Volume 5, Issue 1 (Continuously Updated 2022)
Func Disabil J 2022, 5(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Keshavarzi M H, Nahardani S Z, Jalali M, Pashmdarfard M. Educational Factors in Evidence-based Rehabilitation: A Qualitative Study in Iran. Func Disabil J 2022; 5 (1) : 58
URL: http://fdj.iums.ac.ir/article-1-190-en.html
URL: http://fdj.iums.ac.ir/article-1-190-en.html
1- Department of Medical Education, Clinical Educational Center, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran.
2- Rehabilitation Research Center, Iran University of Medical Sciences, Tehran, Iran.
3- Department of Orthotics and Prosthetics, Rehabilitation Research Center, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
4- Department of Occupational Therapy, Physiotherapy Research Center, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran. ,mpashmdarfard@gmail.com
2- Rehabilitation Research Center, Iran University of Medical Sciences, Tehran, Iran.
3- Department of Orthotics and Prosthetics, Rehabilitation Research Center, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
4- Department of Occupational Therapy, Physiotherapy Research Center, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 1072 kb]
(476 Downloads)
| Abstract (HTML) (1401 Views)
Full-Text: (512 Views)
Introduction
The development and reform in training require an understanding of the education process, modern methods of implementation, recognition of financial resources and facilities, and awareness of the role and duties of human resources. The inability to properly plan to utilize the skills needed by the learners, such as clinical reasoning, problem-solving and critical thinking has made it necessary to keep up with the recent developments in the field [1, 2].
Evidence-based therapy is a systematic process that involves finding, analyzing, and utilizing the best scientific research to help make scientific reasoning. This process begins with designing a clinical question, continuing with the search for relevant resources, and evaluating its credibility, validity, reliability, and usefulness, which ends with the implementation of clinical research findings and evaluating treatment effectiveness [3].
Evidence-based practice (EBP) individualizes healthcare decision-making and service delivery by “the conscientious, explicit, judicious and reasonable use of the best available evidence”, integrating clinical expertise, and patient values and preferences with the best available research information” [4, 5]. EBP has many benefits, such as making services more effective for each individual, more responsive to clients and their families, providing equal treatment to clients based on scientific evidence, up-to-date therapists, improving the quality of service, enhancing professional credibility, encouraging adherence to ethical principles, promoting interdisciplinary collaboration and communication, encouraging continued learning, promoting service delivery, more appropriate clinical decision-making, establishing appropriate communication between research and clinical services, and the need to use it in many health [6, 7].
In Iran, many efforts have been made to improve rehabilitation services to play a more constructive role in the health system [8]. In addition, the use of EBP does not ignore the clinicians’ experiences; rather it considers these experiences necessary to integrate with scientific evidence and patients’ needs [9] which are of great importance in the rehabilitation field. Therefore, rehabilitation specialists can properly improve the level of service delivery and provide healthier, more qualified, shorter, more effective, reasonable, accurate, and patient-oriented treatments [10].
Much research has been conducted on EBP in rehabilitation fields in different countries [11]. Most of the literature published in the last two decades and along with the emergence and expansion of EBP in the field of rehabilitation sciences were published by scholars of this field and have attempted to promote this process and introduce its benefits of it [6, 7, 12].
Most of these studies have been conducted using a quantitative method, and have largely examined the therapists’ knowledge, attitude, and practice toward EBP [11, 13]. In this study, general documents for other professions have been used. While each discipline has its particular conditions that can influence the intake of EBP, cultural conditions are also influential in this regard [14]. Considering the importance of EBP in rehabilitation sciences and meeting the community’s needs, this study aimed to explain the effective educational factors in adopting EBP in the fields of rehabilitation sciences.
Materials and Methods
This study used inductive qualitative content analysis to interpret subjective data scientifically, encode data through a regular process, and identify themes and patterns [15, 16]. All interviews were tape-recorded and then transcribed and analyzed. All principles of informed consent, anonymity, confidentiality, the right to withdraw from participation at any time, and ethical obligations were fully observed in the present research.
