Volume 5, Issue 1 (Continuously Updated 2022)
Func Disabil J 2022, 5(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghafari Z, Noorizadeh Dehkordi S, Nikjooy A, Mousavi Khatir S R, Moghaddasi M. The Effect of Pelvic Floor Muscle Exercises Therapy on the Fatigue and Quality of Life in Multiple Sclerosis Women With Urinary Disorders. Func Disabil J 2022; 5 (1) : 65
URL: http://fdj.iums.ac.ir/article-1-215-en.html
URL: http://fdj.iums.ac.ir/article-1-215-en.html
Zahra Ghafari1 

 , Shohreh Noorizadeh Dehkordi *2
, Shohreh Noorizadeh Dehkordi *2 

 , Afsaneh Nikjooy1
, Afsaneh Nikjooy1 

 , Seyedeh Roghayeh Mousavi Khatir3
, Seyedeh Roghayeh Mousavi Khatir3 

 , Mehdi Moghaddasi4
, Mehdi Moghaddasi4 




 , Shohreh Noorizadeh Dehkordi *2
, Shohreh Noorizadeh Dehkordi *2 

 , Afsaneh Nikjooy1
, Afsaneh Nikjooy1 

 , Seyedeh Roghayeh Mousavi Khatir3
, Seyedeh Roghayeh Mousavi Khatir3 

 , Mehdi Moghaddasi4
, Mehdi Moghaddasi4 


1- Department of Physiotherapy, Iranian Center of Excellence in Physiotherapy, Rehabilitation Research Center, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Physiotherapy, Iranian Center of Excellence in Physiotherapy, Rehabilitation Research Center, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran. ,noorizadeh.sh@iums.ac.ir
3- Department of Physical Therapy, Faculty of Rehabilitation, Tehran University of Medical Sciences, Tehran, Iran.
4- Department of Neurology, Skull Base Research Center, Five Senses Health Research Institute, Hazrat-E Rasool General Hospital, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Physiotherapy, Iranian Center of Excellence in Physiotherapy, Rehabilitation Research Center, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran. ,
3- Department of Physical Therapy, Faculty of Rehabilitation, Tehran University of Medical Sciences, Tehran, Iran.
4- Department of Neurology, Skull Base Research Center, Five Senses Health Research Institute, Hazrat-E Rasool General Hospital, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 1278 kb]
(499 Downloads)
| Abstract (HTML) (1806 Views)
Full-Text: (681 Views)
Introduction
Multiple Sclerosis (MS) is the most common inflammatory disease of the central nervous system that causes urinary disorders in these people. Urinary problems are seen in more than 50% of MS patients [1]. Urinary disorders in MS patients in the form of increased daily urinary frequency, nocturia, stress urinary incontinence and urgency, enuresis, slow flow of urine, the spread of urine flow, interruption, delay, straining to urinate, final dripping, the sensation of incomplete emptying and dripping of urine occurs after urination [2]. Urinary disorders have a great impact on people’s quality of life (QoL) by reducing self-confidence, depression, anxiety, social isolation, leaving jobs, and reducing motivation. It can also reduce the quality of sleep after nocturnal enuresis and make the person tired the next day. Also, people who have urinary disorders usually reduce their water intake, and dehydration is another factor that can aggravate fatigue, and as we know, fatigue is one of the most debilitating symptoms of MS. Also, factors, such as leakage of urine, reduction of water consumption, and increased residual volume of urine can cause urinary infections, which can increase the probability of attack, and progression of the disease, hospitalization, and death of people with MS [3-9]. The goal of all therapeutic interventions to manage urinary problems is to improve the patients’ QoL in the first step and to prevent long-term damage to the bladder and urinary infections in the next step. Exercise therapy is the first line of treatment in people with urinary incontinence caused by MS. Studies have shown that 56% to 70% of MS patients improve urinary disorders by doing therapeutic exercises [10-13].
The effects of pelvic floor muscle exercises have been reviewed in several articles. Articles have shown that pelvic floor exercises can make positive changes in the strength of pelvic floor muscles [14], 24-hour pad test [15], number of nocturnal urination [15], number of pad use [14], defecation episodes of urine [14], and QoL [16]. In a systematic study, it was also stated that pelvic floor muscle exercises are more effective than other non-drug treatments for urinary disorders [17, 18]. In addition, studies were conducted that investigated the effect of postural balance exercises, functional mobility exercises, aerobic exercise at home, regular physical exercises, and water therapy on the fatigue of individuals with MS [19-21]. However, among the studies, the effect of pelvic floor exercise on the fatigue of patients with MS was not observed. Also, few studies mentioned the role of awareness of the pelvic floor before doing the exercises [22].
Therefore, this research was conducted to investigate the effect of specific pelvic floor exercises at home along with increasing awareness of pelvic floor muscles on the level of fatigue and QoL of women with urinary problems caused by MS. In this study, people were given exercises at home to partially control the effect of this confounding variable on fatigue.
Materials and Methods
The current study was a double-blind randomized clinical trial that was conducted in parallel with two control and intervention groups. The studied population was women with urinary disorders caused by MS in the age group of 18 to 50 years. The non-probability sampling method was used. In this study, after obtaining the consent form of the participants, people were divided into two groups based on the expanded disability status scale (EDSS) and the type of urinary disorder using a sealed envelope method. Referring to similar articles [23, 24], the sample size is equal to 30 people, with 15 people in each group.
After the initial evaluations, the patients voluntarily entered the study if they met the inclusion criteria. All participants completed the consent form to participate in the study. The inclusion criteria for the study included the following items, women with MS with relapses and remissions diagnosed by a neurologist, in the age range of 18-50 years, the measurement score of mental health based on mini-mental state examination (MMSE) questionnaire should be higher than 18, disability score based on EDSS questionnaire should be less than seven, urinary disorder based on 8-item Overactive Bladder (OAB-V8) questionnaire should be higher than eight, they should not have had an attack in the last three months and in the dosage of drugs, there have been no changes related to urinary disorders of people in the last three months. Also, the exclusion criteria of people included having an attack during the study, becoming pregnant during the study, and having a urinary infection.
The participants visited the clinic for a total of two sessions. In the first session, to know more about pelvic floor muscles, the anatomy and function of pelvic floor muscles were explained to each participant along with pictures. The prerequisite for doing exercises and contracting the pelvic floor muscles was to know about the pelvic floor muscles. In this study, for this purpose, we placed a rolled towel on the pelvic floor area of the participants while they were sitting on the edge of the bed. Then, we asked each participant to try to separate their seat from the towel by pulling up and gathering the pelvic floor. Then, after ensuring that the pelvic floor muscles were properly contracted, each participant lay down on the bed in an arched position, and tone management exercises, breathing exercises, stretching, and strengthening of the pelvic floor muscles were taught to each participant. In this session, participants were given a bladder diary form to fill it at home for three consecutive days, and based on the information on this form, urinary behavior counseling was given to them verbally and in writing in the second session. Based on this training, the pattern of proper nutrition and behavioral therapy of the participants was explained according to their urinary disorder. In the second session, the exercises were repeated for each participant.
The exercises were explained to each participant during the first and second sessions and the correctness of the exercises was repeated three or more times for each participant. The exercises included tone management exercises, diaphragmatic breathing, stretching of thigh adductor muscles, piriformis, and external rotators, and strengthening of pelvic floor muscles in different positions (from lower to the upper center of gravity). The order of exercises was done by the participants as warm-up, pelvic floor strengthening exercises, and then cooling down. Warm-up and cool-down exercises included tone management, stretching, and diaphragmatic breathing exercises. The exercises were done daily by the participants at home for eight weeks. Stretching exercises for 30 s and strengthening exercises with holding for 3 s and resting for 6 seconds and repeating two sets of 10 per day were prescribed. The therapist followed up the process of doing the exercises weekly (telephone call three times a week).
Data collection
First, the demographic information of the participants was recorded. Before the intervention, the participants completed Qualiveen-30 questionnaire and Modified Fatigue Impact Scale (MFIS). Qualiveen-30 evaluates the QoL affected by urinary disorders in people with spinal cord injury and MS. This questionnaire measures the QoL in four subgroups, harassment (including 9 questions), coercion or restriction (including 8 questions), worry (including 8 questions) and emotions (including 5 questions) and a higher score in this questionnaire indicates a person’s lower QoL. The validity and reliability of this questionnaire were conducted in Iran in 2015 [25]. The MFIS questionnaire is designed to measure the level of fatigue of people with MS in 21 questions, which examines the level of fatigue in three subgroups, physical, cognitive, and psychosocial. A higher score in this questionnaire indicates a higher level of fatigue in people. The validity and reliability of this questionnaire were conducted in Iran in 2013 [26], in this study, the bladder diary form was used only to provide counseling on urinary behavior. To complete the bladder diary form, the participant must complete the form carefully at home for three consecutive days, considering the type of urinary disorder. At the end of the study, participants filled out the MFIS and Qualiveen-30 forms again.
