Volume 6, Issue 1 (Continuously Updated 2023)
Func Disabil J 2023, 6(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Saadatmand M I, Amiri A, Salehi R, Yeganeh A, Mansour Souhani S. Responsiveness of the Persian Version of Forgotten Joint Score-12 Questionnaire After Lower Limb Surgery. Func Disabil J 2023; 6 (1) : 246.1
URL: http://fdj.iums.ac.ir/article-1-208-en.html
URL: http://fdj.iums.ac.ir/article-1-208-en.html
1- Department of Physiotherapy, Rehabilitation Research Center, Iranian Center of Excellence in Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedic Surgery, Rasoul-e-Akram Hospital, Iran University of Medical Sciences, Tehran, Iran.
3- Department of Physiotherapy, Rehabilitation Research Center, Iranian Center of Excellence in Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran. ,monireh.saadat93@gmail.com
2- Department of Orthopedic Surgery, Rasoul-e-Akram Hospital, Iran University of Medical Sciences, Tehran, Iran.
3- Department of Physiotherapy, Rehabilitation Research Center, Iranian Center of Excellence in Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran. ,
Keywords: Responsiveness, FJS-12, Total hip and knee arthroplasty, ACL reconstruction, Physiotherapy
Full-Text [PDF 998 kb]
(520 Downloads)
| Abstract (HTML) (1541 Views)
References
Full-Text: (650 Views)
Introduction
Total hip and knee arthroplasty are widely used for treating degenerative diseases of the hip and knee joints. According to statistics, 1 million total hip arthroplasty (THA) and total knee arthroplasty (TKA) are performed annually in the US. It is predicted to reach 3.5 million cases annually in 2030 [1]. The anterior cruciate ligament (ACL) reconstruction surgery is one of the standard treatments in the US; annually out of 200 000 ACL injuries, half of them lead to reconstruction [2]. These operations have various complications, including bone cement implantation syndrome, fracture during operation, residual pain, damage to muscular structures and ligaments, and dislocation. These complications affect the surgical outcome, quality of life, and joint function [3].
Joint awareness simply refers to any unwanted perception of a joint. These perceptions include strong sensations, such as pain, or weak sensations, such as mild stiffness, mental dysfunction, and any discomfort. Joint awareness is a negative concept, since healthy joints do not cause awareness in daily life, and are essentially forgotten [4]. Reaching a lack of joint awareness, similar to a healthy joint, is regarded as a post-surgical evaluation test. The ultimate goal is to achieve the stage of forgetting joint following total hip and TKA surgeries as well as ACL reconstruction, in addition to restoring the normal function and sensation of joints to a healthy joint state. This is an aim that is difficult to achieve and requires precise measurement [5].
Clinical instruments to evaluate disorders may not be able to specify the effect of musculoskeletal pains in all aspects of the person’s life. The constraints of clinical tools and identification of the need to engage the patient’s view in examining the treatment outcome led to the development and validation of PROM tools to evaluate the person’s activity and participation [6, 7, 8].
Regardless of the type of instrument and scale, an effective assessment of a scale should have three features, validity, reliability, and responsiveness: the scale should be able to find crucial clinical changes [9]. In clinical practice, a tool with good responsiveness should be able to detect changes in the effects of two treatments with different qualities [10]. Responsiveness has two aspects, internal and external responsiveness. The internal means the ability of the tool to identify changes along a specific time interval. External responsiveness refers to the comparison of the changes in a scale with similar changes in a reference scale [11]. The internal responsiveness is calculated through two methods, effect size, and standard response mean. The common method to evaluate external responsiveness is the receiving operator characteristic (ROC) curve [12]. Typically, the responsiveness of minimal clinically important change (MCIC) means the minimum extent of change in the score which is significant by the patient. Knowing MCIC helps the therapist and researchers to understand whether the treatment has progressed towards improvement [10, 13].
The forgotten joint score-12 (FJS-12) questionnaire is a patient-oriented tool developed in two separate versions in 2012 to measure the outcomes in patients under conservative and operative treatments in the knee and hip regions. This questionnaire measures the extent of joint awareness and the ability of patients to forget the involved leg during daily activities. It indicates the extent of acceptance of the new joint as a normal part of the body in the knee and hip regions during various daily activities [5]. The Persian version of FJS-12 is a reliable and valid tool for those seeking to undergo ACL reconstruction as well as THA [1, 14]. However, currently, the responsiveness of the Persian version of this questionnaire has not been examined so far. Accordingly, the responsiveness of the FJS-12 questionnaire has been evaluated by obtaining the MCIC as a patient-oriented tool to properly identify changes in the health status of patients before and after THA and TKA as well as ACL reconstruction.
Materials and Methods
From May 2022 to November 2022, 112 candidates for THA and TKA as well as ACL reconstruction referred to the orthopedic clinics of, Rasoul-e-Akram and Moheb Mehr hospitals as well as the Nava orthopedic clinic. The diagnosis of the candidate of each surgery was performed by an orthopedic specialist based on radiographic and magnetic resonance imaging (MRI) images [15, 16]. The inclusion criteria included patients above 18 years of age, with a literacy of high school and above, as well as Persian official language. The exclusion criteria included those who did not answer more than 8 items of the questionnaire, unwillingness to continue participation in the research, and failure to complete the postoperative physiotherapy sessions. The participants filled out the form of written informed consent before participating in the research.
Forgotten joint score-12 (FJS-12)
This questionnaire was translated in 2021 by Sohani et al., and its reliability and validity were examined among patients after ACL reconstruction [14]. This questionnaire was first designed in English for patients with arthritis of hip and knee joints who have undergone joint replacement surgery. This questionnaire includes 12 items measuring the extent of awareness about the joint along various daily activities. The score is obtained between 0-100. The highest possible score indicates the minimum extent of awareness of the operated joint; if more than four responses are lost, the total score cannot be calculable [5].
Western Ontario and McMaster Universities osteoarthritis index (WOMAC)
The patient-oriented questionnaire is the most widely used outcome measure in patients with lower limb arthritis, designed by Bellamy and Buchanan in 1988. It includes 33 items, covering four dimensions, symptoms (5 items), stiffness (2 items), pain (9 items), and daily life functioning (17 items). There are five options for each item, with the best response recorded as ‘never or none’, while the worst response is recorded as ‘very severe or always’. Here, higher scores represent a better status and less pain. The Persian version of this questionnaire has been translated and validated for use in Iran for patients with knee osteoarthritis. Acceptable evidence shows the reliability, validity, and responsiveness of this questionnaire [17].
