to a power of 95%, and a one-sided significance level of 0.05. A sample size of 28 healthy people was needed [21].

Data collection
For all participants, the following outcome measurements were evaluated, demographic data, wrist size, responsiveness in ROM of the wrist, time of device responsiveness, and participants’ satisfaction. Primary outcome measures were the device feasibility in wrist ROM and device feasibility time; the secondary outcome measure was participants’ satisfaction with the device process (please see attachments) [19, 22].
At first, the evaluator asked each participant to sit on a chair. Second, the evaluator tied the strap to his wrist. Third, the evaluator rotated the two small rotating plates to the desired amount in the counterclockwise direction and then asked each volunteer to move the wrist in the extension and the flexion. When the tool warned, i.e. the movement was done in the correct direction.
The researcher considered three angles 0°, 30° extension, and 30° flexion. The evaluator set the device at each angle and asked participants to move their wrists at certain angles and keep those till the tool was warned. When the device was warned, the evaluator measured the participants’ wrist angle. The evaluator measured the time between the time the wrist reached certain angles, and when the device warned as the time of device responsiveness. To decrease errors, the evaluator repeated all of the tests three times. In the end, the evaluator asked participants to fill up the satisfaction questionnaire on five-point Likert scale [19, 22].
Results
The results showed that the device was efficient for all participants in 0°. Two participants did not show the correct angle in the 30°flexion by the device. Also, two participants did not show the 30° extension correctly by the device. Tables 3 and 4 present the result of device feasibility and responsibility of time. The results of the Fridman test showed no significant difference between the three-time trials (P=0.110) for each angle. Figure 1 shows the average score for each item of the satisfaction questionnaire. A score above the optimal threshold (2.5) was considered for each question.

Discussion
Telerehabilitation has attracted more attention from society (the research community and the commercial market) [23]. The results showed that the audio biofeedback device is efficient in the evaluated angles. Also, the device gave feedback in less than 15 hundredths of a second. The results of this study are beneficial for rehabilitation centers and clinics.
Based on the results of the satisfaction questionnaire, all participants were assigned a score higher than the optimal threshold for every question. The highest score was 5 (the easy learning of the tool), it means the device has a simple process for its users. Therefore, many users who cannot understand complex devices easily perform exercises with the studied device. Since exercise with the device designed in this study does not require any clinical travel and high costs, it has better follow-up of patients with stroke and other disabilities in the wrist in doing therapeutic exercises and saving time with better availability.
Nowadays, due to outbreaks of pandemic diseases, telerehabilitation has attracted the attention of many disabled people, therapists, and researchers [11]. In this article, the researcher tried to aid the telerehabilitation process by introducing a biofeedback tool. In a similar study, the effect of the two methods (traditional and trace tool method) was compared in the therapeutic exercises on pain and ROM in patients with knee osteoarthritis. The results revealed a significant difference between the intervention and control groups regarding the ROM of knee flexion. Furthermore, the result of the satisfaction questionnaire showed a significant difference between the two groups, with a higher median score in the intervention group than in the control group [24].
Marin-Pardo et al. developed a telerehabilitation biofeedback system for muscle training for people suffering post-stroke. The system was a portable stroke telerehabilitation at home, therapist-driven, personalized, and gamified training. They evaluated the systems’s performance in training tasks on a person with a stroke. The results showed that the participant reported no perceived discomfort, pain, or fatigue, and no adverse events were observed during any sessions using the system. Values of calculated individuated activity of the extensor muscle showed a significant increase over time (P<0.001) [25]. However, this system needed a laptop and several sensors to save signals on the electromyography system. Despite this, authors tried to develop a low-cost system, but it is relatively expensive and complicated for some people with low comprehension.
Blair et al. invented a physical therapy device (patent number US8721569 B2) to perform the physical therapy exercise. Users should move their limbs in such a manner to track light from the light emitter on the tracking pattern and perform physical therapy exercises [26]. Although the procedure of this device was not complicated, the users should place their foot on a box to perform exercises to have a proper position during the exercises. Since, some patients cannot stand independently, and it may be fatiguing for them, this device may not be suitable for many patients.
Priester et al. developed a joint angle indication system (patent number US6890312 B1). The joint angle indication system provided information about the angular relationship between a first body part and a second body part. The system included several joint angle variation sensors that vary based on the joint angle between the first and second arm members. An audio biofeedback circuit generated a first feedback signal when the joint angle was less than or equal to the first angle, generated a second feedback signal when the joint angle was greater than or equal to the second angle, and generated no feedback signal when the joint angle was less than the second angle and more significant than the first angle [27]. Although based on our current knowledge, no study was found to show the effect of this device on performing therapeutic exercises in patients, it seems that this device determines the joint angles correctly, and users can perform the exercises at the precisely determined angle. However, this device was limited to use in the upper limbs, and for use in other joints, it requires a specific design of the device and cuffs.