Results
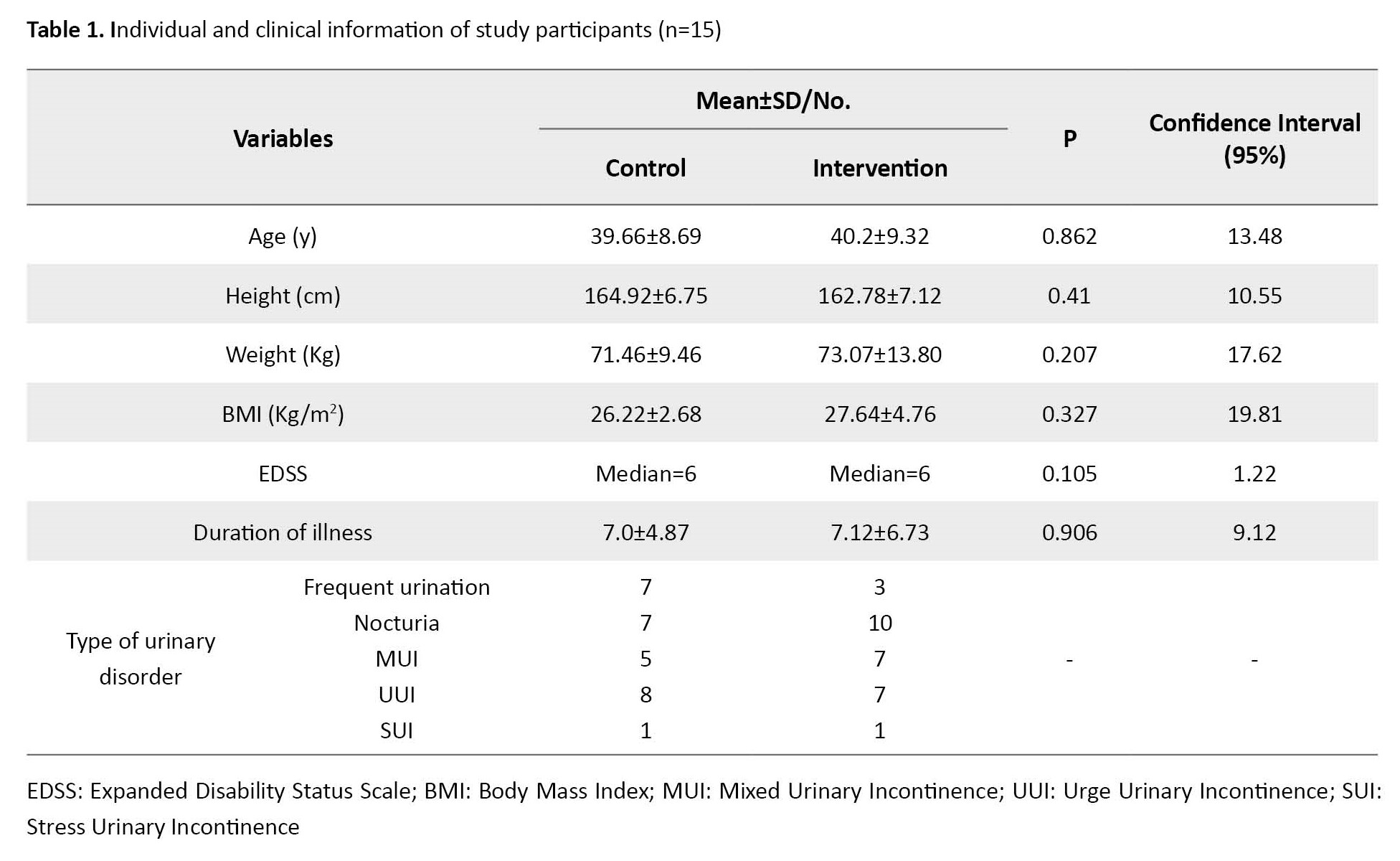
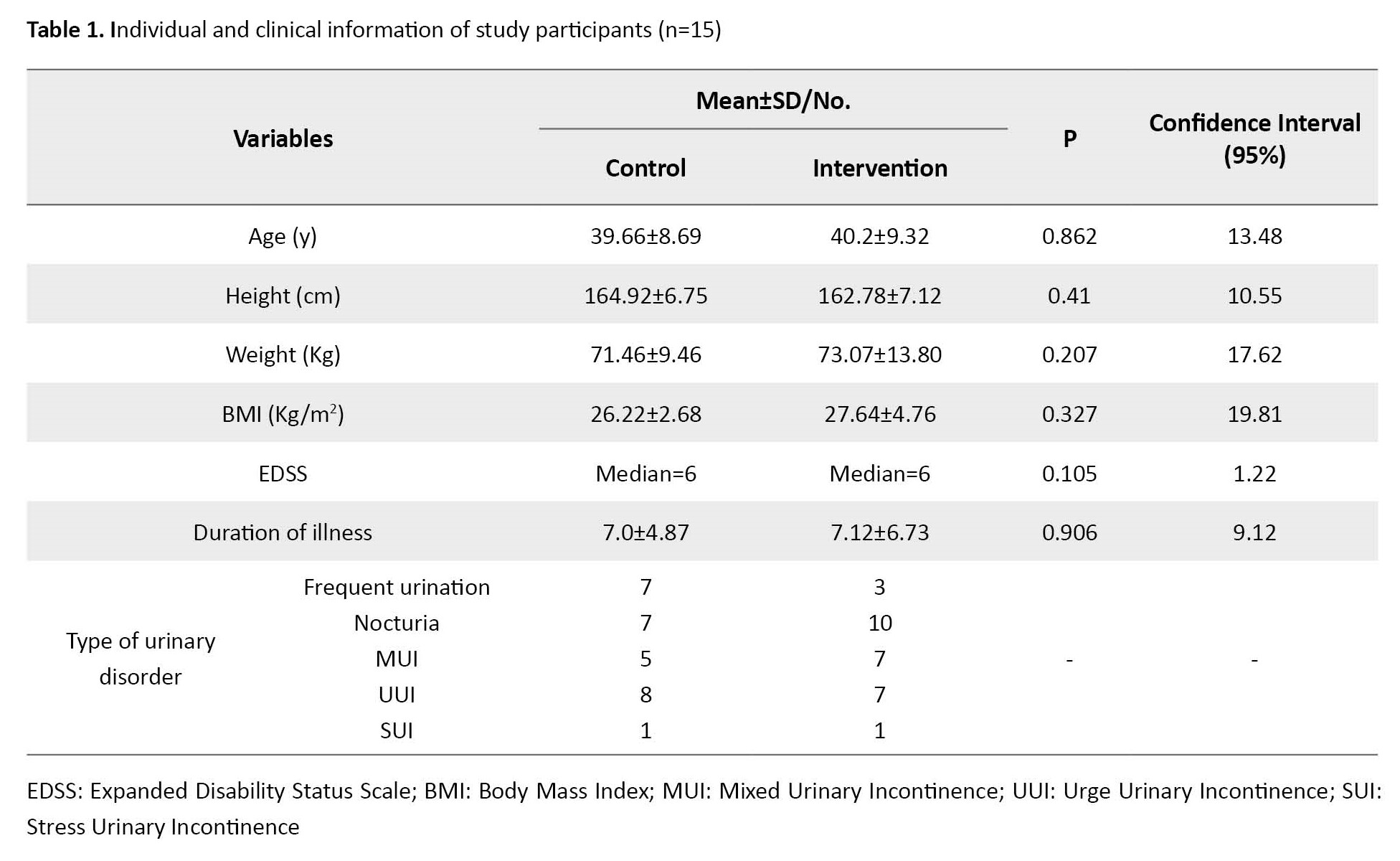
This study was conducted in 2022. All participants completed the study. Table 1 shows the personal and clinical information of the study participants. The type of urinary disorder is shown in the table. Many participants expressed several disorders at the same time, therefore the table shows the number of participants who had each disorder.
Based on the results, all the data in both groups followed the normal distribution before and after the study. Therefore, in this study, a parametric t-test was used. In the comparison between groups, we used the independent sample t-test and the paired sample t-test for within-group comparison.
Fatigue
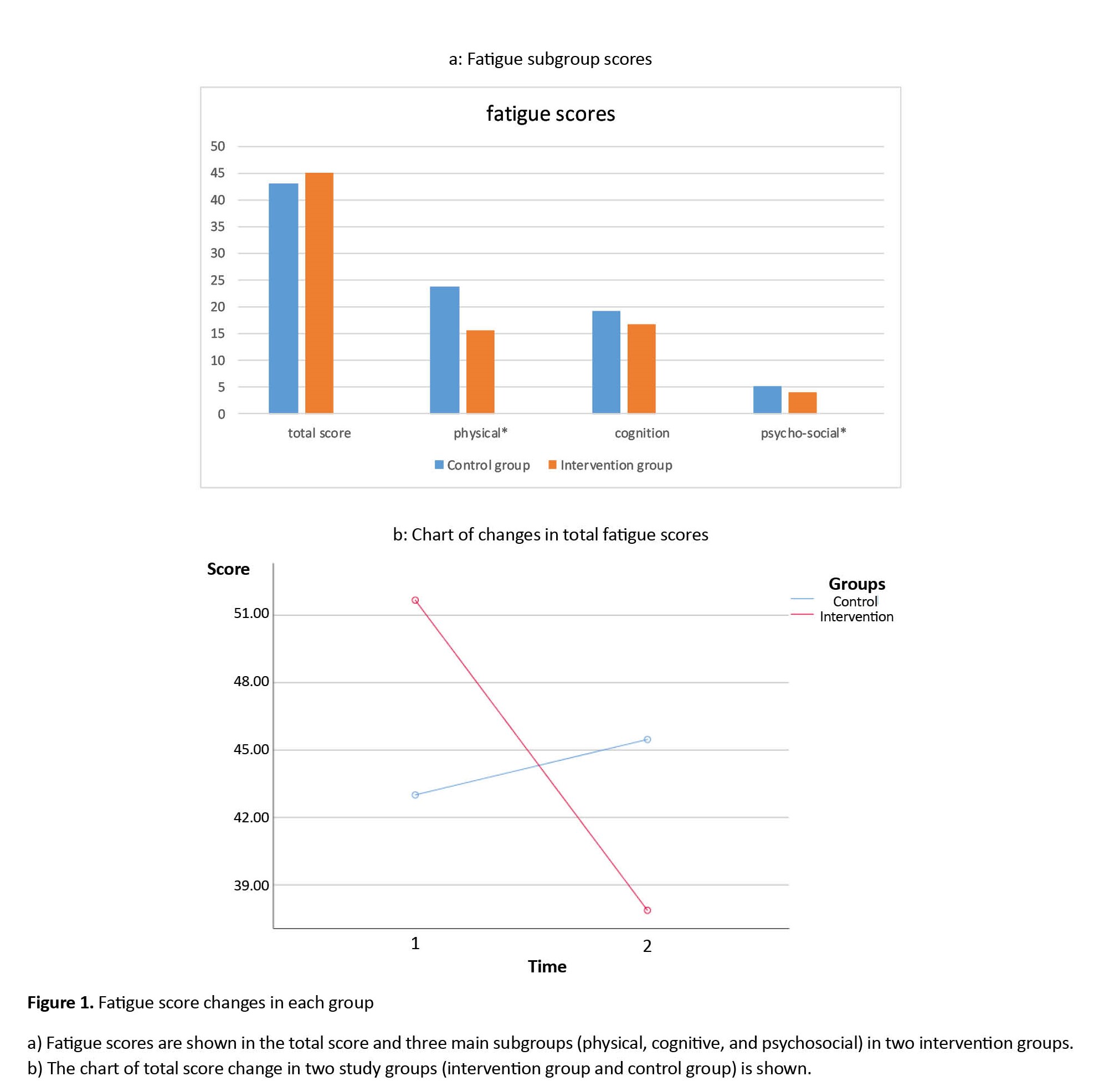
Table 2 presents the comparison results before and after the study. After the study, a significant difference was found in the total score and all variables related to fatigue in the intervention group (P<0.05).