Method
The present research is an interventional (quasi-experimental) method, while also belonging to methodological studies of diagnostic tests. First, the subjects received and completed WOMAC, FJS-12, and visual analogue scale (VAS) questionnaires one week before surgery. Next, after 8 weeks before surgery and completing the full course of physiotherapy three sessions per week, they completed the previous questionnaires plus the global rating of change (GRC). The GRC is a seven-score criterion, which asks questions about the extent of improvement post-treatment [18]. In this study, the physiotherapy treatment has not been studied as a control, since the focus of this study has been on the responsiveness of a measurement tool, and does not emphasize the effectiveness of the treatment method [9, 19]. Nevertheless, the physiotherapy treatment has been performed according to physiotherapy guidelines following THA and TKA as well as ACL reconstruction, including improvements in the range of motion of the involved joint, increase in the muscle strength and endurance, as well as attempts for full loading on the involved joint.
Statistical analysis
All data were introduced into SPSS software, version 26 and Microsoft Excel, version 2016. The significance level was considered P<0.05. The mean and standard deviation of the continuous quantitative and ranked qualitative variables were measured. Also, the Kolmogorov-Smirnov test was used to examine the normality of data distribution. Based on the GRC criterion, the subjects were divided into two groups, improved (I have improved very much and I have improved much), and unimproved (I have improved slightly, I have not changed, I have got worse slightly, I have got worse much, and I have got worse very much) [12].
Changes in the pre-surgery and post-treatment scores were measured for each criterion. Positive score changes indicate improvement, while negative score changes indicate deterioration [20]. The statistical method of external responsiveness is especially interesting for researchers who focus on responsiveness [11, 20]. The responsiveness in this study is measured using two methods of ROC and correlation between the pre- and post-score changes with the GRC score.
ROC analysis measures the differentiation between the improved and unimproved groups resulting from the GRC criterion based on sensitivity and specificity. Sensitivity means finding a clinical change when it exists, while specificity means the ability to find no clinical change when a change is present [10, 12]. The cut-off point has been calculated through several changes in the sensitivity and specificity scores. The sensitivity is drawn on the vertical axis (Y), while specificity-1 is drawn on the horizontal axis (X) for all cutoff points. The area under the curve (AUC) offers some information about the ability of the instrument to identify the improved and unimproved subjects [21, 22]. The accuracy of the AUC based on academic scoring is as follows: 0.90-1.00=excellent, 0.80-0.89=good, 0.70-0.79=average, 0.60-0.69=poor, and 0.00-0.59=fail. An AUC score above 0.70 means suitable responsiveness [23, 24]. The cutoff point close to the top left corner of the AUC is extracted as the highest sensitivity and specificity as the MCIC [25]. MCIC in this study shows whether a proper change in FJS-12 scores has occurred for changes in joint awareness.
The Gamma correlation coefficient has been calculated to measure the relationship between the GRC ranked data and changes in pre/post-treatment scores. A positive score difference is expected to indicate a high improvement score in GRC. Correlation coefficients <0.25, 0.25-0.50, 0.50-0.75, and >0.75 represent no or trivial relationship, weak relationship, average to good relationship, and good to excellent relationship, respectively. A score close to 1 shows that the mentioned instrument can measure changes in health status by GRC [13, 26].
Results
In this study, 25 subjects (22%) with ACL reconstruction, 33 subjects (30%) with THA, and 54 subjects with TKA (48%) participated, respectively. Table 1 presents the demographic characteristics of the subjects plus the clinical data.
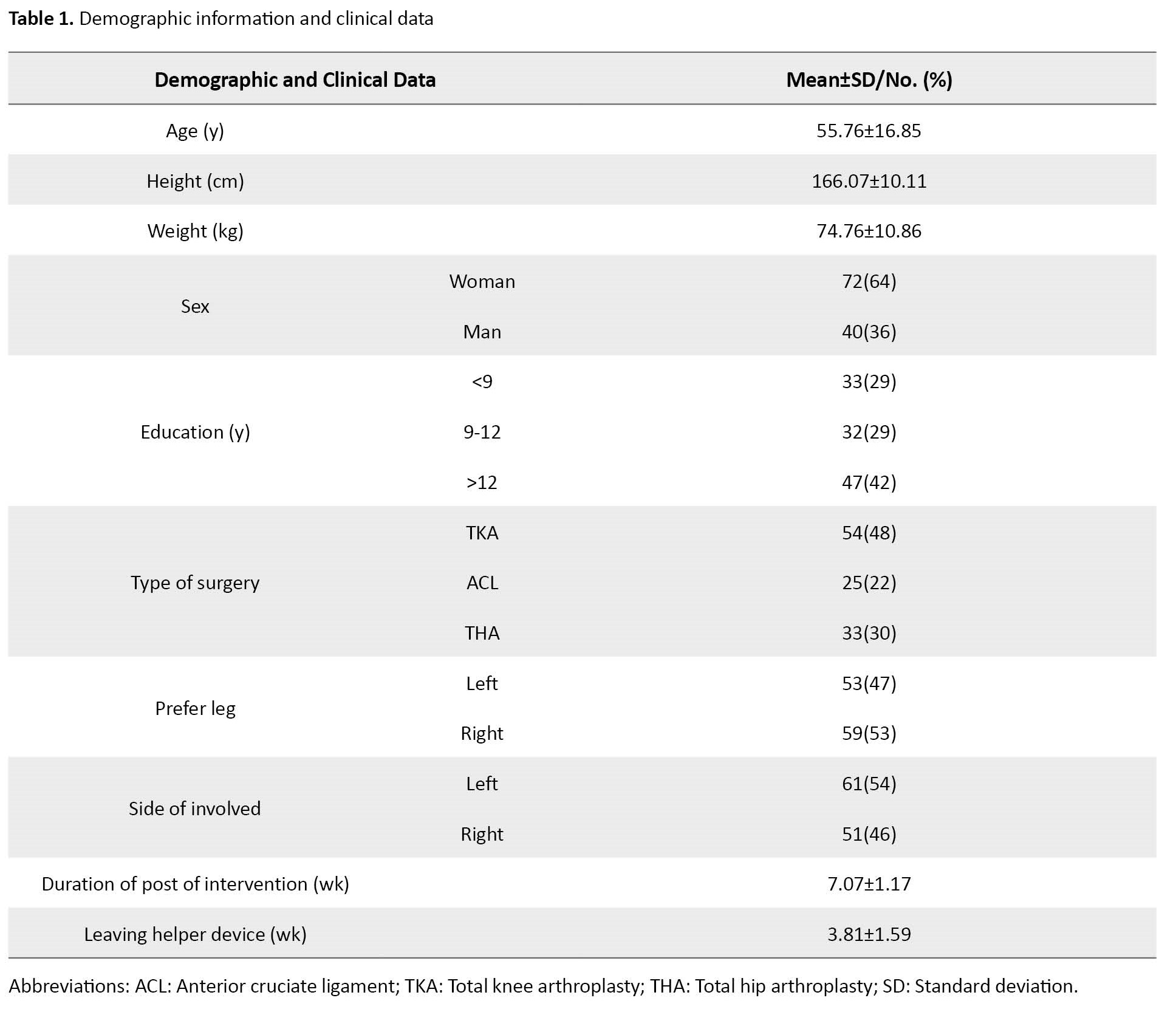
Table 2 presents descriptive statistics, including Means±SD of each questionnaire pre- and post-treatment.