Since the researcher has conducted the present study during the COVID-19 period, some limitations, such as the absence of the control group and only evaluation of clinical outcomes, not laboratory outcomes were met. The long-term effect of the studied tool on participants in the exercises resulted in confirming the tools effectiveness. Additionally, the effect of the audio biofeedback device should be investigated during therapeutic exercises in groups of patients with musculoskeletal disorders who require ongoing therapeutic exercises.
It suggests the use of audio biofeedback tool to perform movements in other joints. It is suggested that future studies should compare the methods of performing therapeutic exercises with the biofeedback tool with traditional methods in a clinical trial study.
Conclusion
The present pilot study has shown that the proposed audio biofeedback device is feasible, safe, and acceptable. The biofeedback tool seduced the participants to complete therapeutic exercises. Employing the audio biofeedback tool for children, the elderly, and people with low attention and concentration can attract attention and increase participation in therapeutic exercises. Also, it seems that the use of the tool can help complete complicated exercises at certain angles.
Ethical Considerations
Compliance with ethical guidelines
The ethical code of the present study was IR.IUMS.REC.1398.1141 which was obtained from the Ethics Committee of Iran University of Medical Sciences. In addition, the objectives of the study were fully explained to the participants and then the written informed consent form was provided to the participants.
Funding
This research was supported by the research project funded by Iran University of Medical Sciences, Tehran, Iran.
Conflict of interest
The author declared no conflict of interest.
Acknowledgments
The author also thanks the Iran University of Medical Sciences for partially funding this study.
References
- Pinto SM, Galang G. Concurrent SCI and TBI: Epidemiology, shared pathophysiology, assessment, and prognostication. Curr Phys Med Rehabil Rep. 2016; 4(1):71-9. [DOI:10.1007/s40141-016-0109-6]
- Almenara M, Cempini M, Gómez C, Cortese M, Martín C, Medina J, et al. Usability test of a hand exoskeleton for activities of daily living: An example of user-centered design. Disabil Rehabil Assist Technol. 2017; 12(1):84-96. [DOI:10.3109/17483107.2015.1079653] [PMID]
- Dalvandi A, Ekman SL, Maddah SSB, Khankeh HR, Heikkilä K. Post stroke life in iranian people: Used and recommended strategies. Iran Rehabil J. 2009; 7(1):17-24. [Link]
- Bennell KL, Hinman RS. A review of the clinical evidence for exercise in osteoarthritis of the hip and knee. J Sci Med Sport. 2011; 14(1):4-9. [DOI:10.1016/j.jsams.2010.08.002] [PMID]
- Bruce-Brand RA, Walls RJ, Ong JC, Emerson BS, O'Byrne JM, Moyna NM. Effects of home-based resistance training and neuromuscular electrical stimulation in knee osteoarthritis: A randomized controlled trial. BMC Musculoskelet Disord. 2012; 13:118. [DOI:10.1186/1471-2474-13-118] [PMID]
- Kontos PC, Miller KL, Brooks D, Jassal SV, Spanjevic L, Devins GM, et al. Factors influencing exercise participation by older adults requiring chronic hemodialysis: A qualitative study. Int Urol Nephrol. 2007; 39(4):1303-11. [DOI:10.1007/s11255-007-9265-z] [PMID]
- Billinger SA, Arena R, Bernhardt J, Eng JJ, Franklin BA, Johnson CM, et al. Physical activity and exercise recommendations for stroke survivors: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014; 45(8):2532-53. [DOI:10.1161/STR.0000000000000022] [PMID]
- Campbell R, Evans M, Tucker M, Quilty B, Dieppe P, Donovan JL. Why don't patients do their exercises? Understanding non-compliance with physiotherapy in patients with osteoarthritis of the knee. J Epidemiol Community Health. 2001; 55(2):132-8.[DOI:10.1136/jech.55.2.132] [PMID]