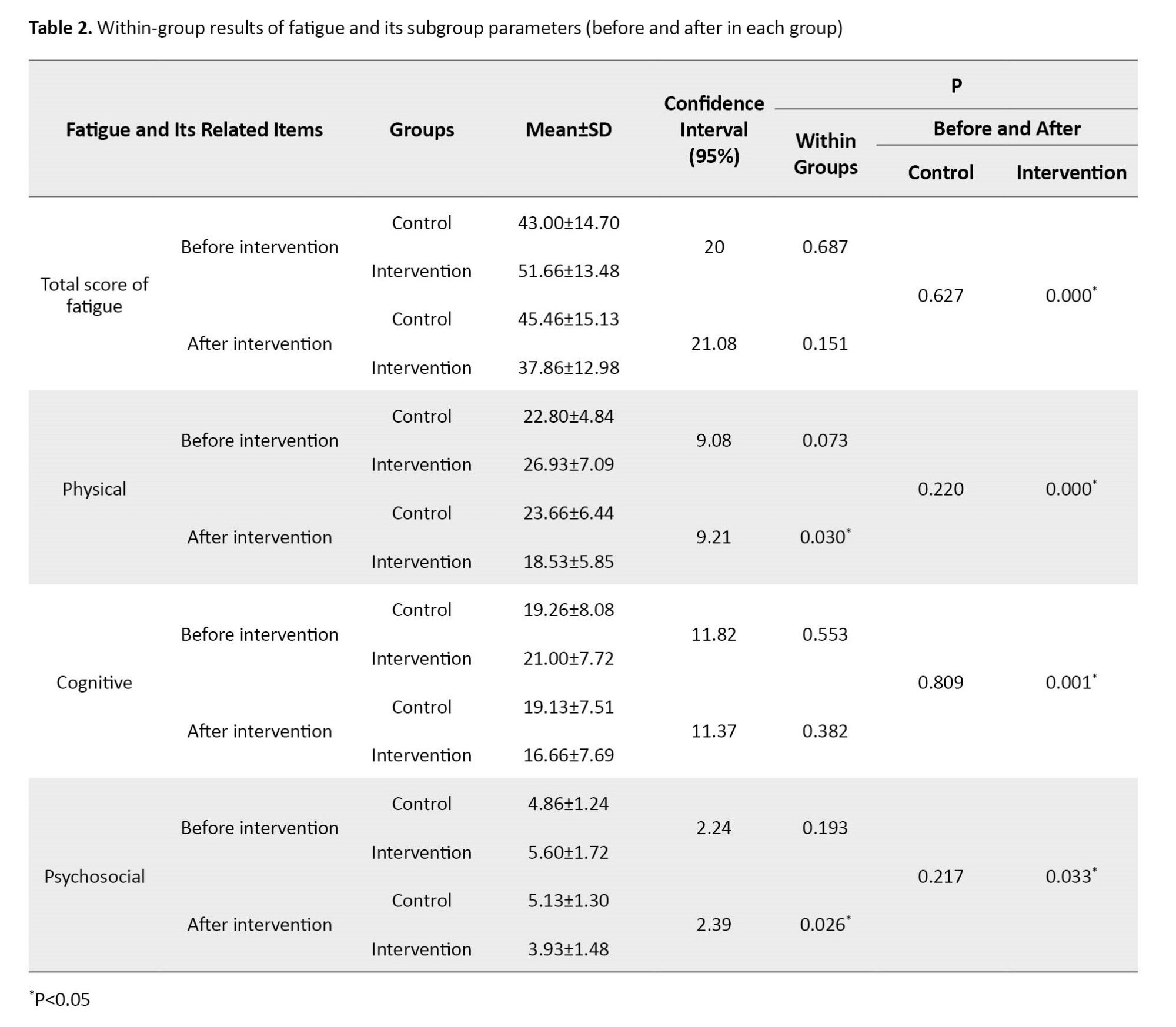
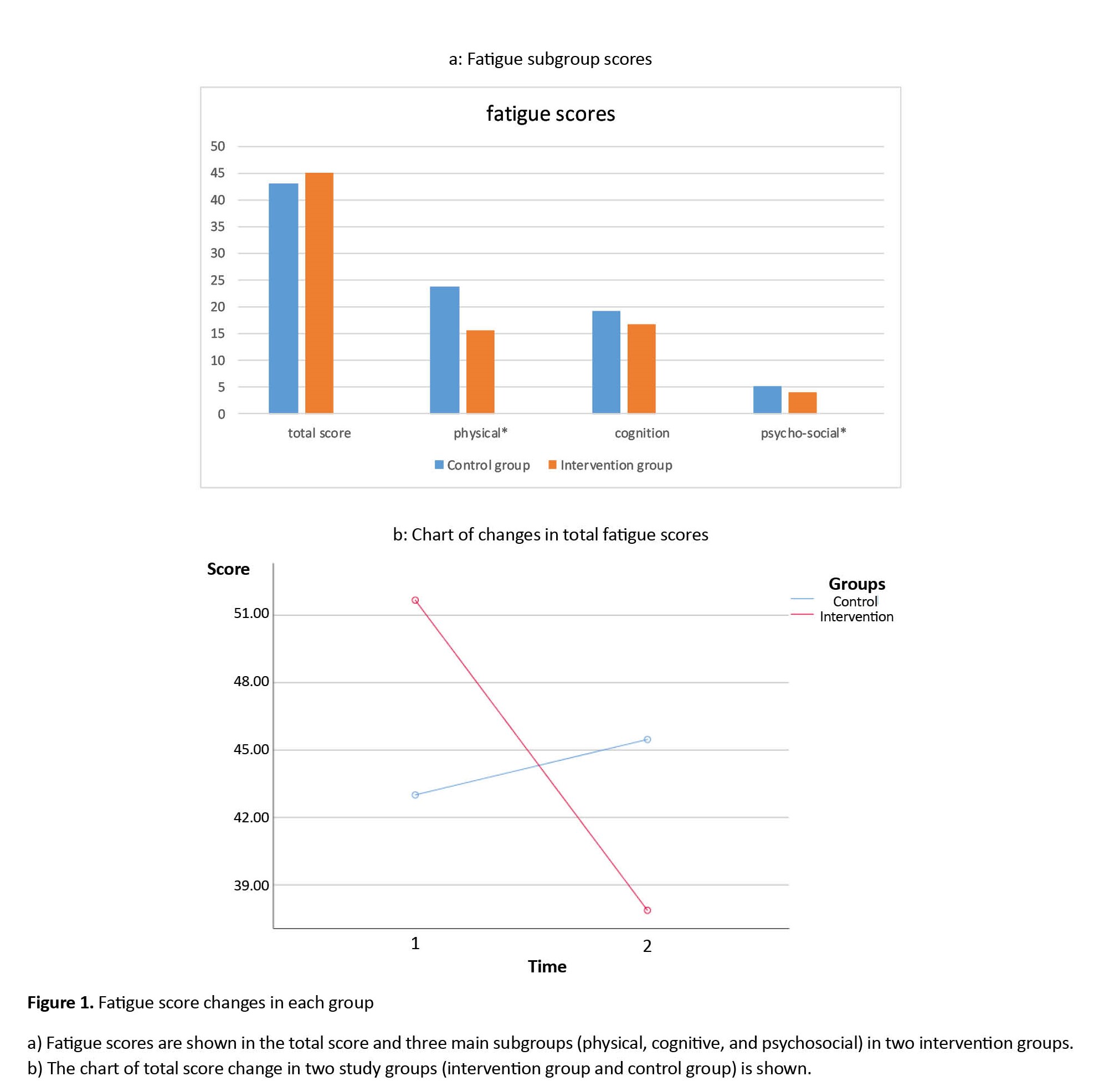
Also, the results showed that after the study, a significant difference was found in the physical and psychosocial subgroups between the two intervention and control groups (P<0.05). A graph shows the average scores of two groups after the study. Also, Figure 1 shows the total score changes.