According to GRC classification, 20 subjects chose ‘I have improved very much’ (18%), 36 subjects chose ‘I have improved much’ (32%), 42 subjects chose ‘I have improved slightly’ (38%), 9 subjects chose ‘I have not changed’ (8%), 3 subjects chose ‘I have worsened’ (3%), and 2 subjects chose ‘I have worsened very much’ (2%). Thus, 56 subjects fell in the improved group (50%) and 56 subjects in the unimproved group (50%).
In this study, the AUC of each questionnaire has been calculated with a confidence interval (CI) of 95%. Their AUC for FJS-12, WOMAC, and VAS has been (0.778, 0.693-0.863), (0.779, 0.695-0.863), and (0.851, 0.782-0.921). Table 3 presents the desired cutoff points of each questionnaire as well as the specificity and sensitivity of each point.
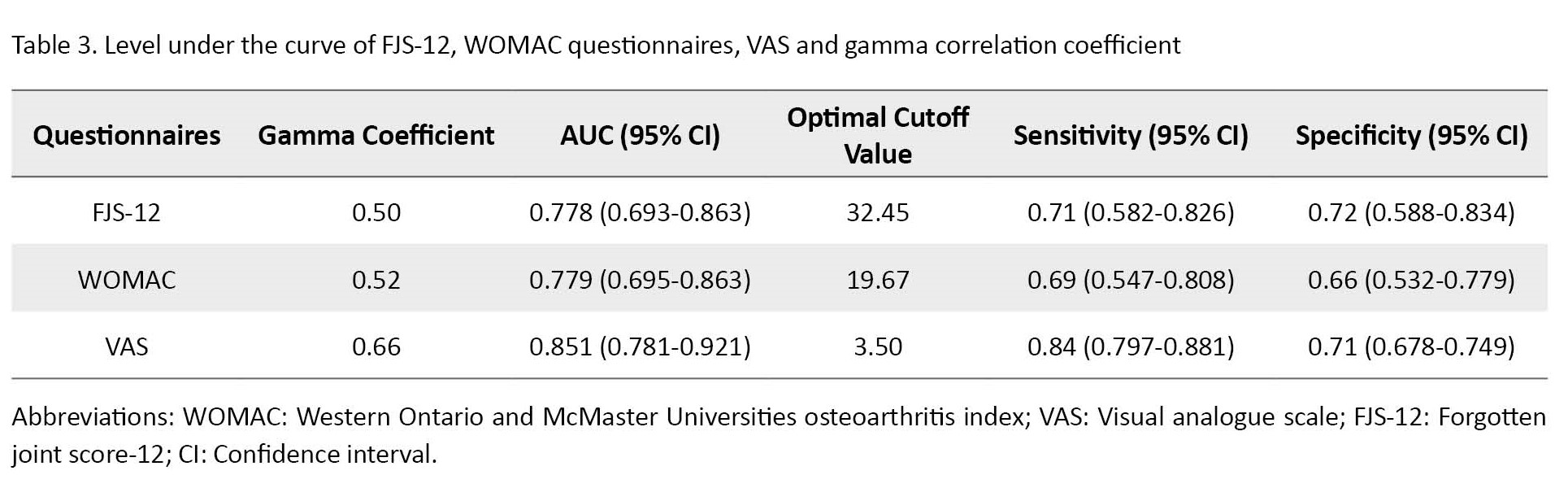
The gamma correlation coefficient between the pre and post-treatment scores with the GRC criterion for FJS-12 has been calculated at 0.5; according to the utilized references, it is in the average to good correlation range [10].
Discussion
The Persian version of FJS-12 used in this study has suitable reliability and validity regarding psychometric properties [14]. This study was conducted to examine the responsiveness of the FJS-12 questionnaire in patients following hip and knee arthroplasty as well as ACL reconstruction and the course of physiotherapy post-surgery based on the rehabilitation guideline of each surgery. The present research did not use a special surgery group as the sample, since it eliminated the effect of type of surgery on the pre- and post-treatment changes, and given the diversity of the operations, an older age range of subjects participated in this research. Also, no studies were found that collated multi-group information regarding the responsiveness of the hip and knee versions of the FJS-12. In addition, so far studies have mostly calculated responsiveness through internal responsiveness, while the strength of the external responsiveness measures the pre- and post-treatment score changes as the health status criterion [27, 28].
The results obtained from the Gamma correlation indicated that this relationship between the changes in FJS-12 score and GRC was average with a value of 0.5 in this time frame. Meanwhile, according to the ROC analysis, all of the examined outcomes have acceptable responsiveness. In addition, MCIC with numbers 32.45, 19.67, and 3.5 for Persian FJS-12, WOMAC, and VAS respectively should manifest a proper change in the health status pre- and post-treatment.
