Volume 5, Issue 1 (Continuously Updated 2022)
Func Disabil J 2022, 5(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mirhajian S S, Salehi R, Sohani S M. Investigating the Responsiveness of the Persian Version of the Core Outcome Measure Index Neck Questionnaire in People With Non-specific Chronic Neck Pain. Func Disabil J 2022; 5 (1) : 62
URL: http://fdj.iums.ac.ir/article-1-205-en.html
URL: http://fdj.iums.ac.ir/article-1-205-en.html
1- Iranian Center of Excellence in Physiotherapy, Rehabilitation Research Center, Department of Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
2- Iranian Center of Excellence in Physiotherapy, Rehabilitation Research Center, Department of Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran. ,sohani.soheil@gmail.com
2- Iranian Center of Excellence in Physiotherapy, Rehabilitation Research Center, Department of Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 1042 kb]
(482 Downloads)
| Abstract (HTML) (1642 Views)
Full-Text: (627 Views)
Introduction
Neck pain is one of the most common musculoskeletal problems following low back pain; hence, it is considered one of the causes of disability in the population [1]. The prevalence of neck pain is between 30% to 50% per year. Based on the duration of the symptoms, neck pain is divided into two groups, namely acute and chronic. When neck pain continues for more than 12 weeks, it is defined as chronic neck pain [2]. According to the Global Burden of Disease Study 2010, neck pain is the fourth leading cause of years lost due to disability after low back pain, depression, and joint pain [3]. The occurrence of neck pain is more common in women compared to men and among middle-aged people [4]. Genetics, psychological factors, sleep disorders, smoking, and a sedentary lifestyle are the variables of the causative factors related to neck pain [2, 5, 6].
Evaluation is always considered an important part of any therapeutic intervention [7] because, in addition to considering pathology and its physical aspects, therapists should consider the contribution of psychological factors in the occurrence of long-term disability in people with neck pain [8]. In recent years, self-report measurement tools have played a very important role in measuring health outcomes in spine-related diseases, thus helping the treatment process of patients [9]. The results of the studies showed that the evaluation of the consequences is the best criterion for evaluating chronic pain in affected people; therefore, it is necessary to evaluate the impact of chronic disorders on individuals’ health as well as the results of therapeutic interventions [7]. Among these outcome-based tools, we can mention the neck disability index, the North American spine society questionnaire, the Copenhagen neck functional disability scale, the Northwick Park neck pain questionnaire, the neck pain and disability scale, and the core outcome measure index [10-14].
In evaluating these patients, it is recommended to evaluate the following 5 dimensions: pain, function, well-being, disability at work, and disability in society [15]. During the last two decades, a large number of these questionnaires have been compiled; however, none of these tools can fully evaluate the consequences of chronic disorders correctly [16]. In addition, these tools cannot evaluate different dimensions of the outcome; therefore, a standard set of tools is needed to evaluate the different outcomes of disorders [15]. For this purpose, in 1998, a group of researchers developed a standard outcome measurement tool called the core outcome measure index (COMI) for patients with low back pain. COMI includes 5 areas as follows: pain, function, general health conditions, disability, and satisfaction [9, 15]. The COMI questionnaire has been registered with the European Spine Association to measure the outcome following spine surgery and non-surgical treatments and is currently used worldwide [17]. The psychometric properties of COMI were evaluated and the results showed acceptable validity and reliability of the questionnaire [16]. The COMI neck questionnaire was compiled and used as a supplement to COMI back to evaluate chronic neck pain patients and patients who underwent neck arthroplasty surgery [18, 19]. This reliable tool has been translated and localized into Turkish, Polish, Italian, Persian, and Japanese languages [20-24].
Responsiveness is an essential psychometric feature of an instrument and describes the ability of an instrument to show a clinically significant change in a patient’s health status over time [25]. From a clinical perspective, an outcome measure with response characteristics should be able to differentiate between treatment effects and random and spontaneous changes [26]. The measurement tool should be able to show real changes for better or worse. The reliability and reproducibility of the Persian version of the COMI neck questionnaire have been investigated and determined that the Persian version of this questionnaire has good reliability and reproducibility in people with neck pain; however, the ability of this questionnaire to respond to treatment has not been investigated. Therefore, this study aims to investigate the responsiveness of the Persian version of the COMI neck questionnaire and to determine the minimum clinically important change scores in patients with chronic neck pain after a course of physiotherapy treatment.
Materials and Methods
Study participants
A total of 104 patients who were referred to physiotherapy because of being diagnosed with chronic neck pain participated in this study by filling out the informed consent form. The diagnosis of chronic neck pain was made by an orthopedic through clinical examination and radiological findings. The inclusion criteria were as follows: age range between 18 and 50 years, ability to read and write and understand the Persian language, non-specific neck pain for more than 3 months, minimum education at the level of high school, and undergoing a course of physiotherapy treatment [18, 23, 27]. Also, the exclusion criteria were having neck pain due to deformity, fracture, spinal canal stenosis of the cervical vertebra, the presence of central or peripheral nervous system disease, systemic diseases, the use of strong painkillers during the period of physiotherapy treatment, or any other concurrent treatment, mental and cognitive diseases, chronic lung or kidney diseases, and a recent history of stroke or heart attack [18, 23, 27].
Study design
This study was based on a prospective cohort design. All patients received and completed the Persian version of the COMI neck questionnaire before the first session of physiotherapy treatment. The physiotherapy program included electrotherapy (TENS, US. hot pack), range of motion exercises, deep neck muscle strengthening, stabilization exercises, soft tissue stretching, and cervical facet joint mobilization. It was not necessary to use the same protocol in all clinics because the purpose of this plan was not to evaluate the protocol but to evaluate the ability to respond to treatment [28, 29]. After 10 treatment sessions, the subjects were re-evaluated and the Persian version of the COMI neck questionnaire was completed again by the patients. In addition to completing the mentioned questionnaire, the patients received and completed the global rating of change (GRC) questionnaire in the final session of the treatment.
Outcome measures
The COMI questionnaire includes 7 questions as follows: 2 questions related to pain, 1 question related to function, 1 question related to well-being, 2 questions related to disability, and 1 question related to satisfaction. The COMI neck questionnaire is designed based on a 10-question graphic scale, and the scores are calculated as follows: a score of 0 indicates the best condition and a score of 10 indicates the worst condition in patients [15, 18].
Assessment tool
The GRC questionnaire is a valid tool that has been used as a reference tool in most of the studies whose purpose was to check the response. This scale includes the question of how much the patient has changed compared to the first day of the visit. The rating of this scale is as follows: “7=I have improved a lot”, “6=I have improved relatively”, “5=I have improved a little”, “4=I have not changed”, “3=I have gotten a little worse”, “2=I have become much worse”, “1=I have become much worse”.
Statistical analysis
The data obtained in this study were analyzed using the SPSS software, version 26. The level of statistical significance was considered P<0.05. To measure responsiveness, the change in scores between the first and last sessions for the COMI neck questionnaire was calculated. The change score was obtained by subtracting the score of the first session from the score of the last session; therefore, a positive score indicated improvement and a negative score indicated worsening of the patient’s condition [30]. In this study, responsiveness was calculated using 2 methods as follows: the receiver operating characteristic (ROC) curve method and the correlation calculation. The ROC curve is the most common method for calculating responsiveness and uses the overall scale of change as an external measure [31]. Functional scales can be considered a diagnostic test to differentiate between patients who have recovered from patients who have not recovered, considering that the ROC curve has been developed to detect recovery or non-recovery using an external criterion. Evaluating the responsiveness of functional scales is similar to evaluating the discrimination capability of a diagnostic test. In this case, the condition to be determined is whether a clinically significant change has occurred. Functional scale scores, similar to other diagnostic tests, may show random changes over time and can never be flawless measurements, and there are “true positive” and “false positive” changes in the scale scores. Functionality happens over time; therefore, one of the ways to evaluate responsiveness is to calculate the sensitivity and specificity of the scales to determine improvement or deterioration. The ROC curve provides information about the sensitivity and specificity for detecting improvement by an external measure. This curve includes a graph of the true positive rate (sensitivity) versus the false positive rate (specificity-1) for each of the possible cut points in the change score [31, 32]. Sensitivity means the ability of a tool to identify a clinical change when a change exists. Specificity means the ability of a tool to identify the lack of clinical change when no change exists [31].