QoL
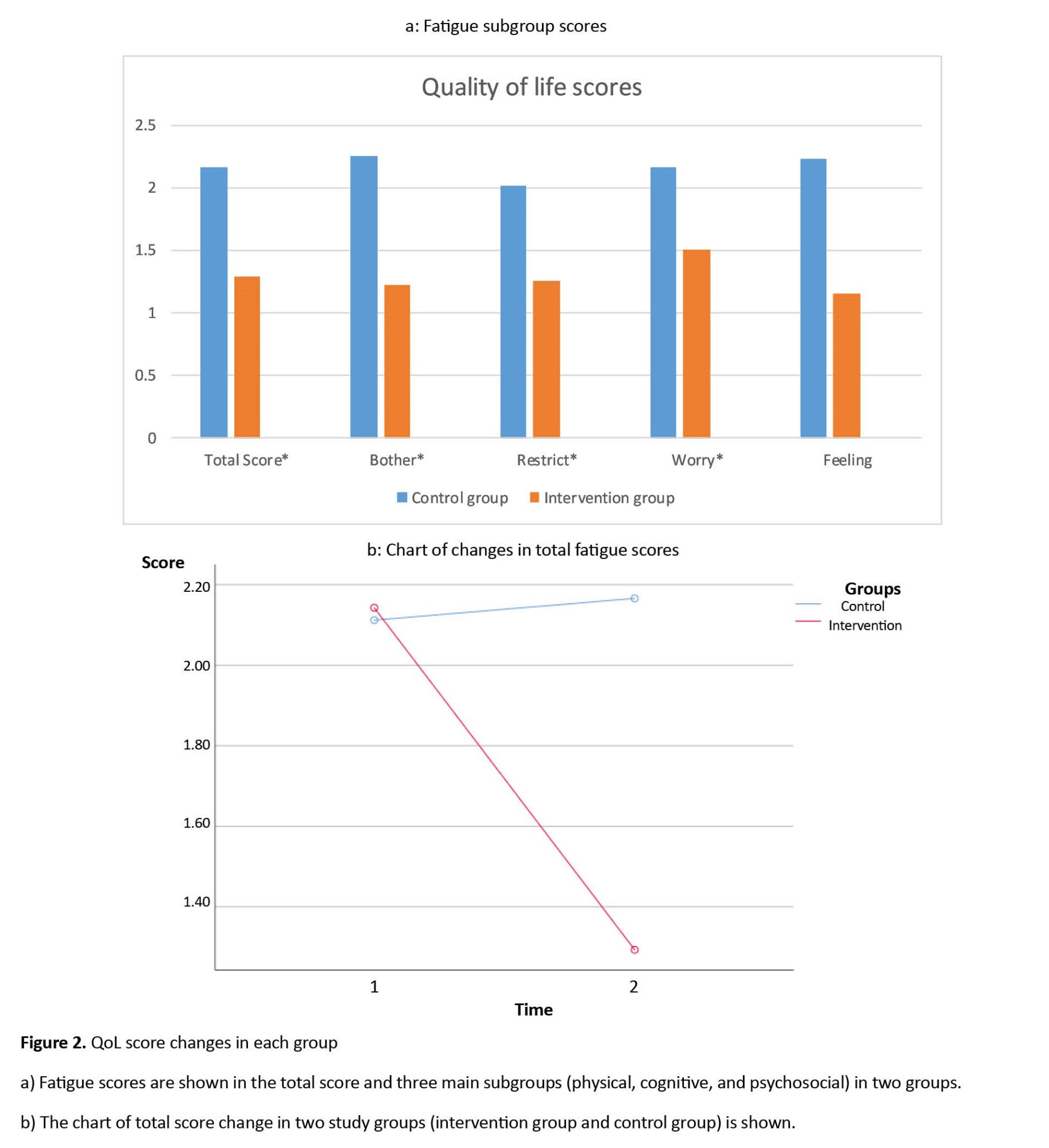
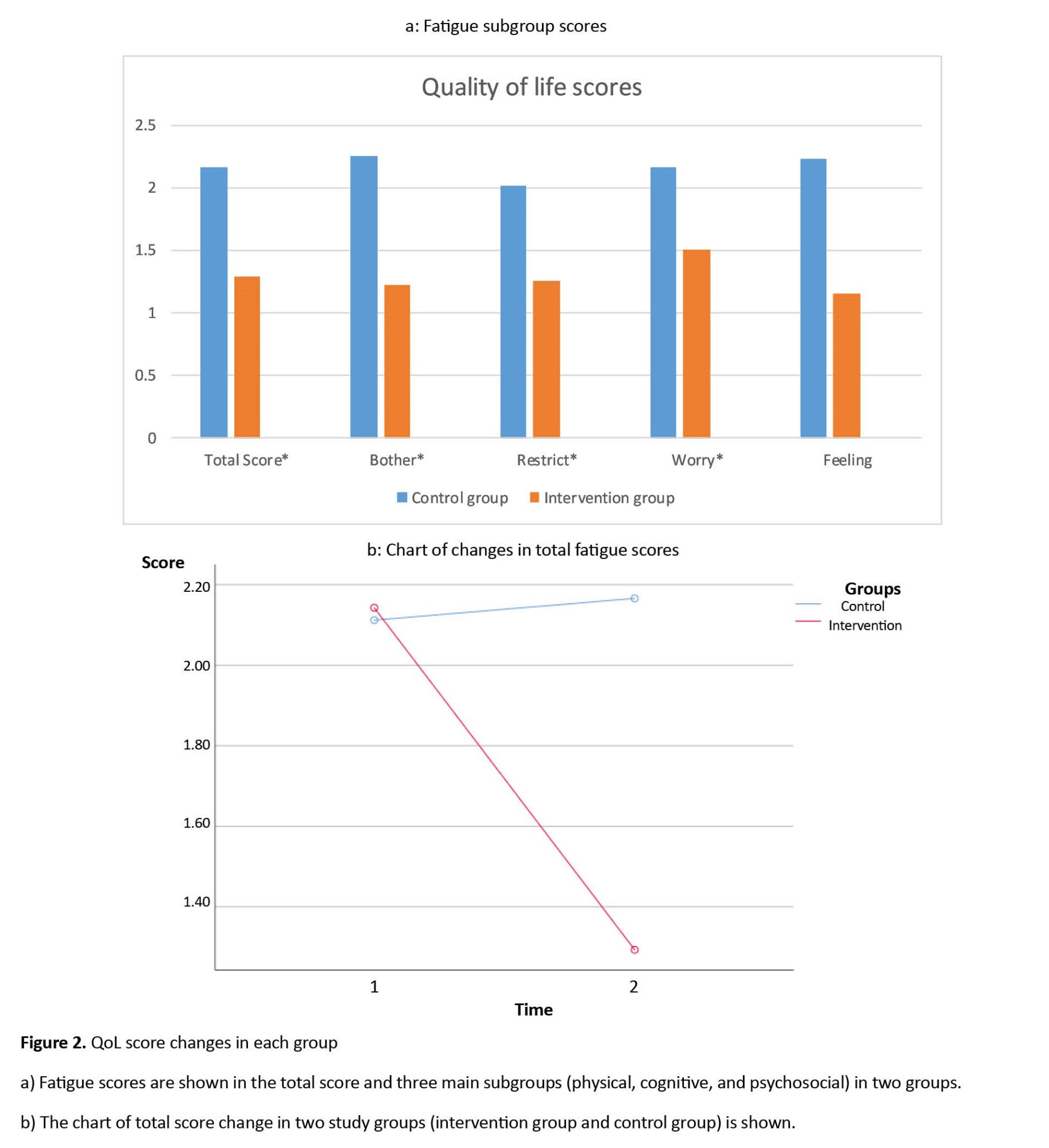
Table 3 presents the within-group results of QoL scores and subgroups related to them. After the study, in the intervention group, a significant difference is observed in the total QoL score and all its subgroups, except for the emotions subgroup (P<0.05). Table 3 presents the Mean±SD of each group and the P between the two groups. After the intervention, scores in the intervention group showed a significant decrease compared to the control group (P<0.05).
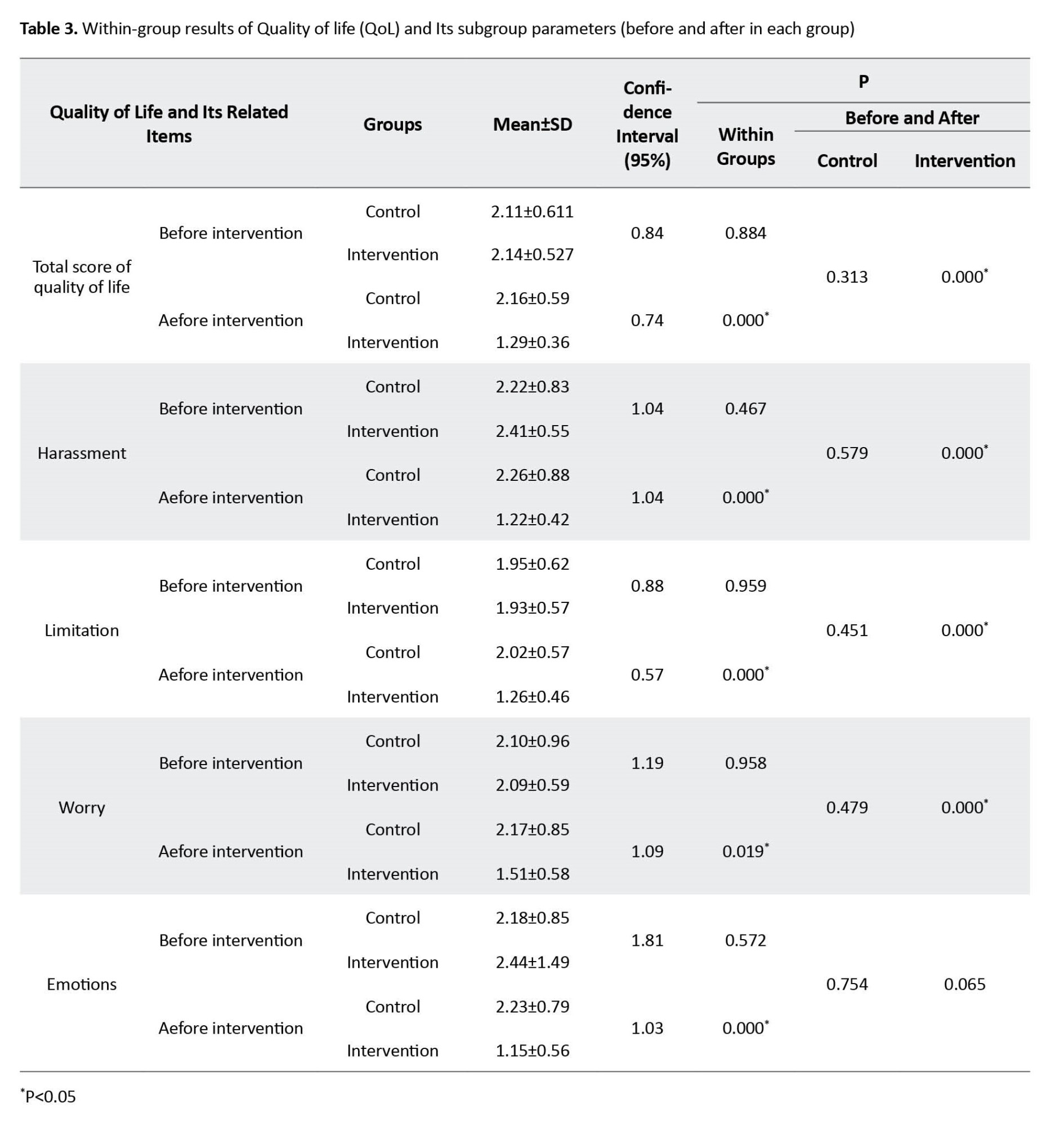
Figure 2 shows the mean scores of the QoL and related subgroups after the study. Also, Figure 2 shows the changes in the total score.