The results of correlation analysis between each outcome measure by GRC have been average. Three reasons exist behind the limitation of the GRC criterion, which can deal with the justification of this average association. The first is the transient improvement or aggravation at the time of selecting the GRC score, which can affect the general perception of the patient about their status. Secondly, the GRC criterion may be different with questionnaire items about health status. Finally, it is mentally difficult to decide on the extent of pre- and post-intervention change due to recall bias [29].
The AUC presents the ability of an instrument to differentiate individuals who experienced change (improved) vs. unchanged (unimproved) individuals [21]. The AUC results of all outcome measures with acceptable external responsiveness suggest differentiative power between improved and unimproved subjects. The acceptable AUC of 0.77 was obtained for the Persian FSJ-12, similar to the AUC of the Italian version 0.76 [3].
MCIC of the desired cutoff point, obtained from ROC analysis, helps therapists and researchers identify significant changes after treatment. The MCIC obtained for FJS-12 has been 32.45, meaning that to identify improvement seven weeks after surgery, the FJS-12 score should at least change by 32.45. However, the MCIC of the Italian version reached 17.5 six months and one year after THA, and for the English version 16.6 in those with TKA [30]. The difference between these scores of different studies can be due to the different designs of each study.
Conclusion
The results obtained from both correlation and ROC methods indicated that the Persian version of the FJS-12 and WOMAC questionnaire has acceptable responsiveness as a criterion for measuring the extent of change in subjects following THA, TKA, and ACL reconstruction operations. Also, the value of MCIC can help Persian-speaking therapists and researchers identify proper changes in the health status.
This study had limitations. First, the use of the GRC criterion which can cause recall, though a short-term follow-up period (seven weeks on average in the study) can mitigate this bias [29]. Secondly, in Iranian culture, the extent of physical activity is lower in senior citizens, and item 12 of the questionnaire was unanswered in most subjects. Thirdly, to explore the responsiveness based on pathology, it is suggested to investigate each group independently with a suitable sample size.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1401.177). The method of this study was approved by the Institutional Review Board of Iran University of Medical Sciences.
Funding
This work was a part of the master’s thesis of Monireh Il Saadatmand, approved by Iran University of Medical Sciences.
Authors' contributions
Conceptualization: Soheil Mansour Sohani; Supervision: Ali Amiri and Ali Yeganeh; Methodology: Reza Salehi; Funding acquisition and resources: Monireh. Il Saadatmand and Soheil Mansour Sohani; Writing-original draft: Monireh. Il Saadatmand; Investigation, writing–review & editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all the participants in this study, and all the people who helped us in this study.
Total hip and knee arthroplasty are widely used for treating degenerative diseases of the hip and knee joints. According to statistics, 1 million total hip arthroplasty (THA) and total knee arthroplasty (TKA) are performed annually in the US. It is predicted to reach 3.5 million cases annually in 2030 [1]. The anterior cruciate ligament (ACL) reconstruction surgery is one of the standard treatments in the US; annually out of 200 000 ACL injuries, half of them lead to reconstruction [2]. These operations have various complications, including bone cement implantation syndrome, fracture during operation, residual pain, damage to muscular structures and ligaments, and dislocation. These complications affect the surgical outcome, quality of life, and joint function [3].
Joint awareness simply refers to any unwanted perception of a joint. These perceptions include strong sensations, such as pain, or weak sensations, such as mild stiffness, mental dysfunction, and any discomfort. Joint awareness is a negative concept, since healthy joints do not cause awareness in daily life, and are essentially forgotten [4]. Reaching a lack of joint awareness, similar to a healthy joint, is regarded as a post-surgical evaluation test. The ultimate goal is to achieve the stage of forgetting joint following total hip and TKA surgeries as well as ACL reconstruction, in addition to restoring the normal function and sensation of joints to a healthy joint state. This is an aim that is difficult to achieve and requires precise measurement [5].
Clinical instruments to evaluate disorders may not be able to specify the effect of musculoskeletal pains in all aspects of the person’s life. The constraints of clinical tools and identification of the need to engage the patient’s view in examining the treatment outcome led to the development and validation of PROM tools to evaluate the person’s activity and participation [6, 7, 8].
Regardless of the type of instrument and scale, an effective assessment of a scale should have three features, validity, reliability, and responsiveness: the scale should be able to find crucial clinical changes [9]. In clinical practice, a tool with good responsiveness should be able to detect changes in the effects of two treatments with different qualities [10]. Responsiveness has two aspects, internal and external responsiveness. The internal means the ability of the tool to identify changes along a specific time interval. External responsiveness refers to the comparison of the changes in a scale with similar changes in a reference scale [11]. The internal responsiveness is calculated through two methods, effect size, and standard response mean. The common method to evaluate external responsiveness is the receiving operator characteristic (ROC) curve [12]. Typically, the responsiveness of minimal clinically important change (MCIC) means the minimum extent of change in the score which is significant by the patient. Knowing MCIC helps the therapist and researchers to understand whether the treatment has progressed towards improvement [10, 13].
The forgotten joint score-12 (FJS-12) questionnaire is a patient-oriented tool developed in two separate versions in 2012 to measure the outcomes in patients under conservative and operative treatments in the knee and hip regions. This questionnaire measures the extent of joint awareness and the ability of patients to forget the involved leg during daily activities. It indicates the extent of acceptance of the new joint as a normal part of the body in the knee and hip regions during various daily activities [5]. The Persian version of FJS-12 is a reliable and valid tool for those seeking to undergo ACL reconstruction as well as THA [1, 14]. However, currently, the responsiveness of the Persian version of this questionnaire has not been examined so far. Accordingly, the responsiveness of the FJS-12 questionnaire has been evaluated by obtaining the MCIC as a patient-oriented tool to properly identify changes in the health status of patients before and after THA and TKA as well as ACL reconstruction.
Materials and Methods
From May 2022 to November 2022, 112 candidates for THA and TKA as well as ACL reconstruction referred to the orthopedic clinics of, Rasoul-e-Akram and Moheb Mehr hospitals as well as the Nava orthopedic clinic. The diagnosis of the candidate of each surgery was performed by an orthopedic specialist based on radiographic and magnetic resonance imaging (MRI) images [15, 16]. The inclusion criteria included patients above 18 years of age, with a literacy of high school and above, as well as Persian official language. The exclusion criteria included those who did not answer more than 8 items of the questionnaire, unwillingness to continue participation in the research, and failure to complete the postoperative physiotherapy sessions. The participants filled out the form of written informed consent before participating in the research.