The area under the ROC curve can be interpreted as the probability of correctly identifying a cured patient from a pair of cured and uncured patients that are randomly selected. It is also more for distinguishing between the two groups of improved and non-improved patients that are determined by external criteria [31, 32]. The range of this area is theoretically from 0 (no accuracy in differentiating the improved group from the unimproved group) to 1 (complete and excellent accuracy). The area under the curve value greater than 0.7 indicates high responsiveness [33].
One of the cut points obtained from the ROC curve is the minimal clinically important difference (MCID). MCID is the number of scores required to show a clinically significant change [31]. In this study, the best cut point was chosen as the change score in the COMI neck questionnaire, which indicates a clinical change in the patient’s functional ability [31]. The best method for detecting MCID is ROC; the point of the ROC curve that is closer to the upper and left corner of the diagram is used to estimate the minimum change score necessary to distinguish improved from non-improved patients [34]. This appropriate cut-off point is the point that has the highest sensitivity and specificity along with the ability to differentiate between improved and non-improved patients [33].
Responsiveness is also obtained by calculating the correlation between the change score of the COMI neck questionnaire and the overall change criterion using the gamma correlation coefficient. According to the numerical information of the general scale of change, we used the gamma correlation coefficient to determine the relationship between the scores of the COMI neck questionnaire and the score of the patient’s general scale of change. In this method, the strength of correlation indicates responsiveness. The correlation coefficients less than 0.25, 0.25 to 0.5, 0.5 to 0.75, and more than 0.75, respectively, indicate no or little connection, weak connection, medium to good connection, and connection it is good to excellent [31].
Results
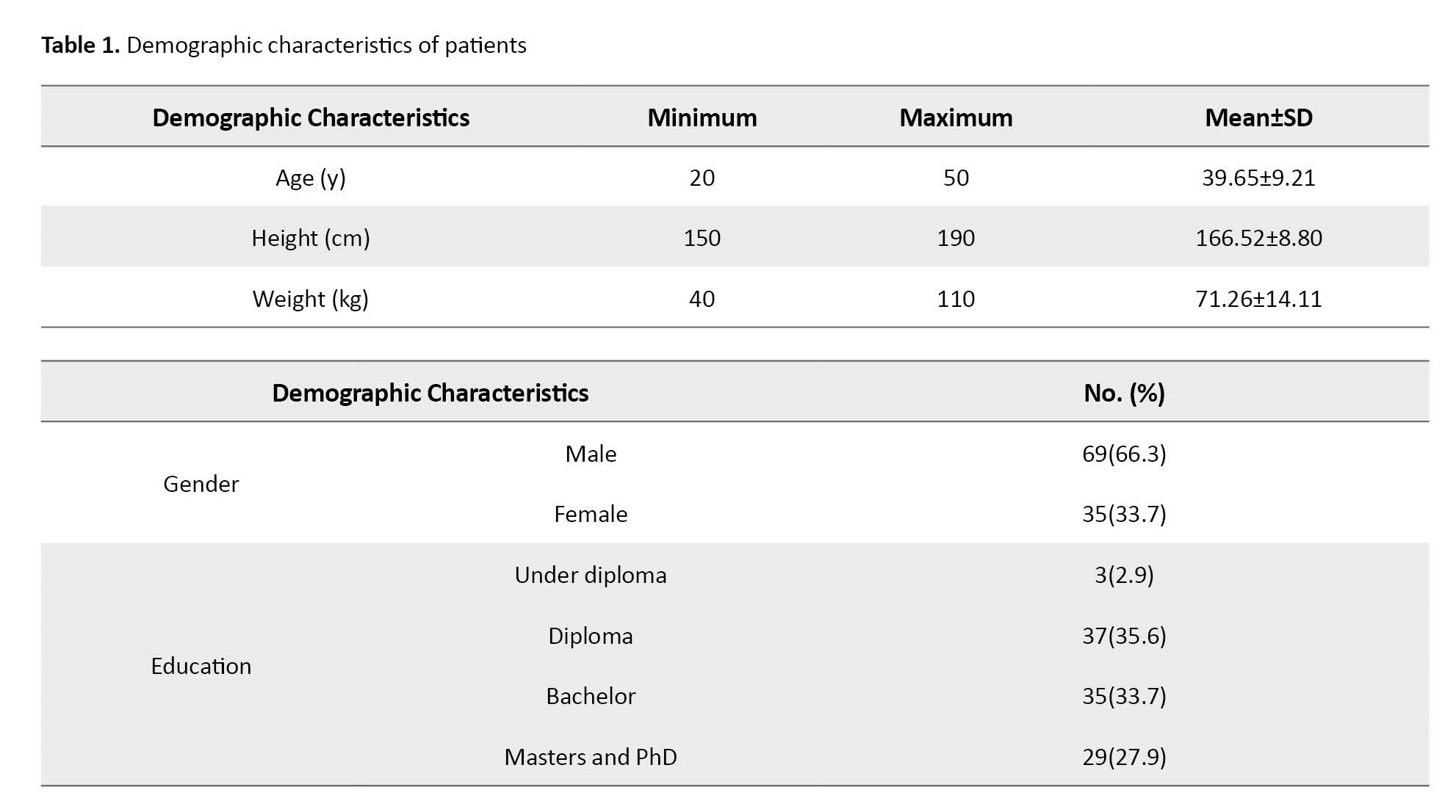
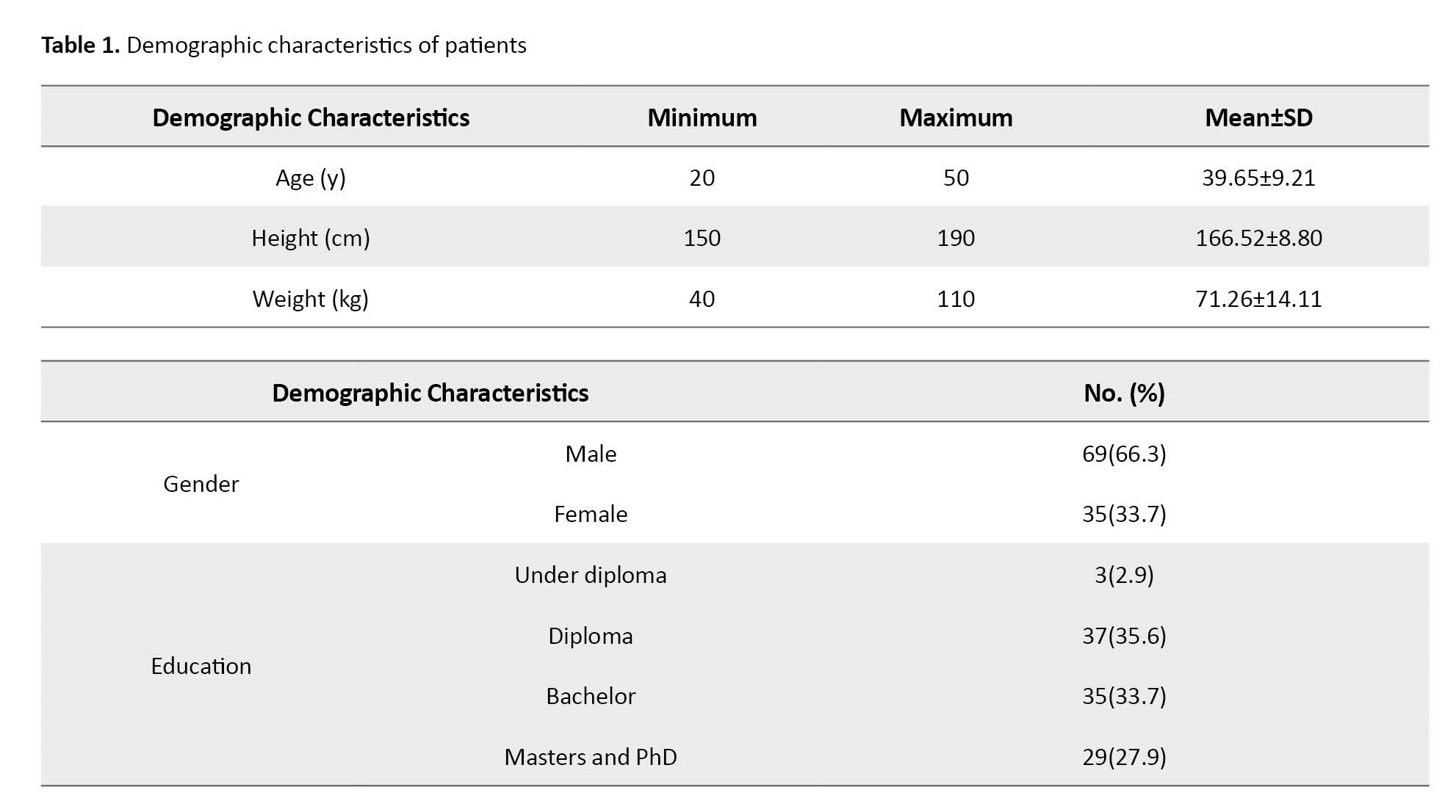
The demographic characteristics of the patients are given in Table 1.