Discussion
This study was conducted to investigate the effect of specific pelvic floor exercises at home along with awareness of pelvic floor muscles on fatigue and QoL of women with urinary disorders caused by MS. In a within-group comparison, the intensity of fatigue (through the MFIS questionnaire) in the intervention group decreased after eight weeks compared to the first day. Also, all sub-groups of fatigue including cognitive, physical, and psycho-social improved. In the control group without specific pelvic floor exercises, the intensity of fatigue and all its subgroups did not improve. Also, the level of fatigue in the intervention group did not improve except in the cognitive and psychosocial subgroups compared to the control group (P=0.137). Although the change graph of the total fatigue score showed a significant difference in the intervention group after the study, this difference was not significant between the two groups.
Fatigue is caused by various factors, such as psychological factors, musculoskeletal factors, sleep disorders, and side effects of a series of drugs. It seems that specific pelvic floor therapeutic exercises at home indirectly reduced fatigue by affecting the pelvic floor muscles and improving urinary disorders. Psychological factors affecting fatigue include stress and anxiety caused by the smell of urine, feeling ashamed and lack of motivation for social work, and musculoskeletal factors affecting fatigue include physical efforts to reach the bathroom earlier. Doing social activities and the subsequent aggravation of muscle weakness, and the lack of proper sleep at night due to nocturnal enuresis can be mentioned as one of the factors of sleep disorders affecting fatigue. The fatigue questionnaire in this study had three subgroups, cognitive fatigue, physical fatigue, and psycho-social fatigue, which cognitive subgroup included ten questions out of 21 questions of the MFIS questionnaire (47% of the total fatigue questionnaire). It seems that since the cognitive sub-group included most of the questions in the questionnaire, the non-significant difference in cognitive fatigue between the two groups was effective on the total score of fatigue and caused the significant difference between the two groups in total fatigue score. Also, the small sample size and measuring the level of fatigue based on the questionnaire that was filled out by the participants can be mentioned as other reasons for this result. The results of Lin et al.’s study in 2019 confirmed the current study because it was shown in Sofia’s study that a close relationship was observed between the frequency of bladder and bowel symptoms and the level of fatigue in MS patients [1].
In the within-group comparison, the QoL (through the Qualiveen-30 questionnaire) and its related subgroups except for emotions (P=0.65) in the intervention group in the eighth week compared to the first week improved (P<0.05). In the control group, the QoL and none of its subgroups improved after eight weeks (P>0.05). Nevertheless, the comparison between the two groups showed that the QoL and all related subgroups improved in the intervention group compared to the control group (P<0.05). It seems that people with urinary disorders caused by MS gradually avoid the community due to the experience of urinary incontinence in public, the bad smell of urine, in addition to feeling embarrassed and decreasing self-confidence, and this social isolation can cause depression in them. Avoiding the community can force a person to quit his job, and this issue can aggravate a person's depression and ultimately cause a decrease in the person's motivation to continue the treatment and reduce the effectiveness of the treatment, which all these factors decrease the quality of people's lives [3-5, 27]. It seems that since the emotions of MS sufferers are dependent on their social functions and are significantly related to the social support of these people, the improvement of urinary symptoms alone cannot play a special role in changing the emotions of these people [28]. To manage feelings, such as shame, worthlessness, anxiety, and discomfort from social stigma and finally not hiding urinary problems, a suitable cultural background is needed in the society where the affected person lives and the support of the people around him.
Rafii et al. conducted a similar study. They taught pelvic floor exercises at home for 12 weeks. The training was in the form of pelvic floor muscle contraction for three seconds and five seconds rest with a repetition of 90-100 daily contractions. The exercises were first taught to the users in the position of lying on the back (supine) with knees together and slow breathing. Gradually, exercises were practiced in sitting and standing positions. The results after 12 weeks showed a significant increase in the QoL (Qualiveen-30) in the intervention group [16]. In the study of Lucio et al. in 2011, pelvic muscle strengthening exercises were performed for 12 weeks on 35 women with MS. The intervention in the group of 18 people included pelvic floor muscle exercises in arch position along with vaginal perineometer in addition to home exercises with a dosage of three times a day and without any external aids and in sitting and standing positions. The results showed a significant difference in Qualiveen-30 and ICIQ-SF questionnaires. Also, the results showed no significant difference in the improvement of the QoL between groups in the SF-36 questionnaire [29]. In many studies, the results showed improvement in the QoL of the participants after 12 weeks, while in the present study, a significant difference between the two groups was observed only after eight weeks of intervention. Also, in the present study, before starting therapeutic exercise, attention was paid to people’s awareness of pelvic floor muscles, and therapeutic exercises were performed as warm-up, pelvic floor strengthening exercises, and then cool down.
One of the limitations of the present study is the sample size. Also, the duration of the study intervention was limited compared to similar studies. It is suggested that in future studies, the study should be conducted with a larger sample size and a longer treatment period with a follow-up period without treatment after the intervention. It is also recommended to study for men. Since urinary infections are common in people with urinary incontinence, reducing urinary incontinence with the help of specific pelvic floor exercises seems to reduce urinary infections. Therefore, it is suggested to investigate the effect of therapeutic exercises on urinary infections through laboratory tests in future studies.
Conclusion
It seems that performing specific pelvic floor therapeutic exercises at home along with increasing awareness of pelvic floor muscles reduces fatigue and improves the QoL in women with urinary disorders caused by MS. Although specific pelvic floor exercises did not improve fatigue (except for the cognitive and psycho-social subgroups) in the treatment group compared to the control group, it seems that fatigue can be improved by controlling other intervening factors of fatigue as well as increasing the sample size and length of treatment.
Ethical Considerations
Compliance with ethical guidelines
The ethical code of the present study was IR.IUMS.REC.1398.1007, which was obtained from the Ethics Committee of Iran University of Medical Sciences. In addition, the objectives of the study were fully explained to the participants and then the written informed consent form was provided to the participants.
Funding
The article was extracted from MA thisis of first author at Department of Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences in Tehran.
Authors' contributions
Conceptualization and supervision: Shohreh Noorizadeh Dehkordi; Methodology: Zahra Ghafari and Seyedeh Roghayeh Mousavi Khatir; Writing–original draft: Zahra Ghafari; Investigation, writing–review & editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We thank all the participants for participating in this study, as well as the Iranian MS Association, Iran University of Medical Sciences, and all the physiotherapists and doctors who helped us in some way to complete the study
References
Multiple Sclerosis (MS) is the most common inflammatory disease of the central nervous system that causes urinary disorders in these people. Urinary problems are seen in more than 50% of MS patients [1]. Urinary disorders in MS patients in the form of increased daily urinary frequency, nocturia, stress urinary incontinence and urgency, enuresis, slow flow of urine, the spread of urine flow, interruption, delay, straining to urinate, final dripping, the sensation of incomplete emptying and dripping of urine occurs after urination [2]. Urinary disorders have a great impact on people’s quality of life (QoL) by reducing self-confidence, depression, anxiety, social isolation, leaving jobs, and reducing motivation. It can also reduce the quality of sleep after nocturnal enuresis and make the person tired the next day. Also, people who have urinary disorders usually reduce their water intake, and dehydration is another factor that can aggravate fatigue, and as we know, fatigue is one of the most debilitating symptoms of MS. Also, factors, such as leakage of urine, reduction of water consumption, and increased residual volume of urine can cause urinary infections, which can increase the probability of attack, and progression of the disease, hospitalization, and death of people with MS [3-9]. The goal of all therapeutic interventions to manage urinary problems is to improve the patients’ QoL in the first step and to prevent long-term damage to the bladder and urinary infections in the next step. Exercise therapy is the first line of treatment in people with urinary incontinence caused by MS. Studies have shown that 56% to 70% of MS patients improve urinary disorders by doing therapeutic exercises [10-13].