Forgotten joint score-12 (FJS-12)
This questionnaire was translated in 2021 by Sohani et al., and its reliability and validity were examined among patients after ACL reconstruction [14]. This questionnaire was first designed in English for patients with arthritis of hip and knee joints who have undergone joint replacement surgery. This questionnaire includes 12 items measuring the extent of awareness about the joint along various daily activities. The score is obtained between 0-100. The highest possible score indicates the minimum extent of awareness of the operated joint; if more than four responses are lost, the total score cannot be calculable [5].
Western Ontario and McMaster Universities osteoarthritis index (WOMAC)
The patient-oriented questionnaire is the most widely used outcome measure in patients with lower limb arthritis, designed by Bellamy and Buchanan in 1988. It includes 33 items, covering four dimensions, symptoms (5 items), stiffness (2 items), pain (9 items), and daily life functioning (17 items). There are five options for each item, with the best response recorded as ‘never or none’, while the worst response is recorded as ‘very severe or always’. Here, higher scores represent a better status and less pain. The Persian version of this questionnaire has been translated and validated for use in Iran for patients with knee osteoarthritis. Acceptable evidence shows the reliability, validity, and responsiveness of this questionnaire [17].
Method
The present research is an interventional (quasi-experimental) method, while also belonging to methodological studies of diagnostic tests. First, the subjects received and completed WOMAC, FJS-12, and visual analogue scale (VAS) questionnaires one week before surgery. Next, after 8 weeks before surgery and completing the full course of physiotherapy three sessions per week, they completed the previous questionnaires plus the global rating of change (GRC). The GRC is a seven-score criterion, which asks questions about the extent of improvement post-treatment [18]. In this study, the physiotherapy treatment has not been studied as a control, since the focus of this study has been on the responsiveness of a measurement tool, and does not emphasize the effectiveness of the treatment method [9, 19]. Nevertheless, the physiotherapy treatment has been performed according to physiotherapy guidelines following THA and TKA as well as ACL reconstruction, including improvements in the range of motion of the involved joint, increase in the muscle strength and endurance, as well as attempts for full loading on the involved joint.
Statistical analysis
All data were introduced into SPSS software, version 26 and Microsoft Excel, version 2016. The significance level was considered P<0.05. The mean and standard deviation of the continuous quantitative and ranked qualitative variables were measured. Also, the Kolmogorov-Smirnov test was used to examine the normality of data distribution. Based on the GRC criterion, the subjects were divided into two groups, improved (I have improved very much and I have improved much), and unimproved (I have improved slightly, I have not changed, I have got worse slightly, I have got worse much, and I have got worse very much) [12].
Changes in the pre-surgery and post-treatment scores were measured for each criterion. Positive score changes indicate improvement, while negative score changes indicate deterioration [20]. The statistical method of external responsiveness is especially interesting for researchers who focus on responsiveness [11, 20]. The responsiveness in this study is measured using two methods of ROC and correlation between the pre- and post-score changes with the GRC score.
ROC analysis measures the differentiation between the improved and unimproved groups resulting from the GRC criterion based on sensitivity and specificity. Sensitivity means finding a clinical change when it exists, while specificity means the ability to find no clinical change when a change is present [10, 12]. The cut-off point has been calculated through several changes in the sensitivity and specificity scores. The sensitivity is drawn on the vertical axis (Y), while specificity-1 is drawn on the horizontal axis (X) for all cutoff points. The area under the curve (AUC) offers some information about the ability of the instrument to identify the improved and unimproved subjects [21, 22]. The accuracy of the AUC based on academic scoring is as follows: 0.90-1.00=excellent, 0.80-0.89=good, 0.70-0.79=average, 0.60-0.69=poor, and 0.00-0.59=fail. An AUC score above 0.70 means suitable responsiveness [23, 24]. The cutoff point close to the top left corner of the AUC is extracted as the highest sensitivity and specificity as the MCIC [25]. MCIC in this study shows whether a proper change in FJS-12 scores has occurred for changes in joint awareness.
The Gamma correlation coefficient has been calculated to measure the relationship between the GRC ranked data and changes in pre/post-treatment scores. A positive score difference is expected to indicate a high improvement score in GRC. Correlation coefficients <0.25, 0.25-0.50, 0.50-0.75, and >0.75 represent no or trivial relationship, weak relationship, average to good relationship, and good to excellent relationship, respectively. A score close to 1 shows that the mentioned instrument can measure changes in health status by GRC [13, 26].
Results
In this study, 25 subjects (22%) with ACL reconstruction, 33 subjects (30%) with THA, and 54 subjects with TKA (48%) participated, respectively. Table 1 presents the demographic characteristics of the subjects plus the clinical data.