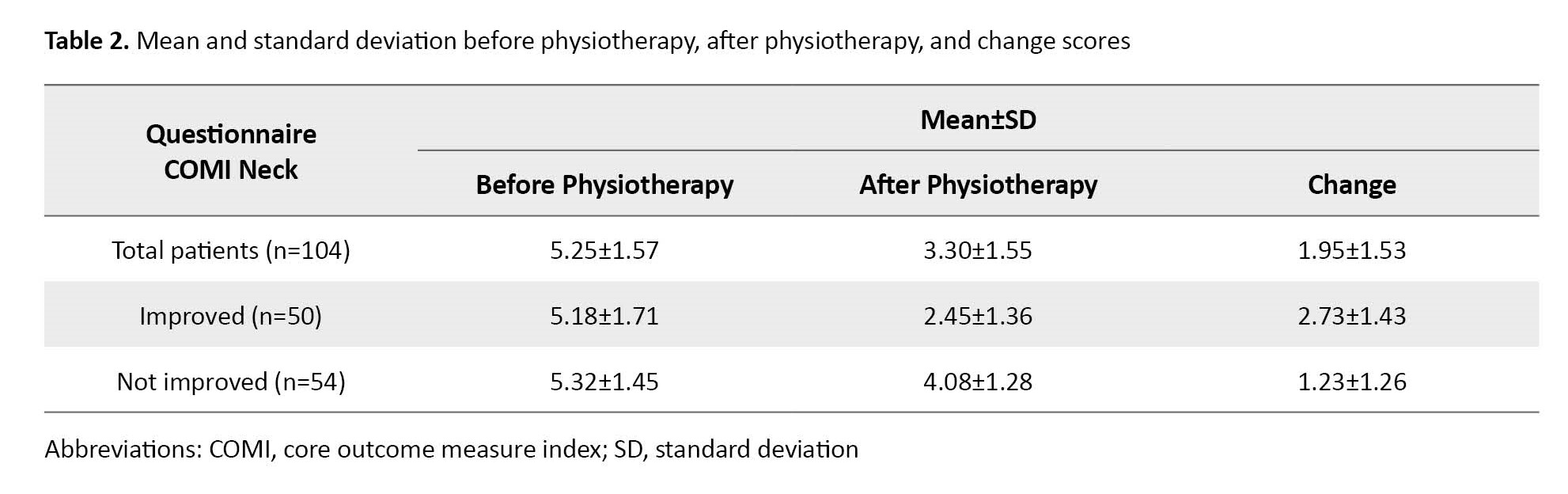
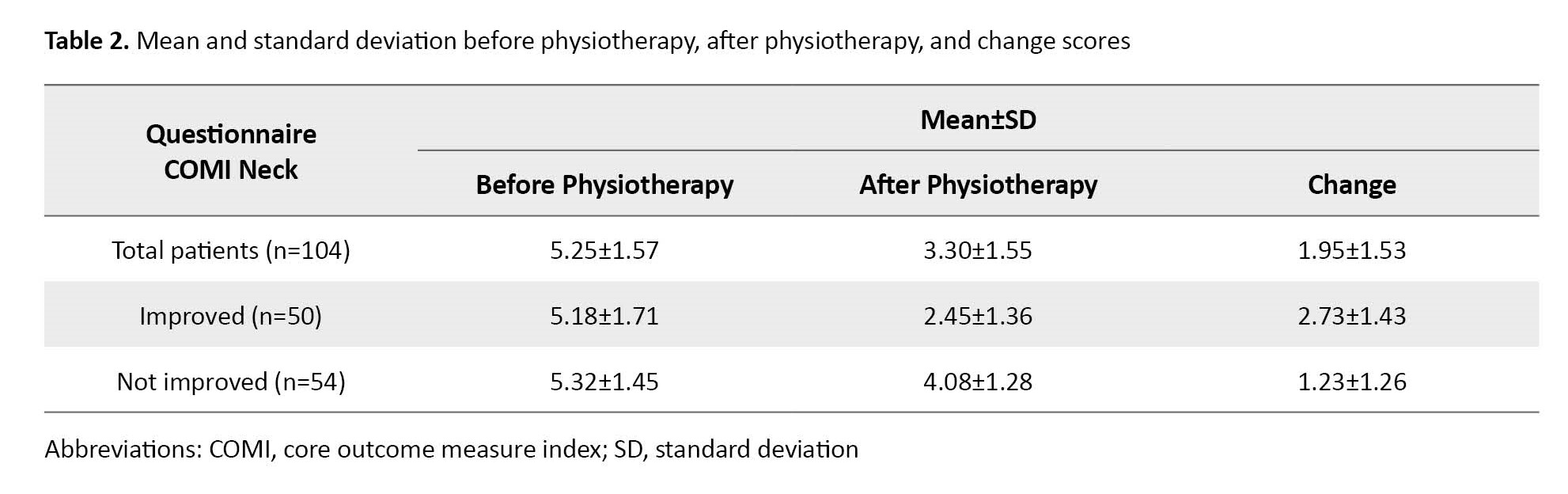
The descriptive statistics of COMI neck questionnaire scores in the first treatment session, the final session, and the change score of the COMI neck questionnaire are shown in Table 2. According to the general scale of change after physiotherapy, 10 patients (9.61%) reported that they had improved a lot, 40 patients (38.47%) had relatively improved, 34 patients (70.0%) had gotten a little better, 19 patients (18.26%) had no change, 1 patient (0.96%) had gotten a little worse, and none of the patients (0%) chose the option “I have gotten much worse”. In addition, the participants did not choose “I have become much worse”. Hence, according to the overall change scale, 50 patients (48.07%) were classified as improved and 54 patients (51.93%) were classified as not improved.
The result of the area under the ROC curve (AUC) and the gamma correlation coefficient are given in Table 3.