- Azma K, RezaSoltani Z, Rezaeimoghaddam F, Dadarkhah A, Mohsenolhosseini S. Efficacy of tele-rehabilitation compared with office-based physical therapy in patients with knee osteoarthritis: A randomized clinical trial. J Telemed Telecare. 2018; 24(8):560-5. [DOI:10.1177/1357633X17723368] [PMID]
- Rao K, Iyer C, Anap D. Can telerehabilitation add a new dimension in the treatment of osteoarthritis knee. J Pain Relief. 2012; 1(5):1000113. [Link]
- Klamroth-Marganska V, Giovanoli S, Easthope CA, Schönhammer JG. Telerehabilitation technology. In: Reinkensmeyer DJ, Marchal-Crespo L, Dietz V, editors. Neurorehabilitation technology. New York: Springer; 2022. [DOI:10.1007/978-3-031-08995-4_25]
- Moffet H, Tousignant M, Nadeau S, Mérette C, Boissy P, Corriveau H, et al. In-home telerehabilitation compared with face-to-face rehabilitation after total knee arthroplasty: A noninferiority randomized controlled trial. J Bone Joint Surg Am. 2015; 97(14):1129-41. [DOI:10.2106/JBJS.N.01066] [PMID]
- Chen M, Li P, Lin F. Influence of structured telephone follow-up on patient compliance with rehabilitation after total knee arthroplasty. Patient Prefer Adherence. 2016; 10:257-64. [DOI:10.2147/PPA.S102156] [PMID]
- Pastora-Bernal JM, Martín-Valero R, Barón-López FJ, Estebanez-Pérez MJ. Evidence of benefit of telerehabitation after orthopedic surgery: A systematic review. J Med Internet Res. 2017; 19(4):e142. [DOI:10.2196/jmir.6836] [PMID] [PMCID]
- Dobson F, Bennell KL, French SD, Nicolson PJ, Klaasman RN, Holden MA, et al. Barriers and facilitators to exercise participation in people with hip and/or knee osteoarthritis: Synthesis of the literature using behavior change theory. Am J Phys Med Rehabil. 2016; 95(5):372-89. [DOI:10.1097/PHM.0000000000000448] [PMID]
- Iso. Ergonomics of human-system interaction [Internet]. 2014 [Updated 2023 December 31]. Available from: [Link]
- Dumas JS, Redish JC. A practical guide to usability testing. Bristol: Intellect books; 1999. [Link]
- Nielsen J. Usability Testing. In: Nielsen J, editor. Usability engineering. Amsterdam: Elsevier Inc; 1994. [DOI:10.1016/B978-0-08-052029-2.50009-7]
- Jiryaei Z, Alvar AA, Bani MA, Vahedi M, Jafarpisheh AS, Razfar N. Development and feasibility of a soft pneumatic-robotic glove to assist impaired hand function in quadriplegia patients: A pilot study. J Bodyw Mov Ther. 2021; 27:731-6. [DOI:10.1016/j.jbmt.2021.03.012] [PMID]
- Williams B. Patient satisfaction: A valid concept? Soc Sci Med. 1994; 38(4):509-16. [DOI:10.1016/0277-9536(94)90247-X] [PMID]
- Mau-Moeller A, Behrens M, Finze S, Bruhn S, Bader R, Mittelmeier W. The effect of continuous passive motion and sling exercise training on clinical and functional outcomes following total knee arthroplasty: A randomized active-controlled clinical study. Health Qual Life Outcomes. 2014; 12:68. [DOI:10.1186/1477-7525-12-68] [PMID]
- Encarnação P, Cook A. Robotic assistive technologies: Principles and practice. Boca Raton: CRC Press; 2017. [DOI:10.4324/9781315368788]
- Moral-Munoz JA, Zhang W, Cobo MJ, Herrera-Viedma E, Kaber DB. Smartphone-based systems for physical rehabilitation applications: A systematic review. Assist Technol. 2021; 33(4):223-36. [DOI:10.1080/10400435.2019.1611676] [PMID]
- Jiryaei Z, Rezaei M, Jiryaei A, Niknami S. Usability testing of a new tool for tracking therapeutic exercise patterns in patients with knee osteoarthritis. Middle East J Rehabiln Health Stud. 2022; 9(1):e119166. [DOI:10.5812/mejrh.119166]
- Marin-Pardo O, Phanord C, Donnelly MR, Laine CM, Liew SL. Development of a low-cost, modular muscle-computer interface for at-home telerehabilitation for chronic stroke. Sensors. 2021; 21(5):1806. [DOI:10.3390/s21051806] [PMID]
- Gordon Talmadge Blair I. Physical therapy device [Internet]. 2014 [Updated 2023 December 31]. Available from: [Link]
- Priester WB, Butler Jr JH, Twigg MJ. Joint angle indication system [Internet]. 2005 [Updated 2023 December 31]. Available from: [Link]
Type of Study: Research |
Subject:
Physiotherapy
Received: 2023/08/5 | Accepted: 2023/09/4 | Published: 2023/02/12
Received: 2023/08/5 | Accepted: 2023/09/4 | Published: 2023/02/12