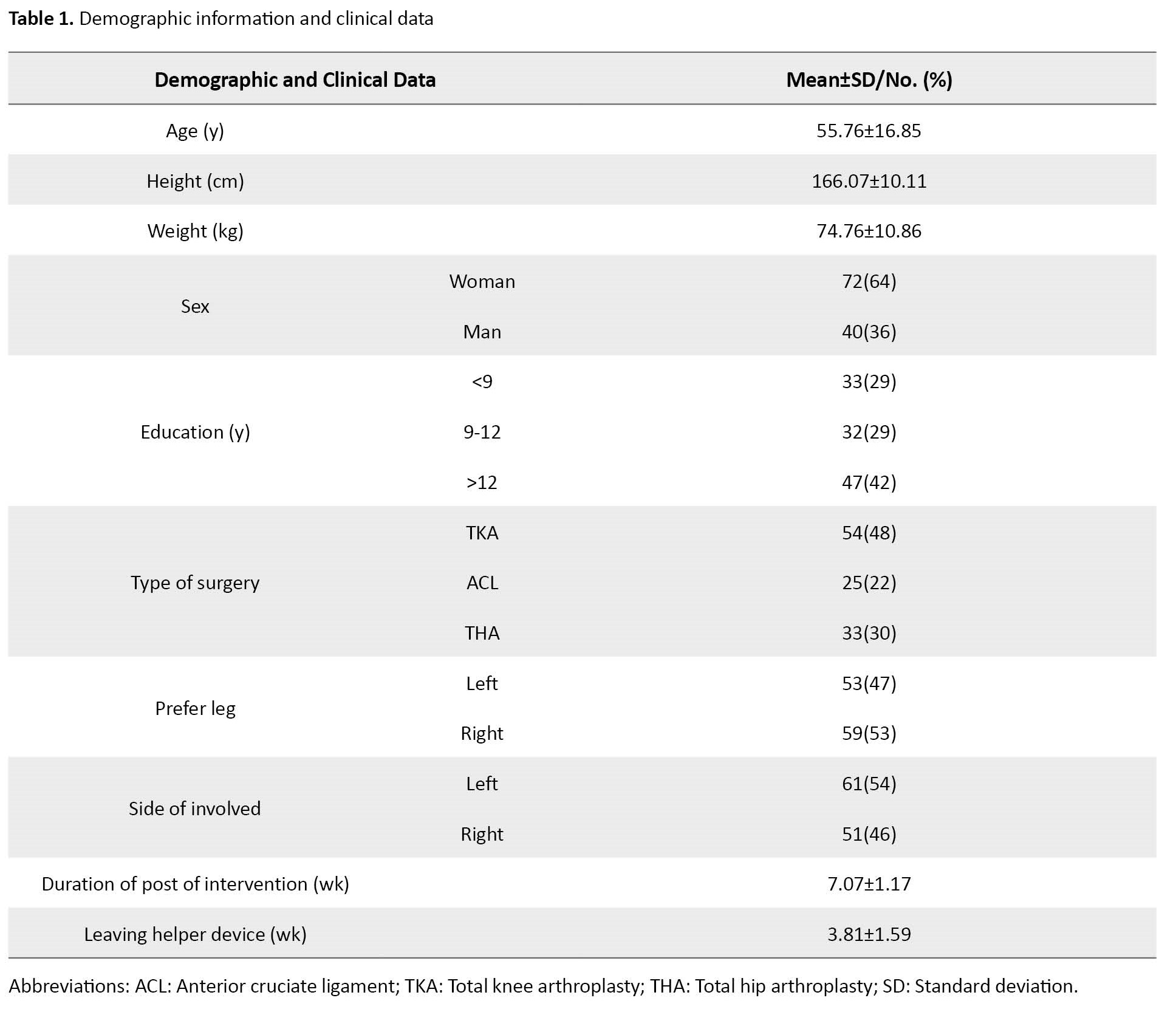
Table 2 presents descriptive statistics, including Means±SD of each questionnaire pre- and post-treatment.

According to GRC classification, 20 subjects chose ‘I have improved very much’ (18%), 36 subjects chose ‘I have improved much’ (32%), 42 subjects chose ‘I have improved slightly’ (38%), 9 subjects chose ‘I have not changed’ (8%), 3 subjects chose ‘I have worsened’ (3%), and 2 subjects chose ‘I have worsened very much’ (2%). Thus, 56 subjects fell in the improved group (50%) and 56 subjects in the unimproved group (50%).
In this study, the AUC of each questionnaire has been calculated with a confidence interval (CI) of 95%. Their AUC for FJS-12, WOMAC, and VAS has been (0.778, 0.693-0.863), (0.779, 0.695-0.863), and (0.851, 0.782-0.921). Table 3 presents the desired cutoff points of each questionnaire as well as the specificity and sensitivity of each point.
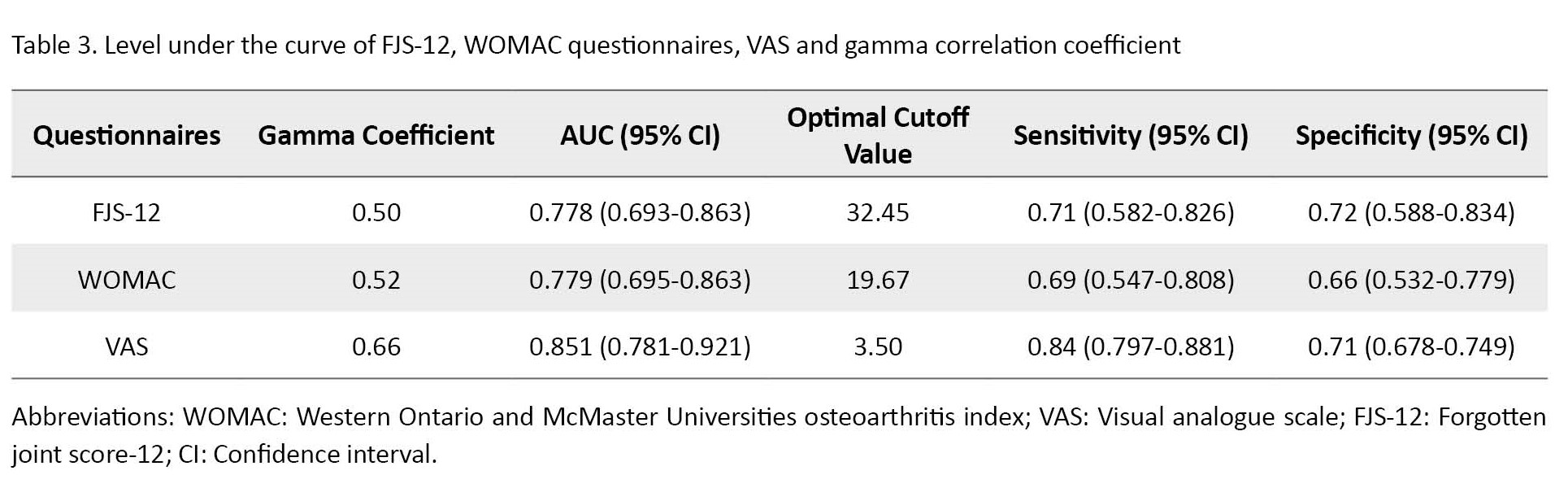
The gamma correlation coefficient between the pre and post-treatment scores with the GRC criterion for FJS-12 has been calculated at 0.5; according to the utilized references, it is in the average to good correlation range [10].