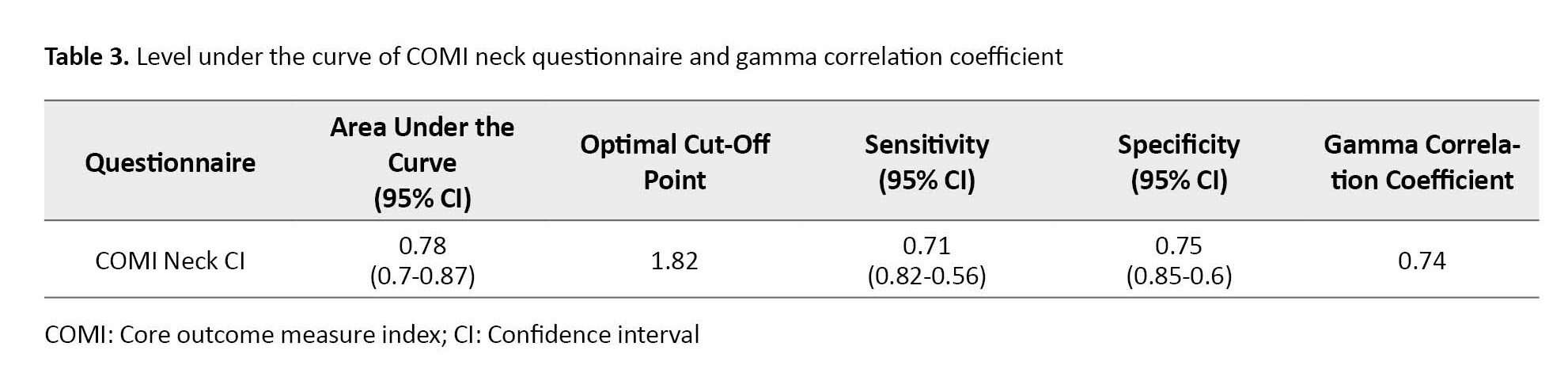
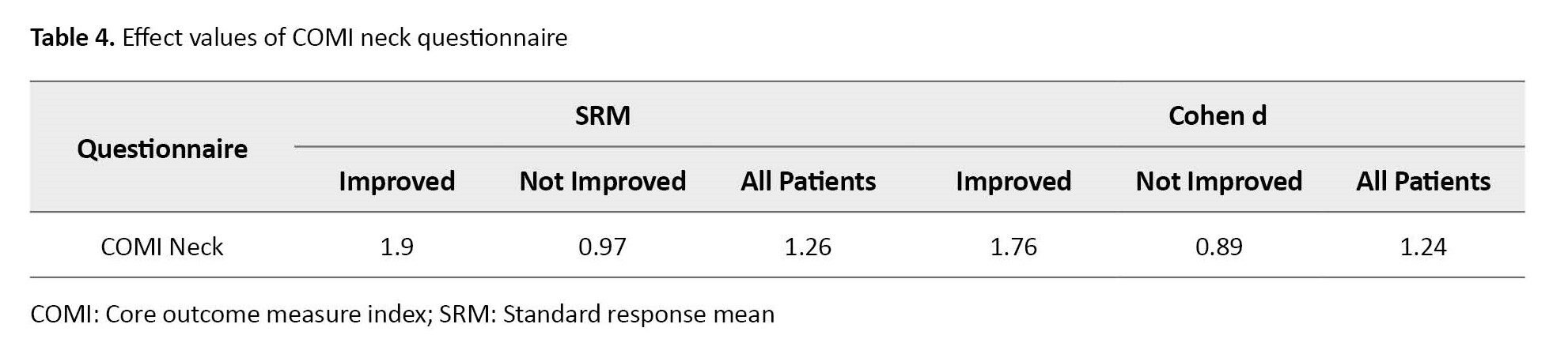
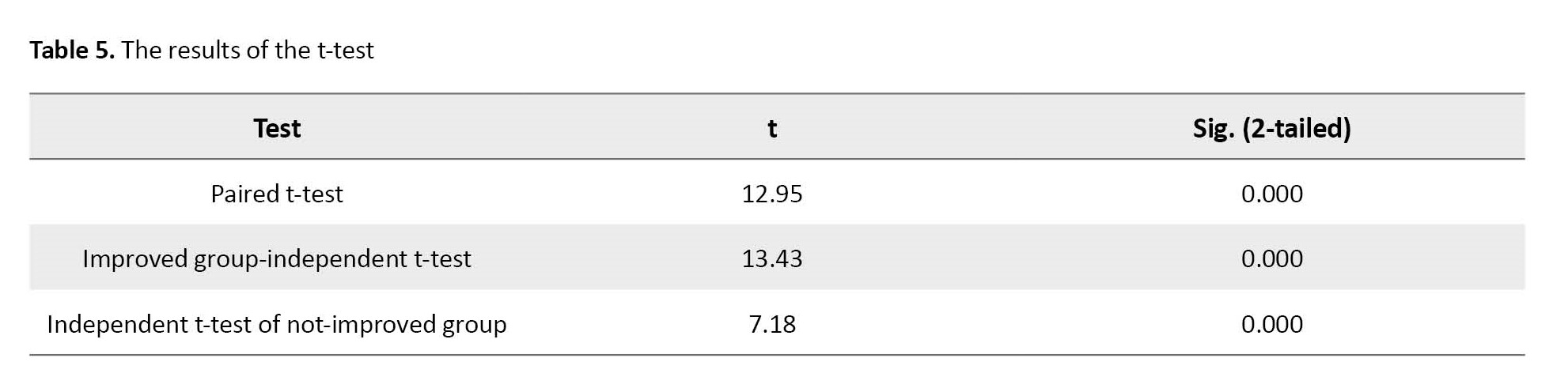
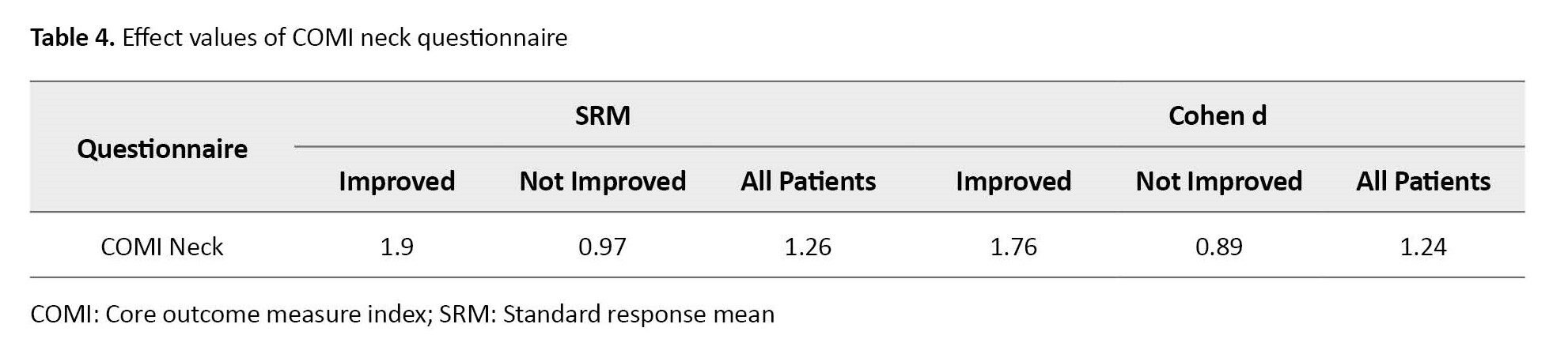
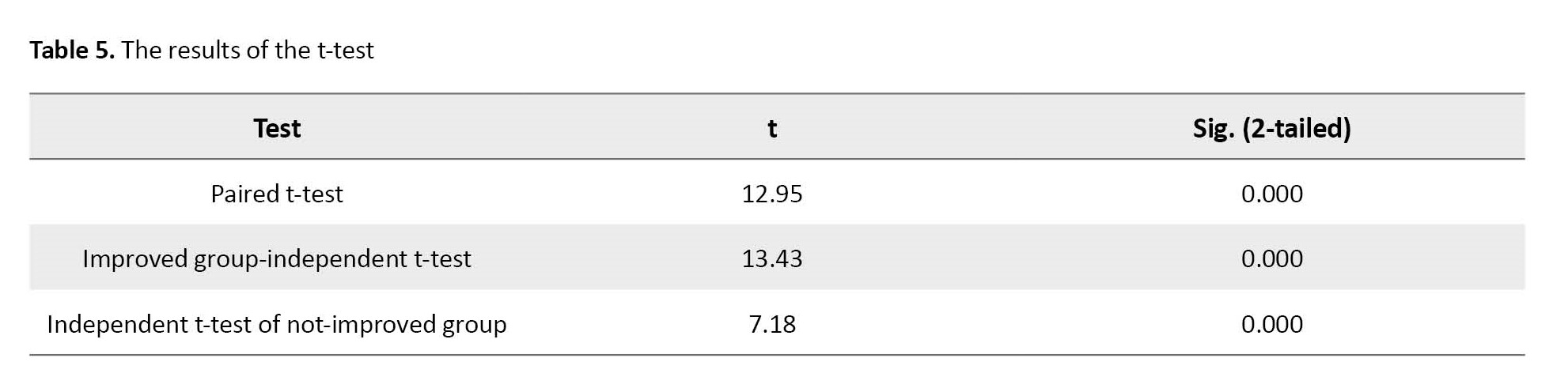
The COMI neck curve showed that the AUC value is greater than 0.78, which indicated that this questionnaire has an acceptable power to differentiate between the improved group and the non-improved group. The optimal cut point with the best combination of specificity and sensitivity for this questionnaire was 1.82 (sensitivity=0.71, specificity=0.75). Also, the results of the COMI neck questionnaire effect values and the t-test are shown in Table 4 and Table 5, respectively.