The effects of pelvic floor muscle exercises have been reviewed in several articles. Articles have shown that pelvic floor exercises can make positive changes in the strength of pelvic floor muscles [14], 24-hour pad test [15], number of nocturnal urination [15], number of pad use [14], defecation episodes of urine [14], and QoL [16]. In a systematic study, it was also stated that pelvic floor muscle exercises are more effective than other non-drug treatments for urinary disorders [17, 18]. In addition, studies were conducted that investigated the effect of postural balance exercises, functional mobility exercises, aerobic exercise at home, regular physical exercises, and water therapy on the fatigue of individuals with MS [19-21]. However, among the studies, the effect of pelvic floor exercise on the fatigue of patients with MS was not observed. Also, few studies mentioned the role of awareness of the pelvic floor before doing the exercises [22].
Therefore, this research was conducted to investigate the effect of specific pelvic floor exercises at home along with increasing awareness of pelvic floor muscles on the level of fatigue and QoL of women with urinary problems caused by MS. In this study, people were given exercises at home to partially control the effect of this confounding variable on fatigue.
Materials and Methods
The current study was a double-blind randomized clinical trial that was conducted in parallel with two control and intervention groups. The studied population was women with urinary disorders caused by MS in the age group of 18 to 50 years. The non-probability sampling method was used. In this study, after obtaining the consent form of the participants, people were divided into two groups based on the expanded disability status scale (EDSS) and the type of urinary disorder using a sealed envelope method. Referring to similar articles [23, 24], the sample size is equal to 30 people, with 15 people in each group.
After the initial evaluations, the patients voluntarily entered the study if they met the inclusion criteria. All participants completed the consent form to participate in the study. The inclusion criteria for the study included the following items, women with MS with relapses and remissions diagnosed by a neurologist, in the age range of 18-50 years, the measurement score of mental health based on mini-mental state examination (MMSE) questionnaire should be higher than 18, disability score based on EDSS questionnaire should be less than seven, urinary disorder based on 8-item Overactive Bladder (OAB-V8) questionnaire should be higher than eight, they should not have had an attack in the last three months and in the dosage of drugs, there have been no changes related to urinary disorders of people in the last three months. Also, the exclusion criteria of people included having an attack during the study, becoming pregnant during the study, and having a urinary infection.
The participants visited the clinic for a total of two sessions. In the first session, to know more about pelvic floor muscles, the anatomy and function of pelvic floor muscles were explained to each participant along with pictures. The prerequisite for doing exercises and contracting the pelvic floor muscles was to know about the pelvic floor muscles. In this study, for this purpose, we placed a rolled towel on the pelvic floor area of the participants while they were sitting on the edge of the bed. Then, we asked each participant to try to separate their seat from the towel by pulling up and gathering the pelvic floor. Then, after ensuring that the pelvic floor muscles were properly contracted, each participant lay down on the bed in an arched position, and tone management exercises, breathing exercises, stretching, and strengthening of the pelvic floor muscles were taught to each participant. In this session, participants were given a bladder diary form to fill it at home for three consecutive days, and based on the information on this form, urinary behavior counseling was given to them verbally and in writing in the second session. Based on this training, the pattern of proper nutrition and behavioral therapy of the participants was explained according to their urinary disorder. In the second session, the exercises were repeated for each participant.
The exercises were explained to each participant during the first and second sessions and the correctness of the exercises was repeated three or more times for each participant. The exercises included tone management exercises, diaphragmatic breathing, stretching of thigh adductor muscles, piriformis, and external rotators, and strengthening of pelvic floor muscles in different positions (from lower to the upper center of gravity). The order of exercises was done by the participants as warm-up, pelvic floor strengthening exercises, and then cooling down. Warm-up and cool-down exercises included tone management, stretching, and diaphragmatic breathing exercises. The exercises were done daily by the participants at home for eight weeks. Stretching exercises for 30 s and strengthening exercises with holding for 3 s and resting for 6 seconds and repeating two sets of 10 per day were prescribed. The therapist followed up the process of doing the exercises weekly (telephone call three times a week).
Data collection
First, the demographic information of the participants was recorded. Before the intervention, the participants completed Qualiveen-30 questionnaire and Modified Fatigue Impact Scale (MFIS). Qualiveen-30 evaluates the QoL affected by urinary disorders in people with spinal cord injury and MS. This questionnaire measures the QoL in four subgroups, harassment (including 9 questions), coercion or restriction (including 8 questions), worry (including 8 questions) and emotions (including 5 questions) and a higher score in this questionnaire indicates a person’s lower QoL. The validity and reliability of this questionnaire were conducted in Iran in 2015 [25]. The MFIS questionnaire is designed to measure the level of fatigue of people with MS in 21 questions, which examines the level of fatigue in three subgroups, physical, cognitive, and psychosocial. A higher score in this questionnaire indicates a higher level of fatigue in people. The validity and reliability of this questionnaire were conducted in Iran in 2013 [26], in this study, the bladder diary form was used only to provide counseling on urinary behavior. To complete the bladder diary form, the participant must complete the form carefully at home for three consecutive days, considering the type of urinary disorder. At the end of the study, participants filled out the MFIS and Qualiveen-30 forms again.
Results
This study was conducted in 2022. All participants completed the study. Table 1 shows the personal and clinical information of the study participants. The type of urinary disorder is shown in the table. Many participants expressed several disorders at the same time, therefore the table shows the number of participants who had each disorder.
Based on the results, all the data in both groups followed the normal distribution before and after the study. Therefore, in this study, a parametric t-test was used. In the comparison between groups, we used the independent sample t-test and the paired sample t-test for within-group comparison.
Fatigue
Table 2 presents the comparison results before and after the study. After the study, a significant difference was found in the total score and all variables related to fatigue in the intervention group (P<0.05).
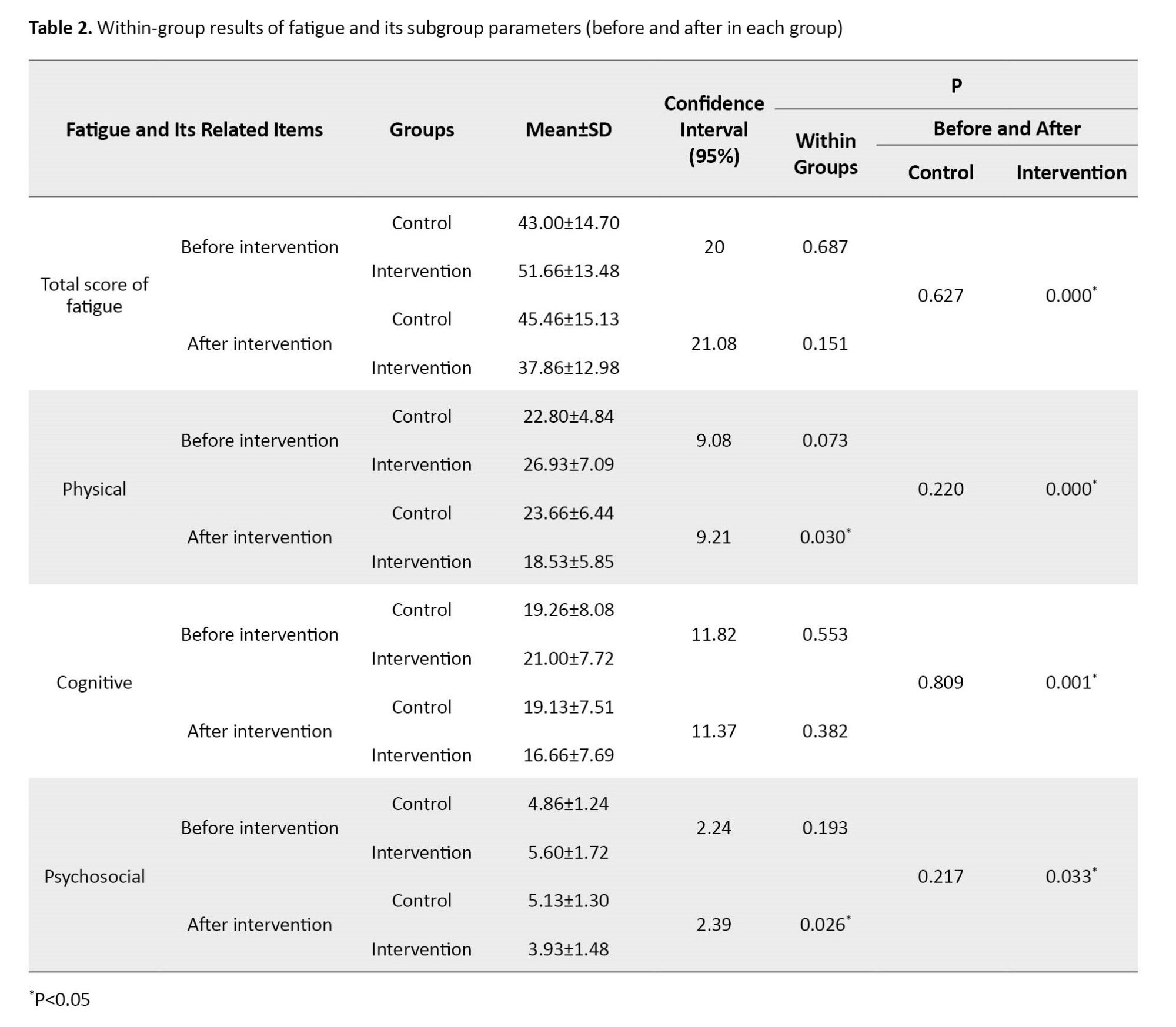
Also, the results showed that after the study, a significant difference was found in the physical and psychosocial subgroups between the two intervention and control groups (P<0.05). A graph shows the average scores of two groups after the study. Also, Figure 1 shows the total score changes.
QoL
Table 3 presents the within-group results of QoL scores and subgroups related to them. After the study, in the intervention group, a significant difference is observed in the total QoL score and all its subgroups, except for the emotions subgroup (P<0.05). Table 3 presents the Mean±SD of each group and the P between the two groups. After the intervention, scores in the intervention group showed a significant decrease compared to the control group (P<0.05).