Discussion
The Persian version of FJS-12 used in this study has suitable reliability and validity regarding psychometric properties [14]. This study was conducted to examine the responsiveness of the FJS-12 questionnaire in patients following hip and knee arthroplasty as well as ACL reconstruction and the course of physiotherapy post-surgery based on the rehabilitation guideline of each surgery. The present research did not use a special surgery group as the sample, since it eliminated the effect of type of surgery on the pre- and post-treatment changes, and given the diversity of the operations, an older age range of subjects participated in this research. Also, no studies were found that collated multi-group information regarding the responsiveness of the hip and knee versions of the FJS-12. In addition, so far studies have mostly calculated responsiveness through internal responsiveness, while the strength of the external responsiveness measures the pre- and post-treatment score changes as the health status criterion [27, 28].
The results obtained from the Gamma correlation indicated that this relationship between the changes in FJS-12 score and GRC was average with a value of 0.5 in this time frame. Meanwhile, according to the ROC analysis, all of the examined outcomes have acceptable responsiveness. In addition, MCIC with numbers 32.45, 19.67, and 3.5 for Persian FJS-12, WOMAC, and VAS respectively should manifest a proper change in the health status pre- and post-treatment.
The results of correlation analysis between each outcome measure by GRC have been average. Three reasons exist behind the limitation of the GRC criterion, which can deal with the justification of this average association. The first is the transient improvement or aggravation at the time of selecting the GRC score, which can affect the general perception of the patient about their status. Secondly, the GRC criterion may be different with questionnaire items about health status. Finally, it is mentally difficult to decide on the extent of pre- and post-intervention change due to recall bias [29].
The AUC presents the ability of an instrument to differentiate individuals who experienced change (improved) vs. unchanged (unimproved) individuals [21]. The AUC results of all outcome measures with acceptable external responsiveness suggest differentiative power between improved and unimproved subjects. The acceptable AUC of 0.77 was obtained for the Persian FSJ-12, similar to the AUC of the Italian version 0.76 [3].
MCIC of the desired cutoff point, obtained from ROC analysis, helps therapists and researchers identify significant changes after treatment. The MCIC obtained for FJS-12 has been 32.45, meaning that to identify improvement seven weeks after surgery, the FJS-12 score should at least change by 32.45. However, the MCIC of the Italian version reached 17.5 six months and one year after THA, and for the English version 16.6 in those with TKA [30]. The difference between these scores of different studies can be due to the different designs of each study.
Conclusion
The results obtained from both correlation and ROC methods indicated that the Persian version of the FJS-12 and WOMAC questionnaire has acceptable responsiveness as a criterion for measuring the extent of change in subjects following THA, TKA, and ACL reconstruction operations. Also, the value of MCIC can help Persian-speaking therapists and researchers identify proper changes in the health status.
This study had limitations. First, the use of the GRC criterion which can cause recall, though a short-term follow-up period (seven weeks on average in the study) can mitigate this bias [29]. Secondly, in Iranian culture, the extent of physical activity is lower in senior citizens, and item 12 of the questionnaire was unanswered in most subjects. Thirdly, to explore the responsiveness based on pathology, it is suggested to investigate each group independently with a suitable sample size.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1401.177). The method of this study was approved by the Institutional Review Board of Iran University of Medical Sciences.
Funding
This work was a part of the master’s thesis of Monireh Il Saadatmand, approved by Iran University of Medical Sciences.
Authors' contributions
Conceptualization: Soheil Mansour Sohani; Supervision: Ali Amiri and Ali Yeganeh; Methodology: Reza Salehi; Funding acquisition and resources: Monireh. Il Saadatmand and Soheil Mansour Sohani; Writing-original draft: Monireh. Il Saadatmand; Investigation, writing–review & editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all the participants in this study, and all the people who helped us in this study.
References
- Maradit Kremers H, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015; 97(17):1386-97. [DOI:10.2106/JBJS.N.01141] [PMID] [PMCID]
- Paschos NK, Howell SM. Anterior cruciate ligament reconstruction: Principles of treatment. EFORT Open Rev. 2016; 1(11):398-408. [DOI:10.1302/2058-5241.1.160032] [PMID] [PMCID]
- Longo UG, De Salvatore S, Piergentili I, Indiveri A, Di Naro C, Santamaria G, et al. Total hip arthroplasty: Minimal clinically important difference and patient acceptable symptom state for the forgotten joint score 12. Int J Environ Res Public Health. 2021; 18(5):2267.[DOI:10.3390/ijerph18052267] [PMID] [PMCID]
- Behrend H, Giesinger K, Zdravkovic V, Giesinger JM. Validating the forgotten joint score-12 in patients after ACL reconstruction. Knee. 2017; 24(4):768-74. [DOI:10.1016/j.knee.2017.05.007] [PMID]
- Behrend H, Giesinger K, Giesinger JM, Kuster MS. The “forgotten joint” as the ultimate goal in joint arthroplasty: Validation of a new patient-reported outcome measure. J Arthroplasty. 2012; 27(3):430-6.e1. [DOI:10.1016/j.arth.2011.06.035] [PMID]