Discussion
The COMI neck questionnaire is a standard outcome measurement tool for evaluating patients with neck pain. The reliability and reproducibility of the Persian version of this questionnaire have been investigated and it has been determined that the Persian version of this questionnaire has good reliability and reproducibility in people with neck pain [23]. In this study, the responses to this questionnaire in patients with chronic neck pain have been investigated. The results of the present study showed that the Persian version of the COMI neck questionnaire has an acceptable response capability (AUC < 0.7) and a good correlation between the change score of this tool and the overall change scale was observed. In addition, the usefulness of this tool has been confirmed by determining the MCID values obtained in the present study. The results showed that the COMI neck questionnaire can be used as a criterion for choosing an appropriate outcome measurement tool in a randomized clinical trial [32]. The purpose of these studies is to evaluate and compare the effectiveness of different treatment methods; therefore, the responsiveness of outcome measurement questionnaires is important in these studies. Some researchers believe that the results obtained from tools that do not have responsiveness should be excluded from the study [26]. The results of this study showed that the Persian version of the COMI neck questionnaire can be used as a reliable tool in randomized clinical trial studies that evaluate different methods of physiotherapy treatment in patients with chronic neck pain.
The results obtained from the ROC curve method are consistent with the results of the correlation method. In the ROC method, for questionnaires to have acceptable responsiveness, they must have an area under the curve higher than 0.7, which in this study, the COMI neck questionnaire showed an area under the curve higher than 0.7 (0.78). In a similar study, Marco Monticone et al. investigated the responses to the COMI neck questionnaire in patients with chronic neck pain. They obtained an AUC value of 0.73 for the COMI neck questionnaire, which was similar to the results of the present study.
The MCID scores provide a framework for future studies of patients with neck pain. In the clinical field, it is necessary to decide on the cut-off point that can distinguish the improved from the not-improved patients [34]. For the COMI neck questionnaire, the optimal cut-off point was 1.82 with the best balance between specificity and sensitivity, that is, 0.75 and 0.71, respectively. Hence, following the results of the general evaluation scale in the COMI neck questionnaire, individuals whose score change is less than 1.82 had not changed while subjects who had a score change greater than 1.82 are considered changed people. The cut-off point of 1.82 in this questionnaire showed the lowest amount of false positives and false negatives at the same time compared to other scores, which has a probability of 0.75 to correctly identify unchanged people at this point and 0.71 is likely to correctly identify altered individuals. Therefore, the COMI neck questionnaire has an acceptable differentiation ability in identifying the change of patients in the course of the disease and follow-up treatment.
The results of the correlation coefficient showed that the Persian version of the COMI neck questionnaire has a moderate to good ability to detect clinical changes in patients with chronic neck pain following physiotherapy treatment. The correlation coefficient between the change score of the COMI neck questionnaire and the overall evaluation scale was more than 0.5(0.74).
The mean standardized response of the COMI neck questionnaire was high and the Cohen d value for this questionnaire was very high. Also, significant changes were observed between the score of the COMI neck questionnaire before and after the treatment and separately in each group.
Conclusion
Finally, the results of this study showed that the Persian version of the COMI neck questionnaire can detect clinical changes in patients with chronic neck pain after physiotherapy intervention. Therefore, we recommend this questionnaire as a tool with appropriate responsiveness to evaluate chronic neck pain patients. In addition, the MCID value obtained in this study will help therapists and researchers to know whether a Persian-speaking patient suffering from chronic neck pain has experienced a real change after physiotherapy intervention.
Study limitations
This study faced some limitations that restricted the generalizability of its results. First, the results of all the responses are specific to the same group of study patients, the type of treatment, and the method of conducting the study [35]. Therefore, the results of this study can be generalized to Persian-speaking patients with chronic neck pain who have undergone physical therapy. In this study, patient perception of change was considered a general measure of change in neck function. However, considering that the patient’s previous experiences affect their current understanding, the validity of this measure may be compromised in this study [31, 32].
Ethical Considerations
Compliance with ethical guidelines
The Ethics Committee of Iran University of Medical Sciences approved this study (Ethics Code: IR.IUMS.REC.1400.434).
Funding
The paper was extracted from the MSc. thesis of Seyyed Shahab Mirhajian entitled "Investigation of the responsiveness of the Persian version of the COMI Neck questionnaire in people with non-specific chronic neck pain" and presented at Department of physiotherapy, Faculty of rehabilitation science, Iran University of Medical Sciences in Tehran.
Authors' contributions
Conceptualization, supervision: Soheil Mansour Sohani; Methodology: Reza Salehi; Investigation,Writing–review & editing: All authors; Writing-original draft: Seyyed Shahab Mirhajian; Funding acquisition, Resources: Seyyed Shahab Mirhajian and Soheil Mansour Sohani.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We would like to thank all the participants in this study, and all the people who helped us in this study.
References
Neck pain is one of the most common musculoskeletal problems following low back pain; hence, it is considered one of the causes of disability in the population [1]. The prevalence of neck pain is between 30% to 50% per year. Based on the duration of the symptoms, neck pain is divided into two groups, namely acute and chronic. When neck pain continues for more than 12 weeks, it is defined as chronic neck pain [2]. According to the Global Burden of Disease Study 2010, neck pain is the fourth leading cause of years lost due to disability after low back pain, depression, and joint pain [3]. The occurrence of neck pain is more common in women compared to men and among middle-aged people [4]. Genetics, psychological factors, sleep disorders, smoking, and a sedentary lifestyle are the variables of the causative factors related to neck pain [2, 5, 6].
Evaluation is always considered an important part of any therapeutic intervention [7] because, in addition to considering pathology and its physical aspects, therapists should consider the contribution of psychological factors in the occurrence of long-term disability in people with neck pain [8]. In recent years, self-report measurement tools have played a very important role in measuring health outcomes in spine-related diseases, thus helping the treatment process of patients [9]. The results of the studies showed that the evaluation of the consequences is the best criterion for evaluating chronic pain in affected people; therefore, it is necessary to evaluate the impact of chronic disorders on individuals’ health as well as the results of therapeutic interventions [7]. Among these outcome-based tools, we can mention the neck disability index, the North American spine society questionnaire, the Copenhagen neck functional disability scale, the Northwick Park neck pain questionnaire, the neck pain and disability scale, and the core outcome measure index [10-14].
In evaluating these patients, it is recommended to evaluate the following 5 dimensions: pain, function, well-being, disability at work, and disability in society [15]. During the last two decades, a large number of these questionnaires have been compiled; however, none of these tools can fully evaluate the consequences of chronic disorders correctly [16]. In addition, these tools cannot evaluate different dimensions of the outcome; therefore, a standard set of tools is needed to evaluate the different outcomes of disorders [15]. For this purpose, in 1998, a group of researchers developed a standard outcome measurement tool called the core outcome measure index (COMI) for patients with low back pain. COMI includes 5 areas as follows: pain, function, general health conditions, disability, and satisfaction [9, 15]. The COMI questionnaire has been registered with the European Spine Association to measure the outcome following spine surgery and non-surgical treatments and is currently used worldwide [17]. The psychometric properties of COMI were evaluated and the results showed acceptable validity and reliability of the questionnaire [16]. The COMI neck questionnaire was compiled and used as a supplement to COMI back to evaluate chronic neck pain patients and patients who underwent neck arthroplasty surgery [18, 19]. This reliable tool has been translated and localized into Turkish, Polish, Italian, Persian, and Japanese languages [20-24].