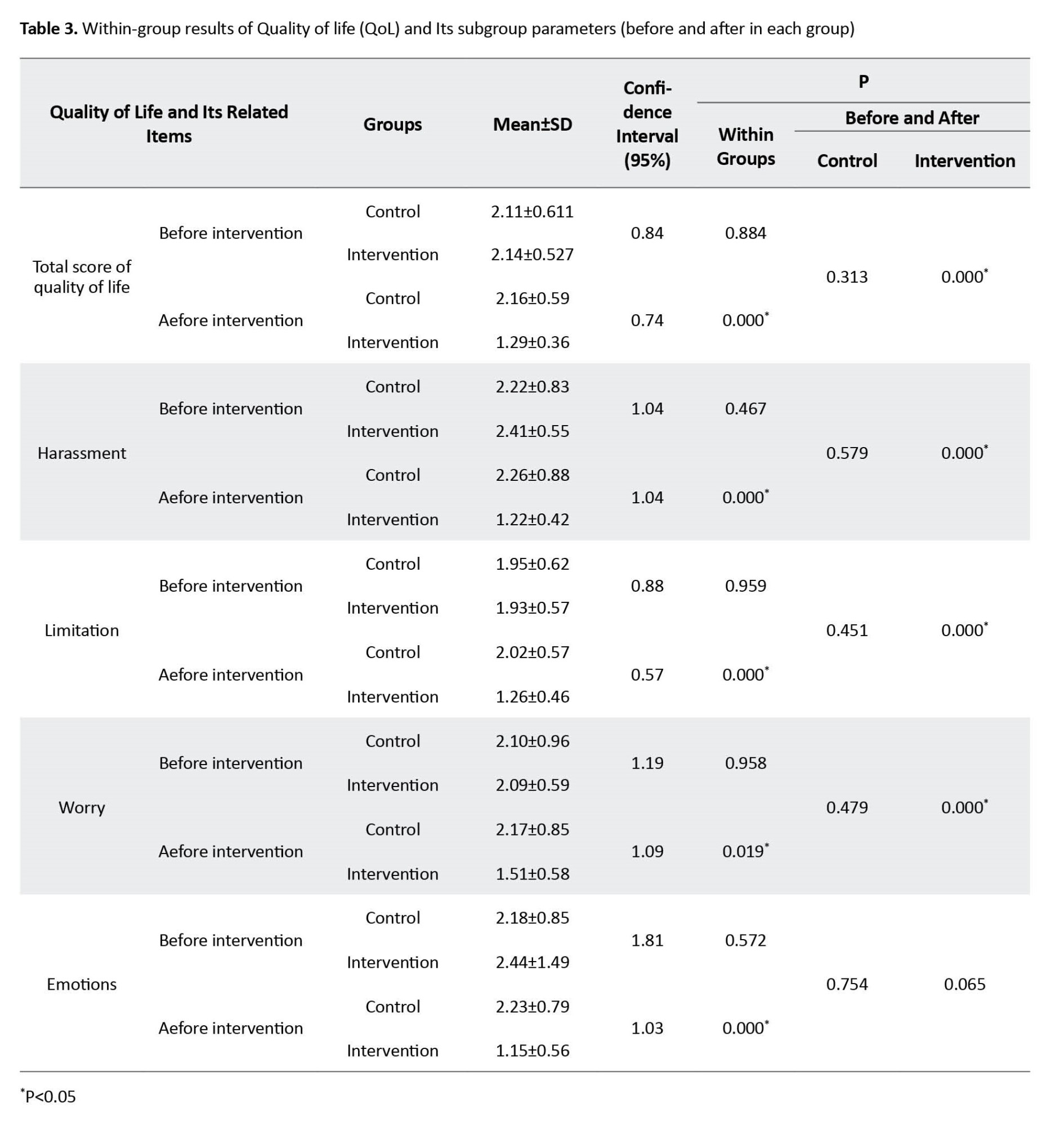
Figure 2 shows the mean scores of the QoL and related subgroups after the study. Also, Figure 2 shows the changes in the total score.
Discussion
This study was conducted to investigate the effect of specific pelvic floor exercises at home along with awareness of pelvic floor muscles on fatigue and QoL of women with urinary disorders caused by MS. In a within-group comparison, the intensity of fatigue (through the MFIS questionnaire) in the intervention group decreased after eight weeks compared to the first day. Also, all sub-groups of fatigue including cognitive, physical, and psycho-social improved. In the control group without specific pelvic floor exercises, the intensity of fatigue and all its subgroups did not improve. Also, the level of fatigue in the intervention group did not improve except in the cognitive and psychosocial subgroups compared to the control group (P=0.137). Although the change graph of the total fatigue score showed a significant difference in the intervention group after the study, this difference was not significant between the two groups.
Fatigue is caused by various factors, such as psychological factors, musculoskeletal factors, sleep disorders, and side effects of a series of drugs. It seems that specific pelvic floor therapeutic exercises at home indirectly reduced fatigue by affecting the pelvic floor muscles and improving urinary disorders. Psychological factors affecting fatigue include stress and anxiety caused by the smell of urine, feeling ashamed and lack of motivation for social work, and musculoskeletal factors affecting fatigue include physical efforts to reach the bathroom earlier. Doing social activities and the subsequent aggravation of muscle weakness, and the lack of proper sleep at night due to nocturnal enuresis can be mentioned as one of the factors of sleep disorders affecting fatigue. The fatigue questionnaire in this study had three subgroups, cognitive fatigue, physical fatigue, and psycho-social fatigue, which cognitive subgroup included ten questions out of 21 questions of the MFIS questionnaire (47% of the total fatigue questionnaire). It seems that since the cognitive sub-group included most of the questions in the questionnaire, the non-significant difference in cognitive fatigue between the two groups was effective on the total score of fatigue and caused the significant difference between the two groups in total fatigue score. Also, the small sample size and measuring the level of fatigue based on the questionnaire that was filled out by the participants can be mentioned as other reasons for this result. The results of Lin et al.’s study in 2019 confirmed the current study because it was shown in Sofia’s study that a close relationship was observed between the frequency of bladder and bowel symptoms and the level of fatigue in MS patients [1].
In the within-group comparison, the QoL (through the Qualiveen-30 questionnaire) and its related subgroups except for emotions (P=0.65) in the intervention group in the eighth week compared to the first week improved (P<0.05). In the control group, the QoL and none of its subgroups improved after eight weeks (P>0.05). Nevertheless, the comparison between the two groups showed that the QoL and all related subgroups improved in the intervention group compared to the control group (P<0.05). It seems that people with urinary disorders caused by MS gradually avoid the community due to the experience of urinary incontinence in public, the bad smell of urine, in addition to feeling embarrassed and decreasing self-confidence, and this social isolation can cause depression in them. Avoiding the community can force a person to quit his job, and this issue can aggravate a person's depression and ultimately cause a decrease in the person's motivation to continue the treatment and reduce the effectiveness of the treatment, which all these factors decrease the quality of people's lives [3-5, 27]. It seems that since the emotions of MS sufferers are dependent on their social functions and are significantly related to the social support of these people, the improvement of urinary symptoms alone cannot play a special role in changing the emotions of these people [28]. To manage feelings, such as shame, worthlessness, anxiety, and discomfort from social stigma and finally not hiding urinary problems, a suitable cultural background is needed in the society where the affected person lives and the support of the people around him.
Rafii et al. conducted a similar study. They taught pelvic floor exercises at home for 12 weeks. The training was in the form of pelvic floor muscle contraction for three seconds and five seconds rest with a repetition of 90-100 daily contractions. The exercises were first taught to the users in the position of lying on the back (supine) with knees together and slow breathing. Gradually, exercises were practiced in sitting and standing positions. The results after 12 weeks showed a significant increase in the QoL (Qualiveen-30) in the intervention group [16]. In the study of Lucio et al. in 2011, pelvic muscle strengthening exercises were performed for 12 weeks on 35 women with MS. The intervention in the group of 18 people included pelvic floor muscle exercises in arch position along with vaginal perineometer in addition to home exercises with a dosage of three times a day and without any external aids and in sitting and standing positions. The results showed a significant difference in Qualiveen-30 and ICIQ-SF questionnaires. Also, the results showed no significant difference in the improvement of the QoL between groups in the SF-36 questionnaire [29]. In many studies, the results showed improvement in the QoL of the participants after 12 weeks, while in the present study, a significant difference between the two groups was observed only after eight weeks of intervention. Also, in the present study, before starting therapeutic exercise, attention was paid to people’s awareness of pelvic floor muscles, and therapeutic exercises were performed as warm-up, pelvic floor strengthening exercises, and then cool down.
One of the limitations of the present study is the sample size. Also, the duration of the study intervention was limited compared to similar studies. It is suggested that in future studies, the study should be conducted with a larger sample size and a longer treatment period with a follow-up period without treatment after the intervention. It is also recommended to study for men. Since urinary infections are common in people with urinary incontinence, reducing urinary incontinence with the help of specific pelvic floor exercises seems to reduce urinary infections. Therefore, it is suggested to investigate the effect of therapeutic exercises on urinary infections through laboratory tests in future studies.
Conclusion
It seems that performing specific pelvic floor therapeutic exercises at home along with increasing awareness of pelvic floor muscles reduces fatigue and improves the QoL in women with urinary disorders caused by MS. Although specific pelvic floor exercises did not improve fatigue (except for the cognitive and psycho-social subgroups) in the treatment group compared to the control group, it seems that fatigue can be improved by controlling other intervening factors of fatigue as well as increasing the sample size and length of treatment.
Ethical Considerations
Compliance with ethical guidelines
The ethical code of the present study was IR.IUMS.REC.1398.1007, which was obtained from the Ethics Committee of Iran University of Medical Sciences. In addition, the objectives of the study were fully explained to the participants and then the written informed consent form was provided to the participants.