- Zelle BA, Herzka A, Harner CD, Irrgang JJ. Evaluation of clinical outcomes in anterior cruciate ligament surgery. Oper Tech Orthop. 2005; 15(1):76-84. [DOI:10.1053/j.oto.2004.11.013]
- Cieza A, Brockow T, Ewert T, Amman E, Kollerits B, Chatterji S, et al. Linking health-status measurements to the international classification of functioning, disability and health. J Rehabil Med. 2002; 34(5):205-10. [DOI:10.1080/165019702760279189] [PMID]
- Fitzpatrick R, Davey C, Buxton MJ, Jones D. Evaluating patient-based outcome measures for use in clinical trials: A review. Health Technol Assess. 1998; 2(14):1-74. [DOI:10.3310/hta2140]
- Stratford PW, Binkley JM, Riddle DL. Health status measures: Strategies and analytic methods for assessing change scores. Phys Ther. 1996; 76(10):1109-23. [DOI:10.1093/ptj/76.10.1109] [PMID]
- Lehman LA, Velozo CA. Ability to detect change in patient function: Responsiveness designs and methods of calculation. J Hand Ther. 2010; 23(4):361-70; quiz 371. [DOI:10.1016/j.jht.2010.05.003] [PMID]
- Husted JA, Cook RJ, Farewell VT, Gladman DD. Methods for assessing responsiveness: A critical review and recommendations. J Clin Epidemiol. 2000; 53(5):459-68. [DOI:10.1016/S0895-4356(99)00206-1] [PMID]
- Lehman LA, Sindhu BS, Shechtman O, Romero S, Velozo CA. A comparison of the ability of two upper extremity assessments to measure change in function. J Hand Ther. 2010; 23(1):31-40. [DOI:10.1016/j.jht.2009.09.006] [PMID]
- de Yébenes Prous MJ, Rodríguez Salvanés F, Carmona Ortells L. [Responsiveness of outcome measures (Spanish)].Reumatol Clin. 2008; 4(6):240-7. [DOI:10.1016/S1699-258X(08)75545-1] [PMID]
- Momeni E, Mansour Sohani S, Nourizadeh Dehkordi S, Amiri A, Amini M. Validity and reliability of the Persian Version of the Forgotten Joint Score-12 Questionnaire in Iranian patients following anterior cruciate ligament reconstruction. Func Disabil J. 2021; 4(1):42. [DOI:10.32598/fdj.4.42]
- Mirghaderi SP, Raeini AG, Gholamshahi H, Mortazavi SMJ, Shafiei SH, Sheikhvatan M. Content validity and reliability of the Persian Version of the Forgotten Joint Score Questionnaire in patients undergoing total hip arthroplasty. Arthroplasty Today. 2022; 15:40-2. [DOI:10.1016/j.artd.2022.01.031] [PMID] [PMCID]
- Moura JL, Kandhari V, Rosenstiel N, Helfer L, Queirós CM, Abreu FG, et al. Figure-of-4 cruciate remnant objective assessment test reducibility of anterior cruciate ligament stump for feasibility of arthroscopic primary anterior cruciate ligament repair. Arthrosc Tech. 2019; 8(6):e637-40. [DOI:10.1016/j.eats.2019.02.008] [PMID] [PMCID]
- Ebrahimzadeh MH, Makhmalbaf H, Birjandinejad A, Keshtan FG, Hoseini HA, Mazloumi SM. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) in Persian speaking patients with knee osteoarthritis. Arch Bone Jt Surg. 2014; 2(1):57-62. [PMID]
- Kamper SJ, Maher CG, Mackay G. Global rating of change scales: A review of strengths and weaknesses and considerations for design. J Man Manip Ther. 2009; 17(3):163-70. [DOI:10.1179/jmt.2009.17.3.163] [PMID] [PMCID]
- Shultz S, Olszewski A, Ramsey O, Schmitz M, Wyatt V, Cook C. A systematic review of outcome tools used to measure lower leg conditions. Int J Sports Phys Ther. 2013; 8(6):838-48. [PMID]
- de Vet HC, Bouter LM, Bezemer PD, Beurskens AJ. Reproducibility and responsiveness of evaluative outcome measures. Theoretical considerations illustrated by an empirical example. Int J Technol Assess Health Care. 2001; 17(4):479-87. [DOI:10.1017/S0266462301107038] [PMID]
- Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007; 60(1):34-42. [DOI:10.1016/j.jclinepi.2006.03.012] [PMID]
- Hand DJ, Till RJ. A simple generalisation of the area under the ROC curve for multiple class classification problems. Mach Learn. 2001; 45(2):171-86. [Link]
- Lin CW, Moseley AM, Refshauge KM, Bundy AC. The Lower Extremity Functional Scale has good clinimetric properties in people with ankle fracture. Phys Ther. 2009; 89(6):580-8. [DOI:10.2522/ptj.20080290] [PMID]
- Mostafaee N, Negahban H, Shaterzadeh Yazdi MJ, Goharpey S, Mehravar M, Pirayeh N. Responsiveness of a Persian version of Knee Injury and Osteoarthritis Outcome Score and Tegner activity scale in athletes with anterior cruciate ligament reconstruction following physiotherapy treatment. Physiother Theory Pract. 2020; 36(9):1019-26. [DOI:10.1080/09593985.2018.1548672] [PMID]
- Ansari NN, Komesh S, Naghdi S, Fakhari Z, Alaei P. Responsiveness of minimal clinically important change for the Persian Functional Rating Index in patients with chronic low back pain. Asian Spine J. 2019; 13(1):111-8. [DOI:10.31616/asj.2018.0107] [PMID] [PMCID]
- Negahban H, Mostafaee N, Sohani SM, Hessam M, Tabesh H, Montazeri A. Responsiveness and minimally important differences for selected Persian-version of outcome measures used in patients with patellofemoral pain syndrome. Disabil Rehabil. 2015; 37(14):1285-90. [DOI:10.3109/09638288.2014.962107] [PMID]
- Revicki D, Hays RD, Cella D, Sloan J. Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J Clin Epidemiol. 2008; 61(2):102-9. [DOI:10.1016/j.jclinepi.2007.03.012] [PMID]
- Çelik D, Çoban Ö, Kılıçoğlu Ö. Minimal clinically important difference of commonly used hip-, knee-, foot-, and ankle-specific questionnaires: A systematic review. J Clin Epidemiol. 2019; 113:44-57. [DOI:10.1016/j.jclinepi.2019.04.017] [PMID]
- Norman GR, Stratford P, Regehr G. Methodological problems in the retrospective computation of responsiveness to change: The lesson of Cronbach. J Clin Epidemiol. 1997; 50(8):869-79. [DOI:10.1016/S0895-4356(97)00097-8] [PMID]
- Clement ND, Scott CEH, Hamilton DF, MacDonald D, Howie CR. Meaningful values in the Forgotten Joint Score after total knee arthroplasty. Bone Joint J. 2021; 103-B(5):846-54. [DOI:10.1302/0301-620X.103B5.BJJ-2020-0396.R1] [PMID]
Type of Study: Research |
Subject:
Physiotherapy
Received: 2023/02/11 | Accepted: 2023/07/23 | Published: 2023/02/6
Received: 2023/02/11 | Accepted: 2023/07/23 | Published: 2023/02/6