Responsiveness is an essential psychometric feature of an instrument and describes the ability of an instrument to show a clinically significant change in a patient’s health status over time [25]. From a clinical perspective, an outcome measure with response characteristics should be able to differentiate between treatment effects and random and spontaneous changes [26]. The measurement tool should be able to show real changes for better or worse. The reliability and reproducibility of the Persian version of the COMI neck questionnaire have been investigated and determined that the Persian version of this questionnaire has good reliability and reproducibility in people with neck pain; however, the ability of this questionnaire to respond to treatment has not been investigated. Therefore, this study aims to investigate the responsiveness of the Persian version of the COMI neck questionnaire and to determine the minimum clinically important change scores in patients with chronic neck pain after a course of physiotherapy treatment.
Materials and Methods
Study participants
A total of 104 patients who were referred to physiotherapy because of being diagnosed with chronic neck pain participated in this study by filling out the informed consent form. The diagnosis of chronic neck pain was made by an orthopedic through clinical examination and radiological findings. The inclusion criteria were as follows: age range between 18 and 50 years, ability to read and write and understand the Persian language, non-specific neck pain for more than 3 months, minimum education at the level of high school, and undergoing a course of physiotherapy treatment [18, 23, 27]. Also, the exclusion criteria were having neck pain due to deformity, fracture, spinal canal stenosis of the cervical vertebra, the presence of central or peripheral nervous system disease, systemic diseases, the use of strong painkillers during the period of physiotherapy treatment, or any other concurrent treatment, mental and cognitive diseases, chronic lung or kidney diseases, and a recent history of stroke or heart attack [18, 23, 27].
Study design
This study was based on a prospective cohort design. All patients received and completed the Persian version of the COMI neck questionnaire before the first session of physiotherapy treatment. The physiotherapy program included electrotherapy (TENS, US. hot pack), range of motion exercises, deep neck muscle strengthening, stabilization exercises, soft tissue stretching, and cervical facet joint mobilization. It was not necessary to use the same protocol in all clinics because the purpose of this plan was not to evaluate the protocol but to evaluate the ability to respond to treatment [28, 29]. After 10 treatment sessions, the subjects were re-evaluated and the Persian version of the COMI neck questionnaire was completed again by the patients. In addition to completing the mentioned questionnaire, the patients received and completed the global rating of change (GRC) questionnaire in the final session of the treatment.
Outcome measures
The COMI questionnaire includes 7 questions as follows: 2 questions related to pain, 1 question related to function, 1 question related to well-being, 2 questions related to disability, and 1 question related to satisfaction. The COMI neck questionnaire is designed based on a 10-question graphic scale, and the scores are calculated as follows: a score of 0 indicates the best condition and a score of 10 indicates the worst condition in patients [15, 18].
Assessment tool
The GRC questionnaire is a valid tool that has been used as a reference tool in most of the studies whose purpose was to check the response. This scale includes the question of how much the patient has changed compared to the first day of the visit. The rating of this scale is as follows: “7=I have improved a lot”, “6=I have improved relatively”, “5=I have improved a little”, “4=I have not changed”, “3=I have gotten a little worse”, “2=I have become much worse”, “1=I have become much worse”.
Statistical analysis
The data obtained in this study were analyzed using the SPSS software, version 26. The level of statistical significance was considered P<0.05. To measure responsiveness, the change in scores between the first and last sessions for the COMI neck questionnaire was calculated. The change score was obtained by subtracting the score of the first session from the score of the last session; therefore, a positive score indicated improvement and a negative score indicated worsening of the patient’s condition [30]. In this study, responsiveness was calculated using 2 methods as follows: the receiver operating characteristic (ROC) curve method and the correlation calculation. The ROC curve is the most common method for calculating responsiveness and uses the overall scale of change as an external measure [31]. Functional scales can be considered a diagnostic test to differentiate between patients who have recovered from patients who have not recovered, considering that the ROC curve has been developed to detect recovery or non-recovery using an external criterion. Evaluating the responsiveness of functional scales is similar to evaluating the discrimination capability of a diagnostic test. In this case, the condition to be determined is whether a clinically significant change has occurred. Functional scale scores, similar to other diagnostic tests, may show random changes over time and can never be flawless measurements, and there are “true positive” and “false positive” changes in the scale scores. Functionality happens over time; therefore, one of the ways to evaluate responsiveness is to calculate the sensitivity and specificity of the scales to determine improvement or deterioration. The ROC curve provides information about the sensitivity and specificity for detecting improvement by an external measure. This curve includes a graph of the true positive rate (sensitivity) versus the false positive rate (specificity-1) for each of the possible cut points in the change score [31, 32]. Sensitivity means the ability of a tool to identify a clinical change when a change exists. Specificity means the ability of a tool to identify the lack of clinical change when no change exists [31].
The area under the ROC curve can be interpreted as the probability of correctly identifying a cured patient from a pair of cured and uncured patients that are randomly selected. It is also more for distinguishing between the two groups of improved and non-improved patients that are determined by external criteria [31, 32]. The range of this area is theoretically from 0 (no accuracy in differentiating the improved group from the unimproved group) to 1 (complete and excellent accuracy). The area under the curve value greater than 0.7 indicates high responsiveness [33].
One of the cut points obtained from the ROC curve is the minimal clinically important difference (MCID). MCID is the number of scores required to show a clinically significant change [31]. In this study, the best cut point was chosen as the change score in the COMI neck questionnaire, which indicates a clinical change in the patient’s functional ability [31]. The best method for detecting MCID is ROC; the point of the ROC curve that is closer to the upper and left corner of the diagram is used to estimate the minimum change score necessary to distinguish improved from non-improved patients [34]. This appropriate cut-off point is the point that has the highest sensitivity and specificity along with the ability to differentiate between improved and non-improved patients [33].
Responsiveness is also obtained by calculating the correlation between the change score of the COMI neck questionnaire and the overall change criterion using the gamma correlation coefficient. According to the numerical information of the general scale of change, we used the gamma correlation coefficient to determine the relationship between the scores of the COMI neck questionnaire and the score of the patient’s general scale of change. In this method, the strength of correlation indicates responsiveness. The correlation coefficients less than 0.25, 0.25 to 0.5, 0.5 to 0.75, and more than 0.75, respectively, indicate no or little connection, weak connection, medium to good connection, and connection it is good to excellent [31].
Results
The demographic characteristics of the patients are given in Table 1.
The descriptive statistics of COMI neck questionnaire scores in the first treatment session, the final session, and the change score of the COMI neck questionnaire are shown in Table 2. According to the general scale of change after physiotherapy, 10 patients (9.61%) reported that they had improved a lot, 40 patients (38.47%) had relatively improved, 34 patients (70.0%) had gotten a little better, 19 patients (18.26%) had no change, 1 patient (0.96%) had gotten a little worse, and none of the patients (0%) chose the option “I have gotten much worse”. In addition, the participants did not choose “I have become much worse”. Hence, according to the overall change scale, 50 patients (48.07%) were classified as improved and 54 patients (51.93%) were classified as not improved.
The result of the area under the ROC curve (AUC) and the gamma correlation coefficient are given in Table 3.