Funding
The article was extracted from MA thisis of first author at Department of Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences in Tehran.
Authors' contributions
Conceptualization and supervision: Shohreh Noorizadeh Dehkordi; Methodology: Zahra Ghafari and Seyedeh Roghayeh Mousavi Khatir; Writing–original draft: Zahra Ghafari; Investigation, writing–review & editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We thank all the participants for participating in this study, as well as the Iranian MS Association, Iran University of Medical Sciences, and all the physiotherapists and doctors who helped us in some way to complete the study
References
- Lin SD, Butler JE, Boswell-Ruys CL, Hoang P, Jarvis T, Gandevia SC, et al. The frequency of bowel and bladder problems in multiple sclerosis and its relation to fatigue: A single centre experience. PLoS One. 2019; 14(9):e0222731. [DOI:10.1371/journal.pone.0222731] [PMID] [PMCID]
- Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. 2003; 61(1):37-49. [DOI:10.1016/S0090-4295(02)02243-4] [PMID]
- Wendebourg MJ, Heesen C, Finlayson M, Meyer B, Pöttgen J, Köpke S. Patient education for people with multiple sclerosis-associated fatigue: A systematic review. PLoS One. 2017; 12(3):e0173025. [DOI:10.1371/journal.pone.0173025] [PMID] [PMCID]
- Nortvedt MW, Riise T, Myhr KM, Landtblom AM, Bakke A, Nyland HI. Reduced quality of life among multiple sclerosis patients with sexual disturbance and bladder dysfunction. Mult Scler. 2001; 7(4):231-5. [DOI:10.1177/135245850100700404] [PMID]
- de Sèze M, Ruffion A, Denys P, Joseph PA, Perrouin-Verbe B, GENULF. The neurogenic bladder in multiple sclerosis: review of the literature and proposal of management guidelines. Mult Scler. 2007; 13(7):915-28. [DOI:10.1177/1352458506075651] [PMID]
- Cincotta MC, Engelhard MM, Stankey M, Goldman MD. Fatigue and fluid hydration status in multiple sclerosis: A hypothesis. Mult Scler. 2016; 22(11):1438-43. [DOI:10.1177/1352458516663854] [PMID] [PMCID]
- Ruiz-Rizzo AL, Bublak P, Kluckow S, Finke K, Gaser C, Schwab M, et al. Neural distinctiveness of fatigue and low sleep quality in multiple sclerosis. Eur J Neurol. 2022; 29(10):3017-27. [DOI:10.1111/ene.15445] [PMID]
- Minardi D, d'Anzeo G, Parri G, Polito M Jr, Piergallina M, El Asmar Z, et al. The role of uroflowmetry biofeedback and biofeedback training of the pelvic floor muscles in the treatment of recurrent urinary tract infections in women with dysfunctional voiding: A randomized controlled prospective study. Urology. 2010; 75(6):1299-304. [DOI:10.1016/j.urology.2009.11.019] [PMID]
- Hansson Vikström N, Wasteson E, Lindam A, Samuelsson E. Anxiety and depression in women with urinary incontinence using E-health. Int Urogynecol J. 2021; 32(1):103-9. [DOI:10.1007/s00192-020-04227-2] [PMID] [PMCID]
- Deeba E, Koptides D, Lambrianides A, Pantzaris M, Krashias G, Christodoulou C. Complete sequence analysis of human toll-like receptor 3 gene in natural killer cells of multiple sclerosis patients. Mult Scler Relat Disord. 2019; 33:100-6. [DOI:10.1016/j.msard.2019.05.027] [PMID]
- Wilson PD. Conservative treatment in women. In: Incontinence: 2nd international consultation. Plymouth: Health Publications; 2002. [Link]
- Heine M, van de Port I, Rietberg MB, van Wegen EE, Kwakkel G. Exercise therapy for fatigue in multiple sclerosis. Cochrane database of systematic reviews. 2015; (9):CD009956. [DOI:10.1002/14651858.CD009956.pub2] [PMID] [PMCID]
- Pérez DC, Chao CW, Jiménez LL, Fernández IM, De la Llave Rincon AI. Pelvic floor muscle training adapted for urinary incontinence in multiple sclerosis: A randomized clinical trial. Int Urogynecol J. 2020; 31(2):267-75. [DOI:10.1007/s00192-019-03993-y] [PMID]
- Pereira CMA, Castiglione M, Kasawara KT. Effects of physiotherapy treatment for urinary incontinence in patient with multiple sclerosis. J Phys Ther Sci. 2017; 29(7):1259-63. [DOI:10.1589/jpts.28.1259] [PMID] [PMCID]
- Lucio AC, Campos RM, Perissinotto MC, Miyaoka R, Damasceno BP, D’Ancona CA. Pelvic floor muscle training in the treatment of lower urinary tract dysfunction in women with multiple sclerosis. Neurourol Urodyn. 2010; 29(8):1410-3. [DOI:10.1002/nau.20941] [PMID]
- Rafii F, Sajjadi M, Shareinia H, Sarraf P, Seyedalshohahadaee M. Effects of pelvic floor muscle exercises on urinary incontinence and quality of life in patients with multiple sclerosis. World Fam Med. 2018; 16(1):62-69. [DOI:10.5742/MEWFM.2018.93199] [Link]
- Bø K, Talseth T, Holme I. Single blind, randomised controlled trial of pelvic floor exercises, electrical stimulation, vaginal cones, and no treatment in management of genuine stress incontinence in women. BMJ. 1999; 318(7182):487-93. [DOI:10.1136/bmj.318.7182.487] [PMID] [PMCID]
- Henalla SM, Hutchins CJ, Robinson P, Macvicar J. Non-operative methods in the treatment of female genuine stress incontinence of urine. J Obstet Gynaecol. 1989; 9(3):222-5. [DOI:10.3109/01443618909151046]
- Razazian N, Kazeminia M, Moayedi H, Daneshkhah A, Shohaimi S, Mohammadi M, et al. The impact of physical exercise on the fatigue symptoms in patients with multiple sclerosis: A systematic review and meta-analysis. BMC Neurol. 2020; 20(1):93. [DOI:10.1186/s12883-020-01654-y] [PMID] [PMCID]
- Moraes AG, Neri SGR, Motl RW, Tauil CB, von Glehn F, Corrêa ÉC, et al. Effects of hippotherapy on postural balance, functional mobility, self-perceived fatigue, and quality of life in people with relapsing-remitting multiple sclerosis: Secondary results of an exploratory clinical trial. Mult Scler Relat Disord. 2021; 52:102948. [DOI:10.1016/j.msard.2021.102948] [PMID]
- Kargarfard M, Shariat A, Ingle L, Cleland JA, Kargarfard M. Randomized Controlled trial to examine the impact of aquatic exercise training on functional capacity, balance, and perceptions of fatigue in female patients with multiple sclerosis. Arch Phys Med Rehabil. 2018; 99(2):234-41. [DOI:10.1016/j.apmr.2017.06.015] [PMID]
- Rafii F, Shareinia H, Seyedalshohahadaee M, Sarraf P, Mahmoodi F. The effect of pelvic floor muscle exercise training on urinary incontinence in patients with multiple sclerosis. Iran J Nurs. 2014; 27(87):43-54. [DOI:10.29252/ijn.27.87.43]
- Lúcio A, Dʼancona CA, Perissinotto MC, McLean L, Damasceno BP, de Moraes Lopes MH. Pelvic floor muscle training with and without electrical stimulation in the treatment of lower urinary tract symptoms in women with multiple sclerosis. J Wound Ostomy Continence Nurs. 2016; 43(4):414-9. [DOI:10.1097/WON.0000000000000223] [PMID]
- McClurg D, Ashe R, Marshall K, Lowe‐Strong A. Comparison of pelvic floor muscle training, electromyography biofeedback, and neuromuscular electrical stimulation for bladder dysfunction in people with multiple sclerosis: A randomized pilot study. Neurourol Urodyn. 2006; 25(4):337-48. [DOI:10.1002/nau.20209] [PMID]
- Nikfallah A, Rezaali S, Mohammadi N, Abrishamkar M, Rezaei E, Sahraian MA, et al. Translation, cultural adaptation and validation of the qualiveen-30 questionnaire in persian for patients with spinal cord injury and multiple sclerosis. Low Urin Tract Symptoms. 2015; 7(1):42-9. [DOI:10.1111/luts.12051] [PMID]
- Ghajarzadeh M, Jalilian R, Eskandari G, Ali Sahraian M, Reza Azimi A. Validity and reliability of Persian version of Modified Fatigue Impact Scale (MFIS) questionnaire in Iranian patients with multiple sclerosis. Disabil Rehabil. 2013; 35(18):1509-12. [DOI:10.3109/09638288.2012.742575] [PMID]
- Rosiak K, Zagożdżon P. Quality of life and social support in patients with multiple sclerosis. Psychiatr Pol. 2017; 51(5):923-35. [DOI:10.12740/PP/64709] [PMID]
- Radlak B, Cooper C, Summers F, Phillips LH. Multiple sclerosis, emotion perception and social functioning. J Neuropsychol. 2021; 15(3):500-15. [DOI:10.1111/jnp.12237] [PMID]
- Lúcio AC, Perissinoto MC, Natalin RA, Prudente A, Damasceno BP, D'ancona CA. A comparative study of pelvic floor muscle training in women with multiple sclerosis: Its impact on lower urinary tract symptoms and quality of life. Clinics (Sao Paulo). 2011; 66(9):1563-8. [DOI:10.1590/S1807-59322011000900010] [PMID] [PMCID]
Type of Study: Research |
Subject:
Physiotherapy
Received: 2023/03/8 | Accepted: 2023/04/17 | Published: 2022/12/29
Received: 2023/03/8 | Accepted: 2023/04/17 | Published: 2022/12/29