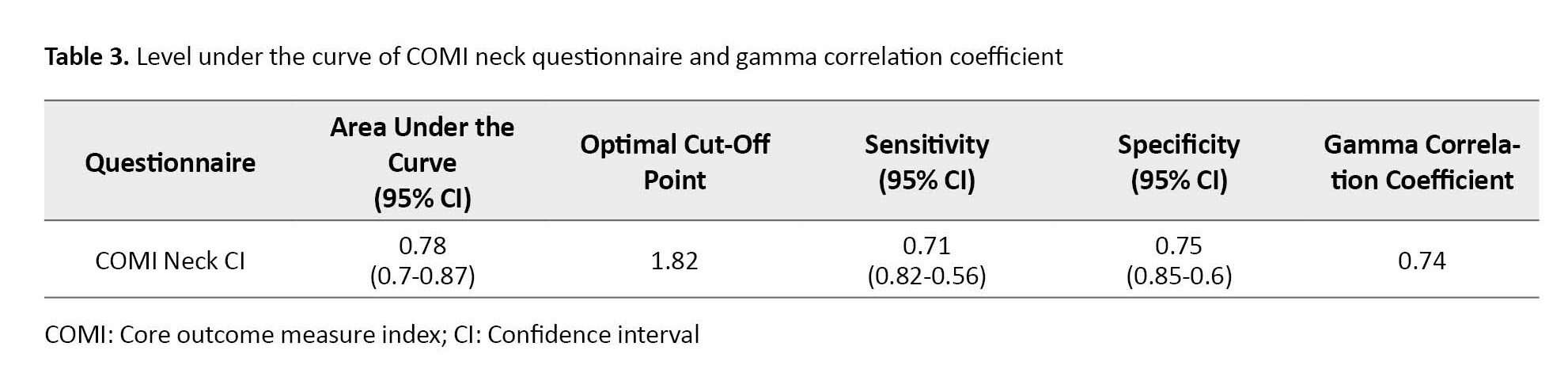
The COMI neck curve showed that the AUC value is greater than 0.78, which indicated that this questionnaire has an acceptable power to differentiate between the improved group and the non-improved group. The optimal cut point with the best combination of specificity and sensitivity for this questionnaire was 1.82 (sensitivity=0.71, specificity=0.75). Also, the results of the COMI neck questionnaire effect values and the t-test are shown in Table 4 and Table 5, respectively.
Discussion
The COMI neck questionnaire is a standard outcome measurement tool for evaluating patients with neck pain. The reliability and reproducibility of the Persian version of this questionnaire have been investigated and it has been determined that the Persian version of this questionnaire has good reliability and reproducibility in people with neck pain [23]. In this study, the responses to this questionnaire in patients with chronic neck pain have been investigated. The results of the present study showed that the Persian version of the COMI neck questionnaire has an acceptable response capability (AUC < 0.7) and a good correlation between the change score of this tool and the overall change scale was observed. In addition, the usefulness of this tool has been confirmed by determining the MCID values obtained in the present study. The results showed that the COMI neck questionnaire can be used as a criterion for choosing an appropriate outcome measurement tool in a randomized clinical trial [32]. The purpose of these studies is to evaluate and compare the effectiveness of different treatment methods; therefore, the responsiveness of outcome measurement questionnaires is important in these studies. Some researchers believe that the results obtained from tools that do not have responsiveness should be excluded from the study [26]. The results of this study showed that the Persian version of the COMI neck questionnaire can be used as a reliable tool in randomized clinical trial studies that evaluate different methods of physiotherapy treatment in patients with chronic neck pain.
The results obtained from the ROC curve method are consistent with the results of the correlation method. In the ROC method, for questionnaires to have acceptable responsiveness, they must have an area under the curve higher than 0.7, which in this study, the COMI neck questionnaire showed an area under the curve higher than 0.7 (0.78). In a similar study, Marco Monticone et al. investigated the responses to the COMI neck questionnaire in patients with chronic neck pain. They obtained an AUC value of 0.73 for the COMI neck questionnaire, which was similar to the results of the present study.
The MCID scores provide a framework for future studies of patients with neck pain. In the clinical field, it is necessary to decide on the cut-off point that can distinguish the improved from the not-improved patients [34]. For the COMI neck questionnaire, the optimal cut-off point was 1.82 with the best balance between specificity and sensitivity, that is, 0.75 and 0.71, respectively. Hence, following the results of the general evaluation scale in the COMI neck questionnaire, individuals whose score change is less than 1.82 had not changed while subjects who had a score change greater than 1.82 are considered changed people. The cut-off point of 1.82 in this questionnaire showed the lowest amount of false positives and false negatives at the same time compared to other scores, which has a probability of 0.75 to correctly identify unchanged people at this point and 0.71 is likely to correctly identify altered individuals. Therefore, the COMI neck questionnaire has an acceptable differentiation ability in identifying the change of patients in the course of the disease and follow-up treatment.
The results of the correlation coefficient showed that the Persian version of the COMI neck questionnaire has a moderate to good ability to detect clinical changes in patients with chronic neck pain following physiotherapy treatment. The correlation coefficient between the change score of the COMI neck questionnaire and the overall evaluation scale was more than 0.5(0.74).
The mean standardized response of the COMI neck questionnaire was high and the Cohen d value for this questionnaire was very high. Also, significant changes were observed between the score of the COMI neck questionnaire before and after the treatment and separately in each group.
Conclusion
Finally, the results of this study showed that the Persian version of the COMI neck questionnaire can detect clinical changes in patients with chronic neck pain after physiotherapy intervention. Therefore, we recommend this questionnaire as a tool with appropriate responsiveness to evaluate chronic neck pain patients. In addition, the MCID value obtained in this study will help therapists and researchers to know whether a Persian-speaking patient suffering from chronic neck pain has experienced a real change after physiotherapy intervention.
Study limitations
This study faced some limitations that restricted the generalizability of its results. First, the results of all the responses are specific to the same group of study patients, the type of treatment, and the method of conducting the study [35]. Therefore, the results of this study can be generalized to Persian-speaking patients with chronic neck pain who have undergone physical therapy. In this study, patient perception of change was considered a general measure of change in neck function. However, considering that the patient’s previous experiences affect their current understanding, the validity of this measure may be compromised in this study [31, 32].
Ethical Considerations
Compliance with ethical guidelines
The Ethics Committee of Iran University of Medical Sciences approved this study (Ethics Code: IR.IUMS.REC.1400.434).
Funding
The paper was extracted from the MSc. thesis of Seyyed Shahab Mirhajian entitled "Investigation of the responsiveness of the Persian version of the COMI Neck questionnaire in people with non-specific chronic neck pain" and presented at Department of physiotherapy, Faculty of rehabilitation science, Iran University of Medical Sciences in Tehran.
Authors' contributions
Conceptualization, supervision: Soheil Mansour Sohani; Methodology: Reza Salehi; Investigation,Writing–review & editing: All authors; Writing-original draft: Seyyed Shahab Mirhajian; Funding acquisition, Resources: Seyyed Shahab Mirhajian and Soheil Mansour Sohani.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We would like to thank all the participants in this study, and all the people who helped us in this study.
References
- Ferrari R, Russell AS. Regional musculoskeletal conditions: Neck pain. Best Pract Res Clin Rheumatol. 2003; 17(1):57-70. [DOI:10.1016/S1521-6942(02)00097-9] [PMID]
- Hogg-Johnson S, van der Velde G, Carroll LJ, Holm LW, Cassidy JD, Guzman J, et al. The burden and determinants of neck pain in the general population: Results of the bone and joint decade 2000-2010 task force on neck pain and its associated disorders. J Manip Physiol Ther. 2009; 32(S 2):S46-60. [doi:10.1016/j.jmpt.2008.11.010]
- Cohen SP. Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin Proc. 2015; 90(2):284-99. [DOI:10.1016/j.mayocp.2014.09.008] [PMID]
- Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: A systematic critical review of the literature. Eur Spine J. 2006; 15(6):834-48. [DOI:10.1007/s00586-004-0864-4] [PMID] [PMCID]
- Kääriä S, Laaksonen M, Rahkonen O, Lahelma E, Leino-Arjas P. Risk factors of chronic neck pain: A prospective study among middle-aged employees. Eur J Pain. 2012; 16(6):911-20. [DOI:10.1002/j.1532-2149.2011.00065.x] [PMID]
- Strine TW, Hootman JM. US national prevalence and correlates of low back and neck pain among adults. Arthritis Rheum. 2007; 57(4):656-65. [DOI:10.1002/art.22684] [PMID]
- Slevin ML, Plant H, Lynch Da, Drinkwater J, Gregory W. Who should measure quality of life, the doctor or the patient? Br J Cancer. 1988; 57(1):109-12. [DOI:10.1038/bjc.1988.20] [PMID] [PMCID]
- Walton DM, Carroll LJ, Kasch H, Sterling M, Verhagen AP, MacDermid JC, et al. An overview of systematic reviews on prognostic factors in neck pain: Results from the International Collaboration on Neck Pain (ICON) project. Open Orthop J. 2013; 7:494-505. [DOI:10.2174/1874325001307010494] [PMID] [PMCID]
- Bombardier C. Outcome assessments in the evaluation of treatment of spinal disorders: Summary and general recommendations. Spine. 2000; 25(24):3100-3. [DOI:10.1097/00007632-200012150-00003] [PMID]
- Jordan A, Manniche C, Mosdal C, Hindsberger C. The copenhagen neck functional disability scale: A study of reliability and validity. J Manipulative Physiol Ther. 1998; 21(8):520-7. [PMID]
- Leak A, Cooper J, Dyer S, Williams K, Turner-Stokes L, Frank A. The northwick park neck pain questionnaire, devised to measure neck pain and disability. Br J Rheumatol. 1994; 33(5):469-74. [DOI:10.1093/rheumatology/33.5.469] [PMID]
- Stoll T, Huber E, Bachmann S, Baumeler H-R, Mariacher S, Rutz M, et al. Validity and sensitivity to change of the NASS questionnaire for patients with cervical spine disorders. Spine. 2004; 29(24):2851-5. [DOI:10.1097/01.brs.0000147802.57484.77] [PMID]
- Vernon H, Mior S. The neck disability index: A study of reliability and validity. J Manipulative Physiol Ther. 1991; 14(7):409-15. [DOI:10.1037/t35122-000]
- Wheeler AH, Goolkasian P, Baird AC, Darden BV. Development of the neck pain and disability scale: Item analysis, face, and criterion-related validity. Spine. 1999; 24(13):1290-4. [DOI:10.1097/00007632-199907010-00004] [PMID]
- Deyo RA, Battie M, Beurskens A, Bombardier C, Croft P, Koes B, et al. Outcome measures for low back pain research: A proposal for standardized use. Spine. 1998; 23(18):2003-13. [DOI:10.1097/00007632-199809150-00018] [PMID]
- Miekisiak G, Kollataj M, Dobrogowski J, Kloc W, Libionka W, Banach M, et al. Validation and cross-cultural adaptation of the polish version of the oswestry disability index. Spine. 2013; 38(4):E237-43. [DOI:10.1097/BRS.0b013e31827e948b] [PMID]
- Zweig T, Mannion AF, Grob D, Melloh M, Munting E, Tuschel A, et al. How to Tango: A manual for implementing Spine Tango. Eur Spine J. 2009; 18(S 3):312-20. [DOI:10.1007/s00586-009-1074-x] [PMID] [PMCID]
- Fankhauser CD, Mutter U, Aghayev E, Mannion AF. Validity and responsiveness of the Core Outcome Measures Index (COMI) for the neck. Eur Spine J. 2012; 21(1):101-14. [DOI:10.1007/s00586-011-1921-4] [PMID] [PMCID]
- White P, Lewith G, Prescott P. The core outcomes for neck pain: Validation of a new outcome measure. Spine. 2004; 29(17):1923-30. [DOI:10.1097/01.brs.0000137066.50291.da] [PMID]
- Karabicak GO, Kanik ZH, Gunaydin G, Pala OO, Citaker S. Reliability and validity of the Turkish version of the core outcome measures index for the neck pain. Eur Spine J. 2020; 29(1):186-93. [DOI:10.1007/s00586-019-06169-w] [PMID]
- Miekisiak G, Banach M, Kiwic G, Kubaszewski L, Kaczmarczyk J, Sulewski A, et al. Reliability and validity of the Polish version of the Core Outcome Measures Index for the neck. Eur Spine J. 2014; 23(4):898-903. [DOI:10.1007/s00586-013-3129-2] [PMID] [PMCID]
- Monticone M, Baiardi P, Nido N, Righini C, Tomba A, Giovanazzi E. Development of the Italian version of the neck pain and disability scale, NPDS-I: Cross-cultural adaptation, reliability, and validity. Spine. 2008; 33(13):E429-34. [DOI:10.1097/BRS.0b013e318175c2b0] [PMID]
- Rafatifard M, Shahali S, Mansour Sohani S. Validity and reliability of Persian version of COMI-neck questionnaire in Iranian patients with chronic neck pain. Func Disabil J. 2018; 1(2):57-64. [DOI:10.30699/fdisj.1.2.57]
- Kirshner B, Guyatt G. A methodological framework for assessing health indices. J Chronic Dis. 1985; 38(1):27-36. [DOI:10.1016/0021-9681(85)90005-0] [PMID]
- Staples MP, Forbes A, Green S, Buchbinder R. Shoulder-specific disability measures showed acceptable construct validity and responsiveness. J Clin Epidemiol. 2010; 63(2):163-70. [DOI:10.1016/j.jclinepi.2009.03.023] [PMID]
- Monticone M, Ferrante S, Maggioni S, Grenat G, Checchia GA, Testa M, et al. Reliability, validity and responsiveness of the cross-culturally adapted Italian version of the core outcome measures index (COMI) for the neck. Eur Spine J. 2014; 23(4):863-72. [DOI:10.1007/s00586-013-3092-y] [PMID] [PMCID]
- Kaslow RA, Ostrow DG, Detels R, Phair JP, Polk BF, Rinaldo Jr CR. The multicenter AIDS cohort study: Rationale, organization, and selected characteristics of the participants. Am J Epidemiol. 1987; 126(2):310-8. [DOI:10.1093/aje/126.2.310] [PMID]
- Salehi R, Negahban H, Saghayezhian N, Saadat M. The responsiveness of the Persian version of Neck Disability Index and Functional Rating Index following physiotherapy intervention in people with chronic neck pain. Iran J Med Sci. 2019; 44(5):390-6. [doi:10.30476/ijms.2019.44963]
- De Vet HC, Bouter LM, Bezemer PD, Beurskens AJ. Reproducibility and responsiveness of evaluative outcome measures: theoretical considerations illustrated by an empirical example. Int J Technol Assess Health Care. 2001; 17(4):479-87. [DOI:10.1017/S0266462301107038] [PMID]
- Lehman LA, Velozo CA. Ability to detect change in patient function: responsiveness designs and methods of calculation. J Hand Ther. 2010; 23(4):361-71. [DOI:10.1016/j.jht.2010.05.003] [PMID]
- Husted JA, Cook RJ, Farewell VT, Gladman DD. Methods for assessing responsiveness: a critical review and recommendations. J Clin Epidemiol. 2000; 53(5):459-68. [DOI:10.1016/S0895-4356(99)00206-1] [PMID]
- Deyo RA, Centor RM. Assessing the responsiveness of functional scales to clinical change: an analogy to diagnostic test performance. J Chronic Dis. 1986; 39(11):897-906. [DOI:10.1016/0021-9681(86)90038-X] [PMID]
- Stratford PW, Binkley JM, Riddle DL. Health status measures: strategies and analytic methods for assessing change scores. Phys Ther. 1996; 76(10):1109-23. [DOI:10.1093/ptj/76.10.1109] [PMID]
- Tveitå EK, Ekeberg OM, Juel NG, Bautz-Holter E. Responsiveness of the shoulder pain and disability index in patients with adhesive capsulitis. BMC Musculoskelet Disord. 2008; 9:161.[DOI:10.1186/1471-2474-9-161] [PMID] [PMCID]
- Oshima Y, Nagata K, Nakamoto H, Sakamoto R, Takeshita Y, Ohtomo N, et al. Validity of the Japanese core outcome measures index (COMI)-neck for cervical spine surgery: a prospective cohort study. Eur Spine J. 2021; 30(2):402-9. [DOI:10.1007/s00586-020-06657-4] [PMID]
Type of Study: Research |
Subject:
Physiotherapy
Received: 2023/02/5 | Accepted: 2023/03/4 | Published: 2022/02/3
Received: 2023/02/5 | Accepted: 2023/03/4 | Published: 2022/02/3