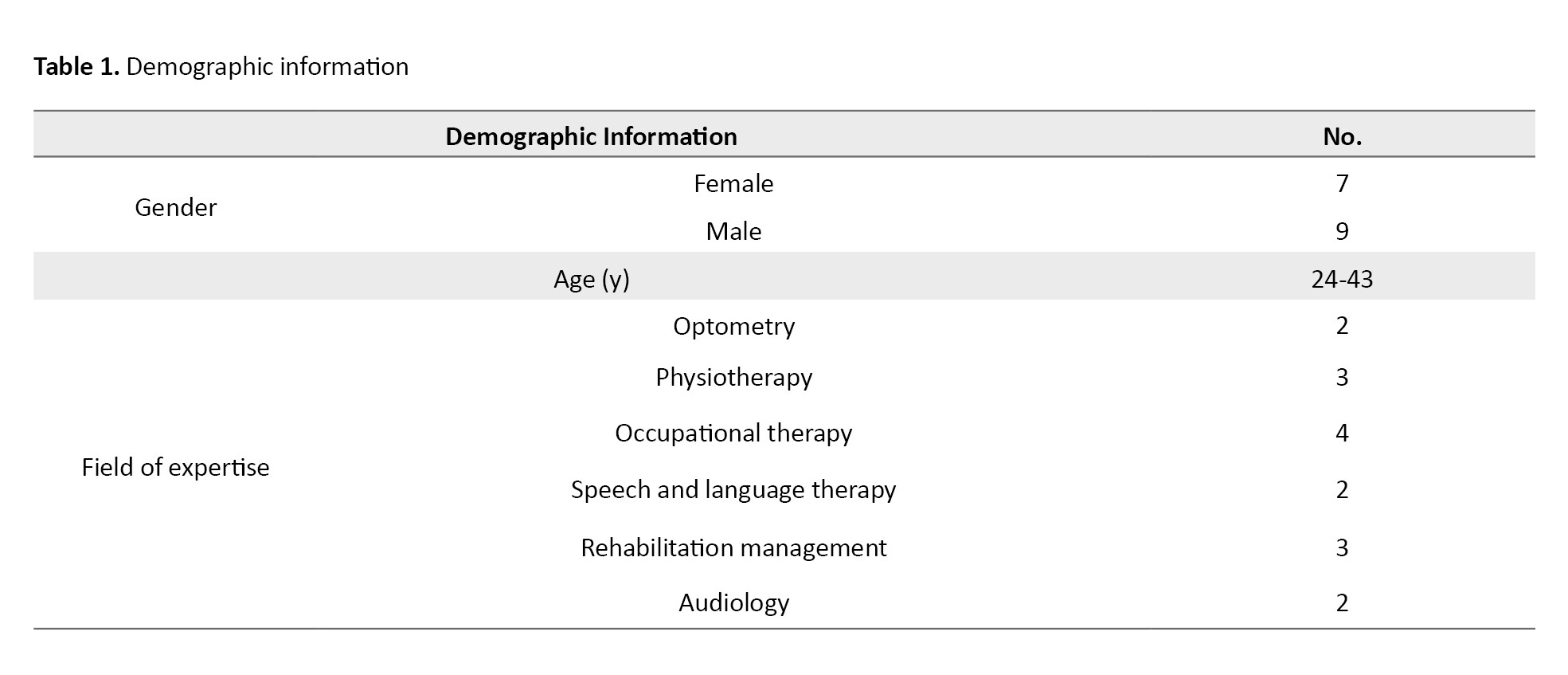
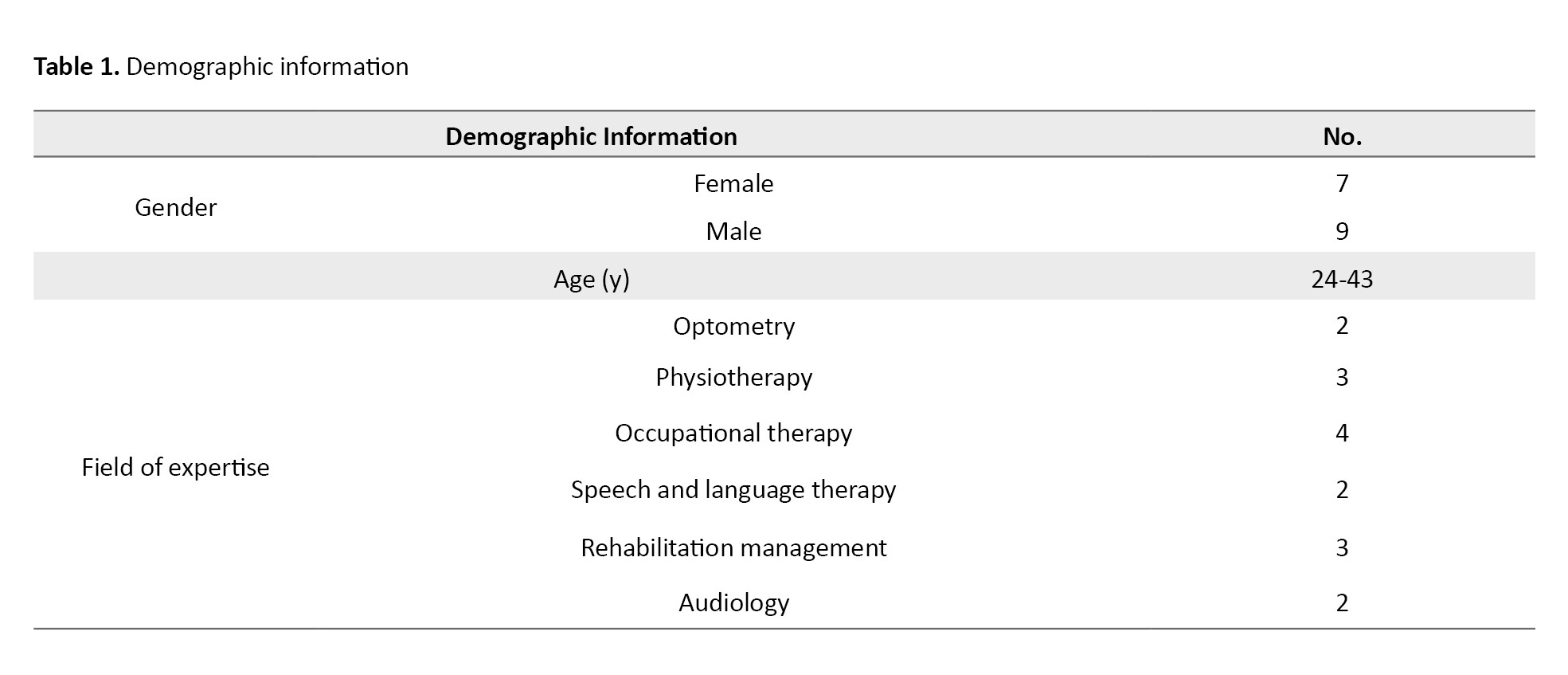
Accordingly, 16 face-to-face interviews were conducted with rehabilitation health professionals aged 24-43 until each new interview yielded little or no new data. This study was performed in April-September 2021. Table 1 lists the demographic characteristics of the participants. The research setting in this study was public, private clinics, hospitals, colleges, or any other center where rehabilitation experts provide services. The Graneheim and Lundman methods were used to analyze the data [17].
The interview transcripts were profoundly read several times, then meaningful units were extracted and the initial codes were formed by classifying similarities and differences. In the last step, the main themes emerged from the original codes and the main categories.
Trustworthiness
To ensure the trustworthiness of the data, Lincoln and Guba’s four evaluative criteria, including credibility, dependability, transferability, and conformability, were used [15]. In this study, the prolonged engagement of the researcher with the participants, interviews with both men and women, member check of transcriptions and the extracted primary codes by the interviewees, data analysis by a team of researchers, and maximum variation sampling, were performed to enhance the credibility of the data. To establish dependability, in every step of coding, three separate researchers who were familiar with qualitative analysis and were experts in the area under study audited the interview transcriptions, both the transcriptions and the obtained codes, and their comments and suggestions were considered in the data analysis. Transferability was ensured through maximum variation sampling, clear, and transparent reporting of the data and results, enabling auditability.
Results
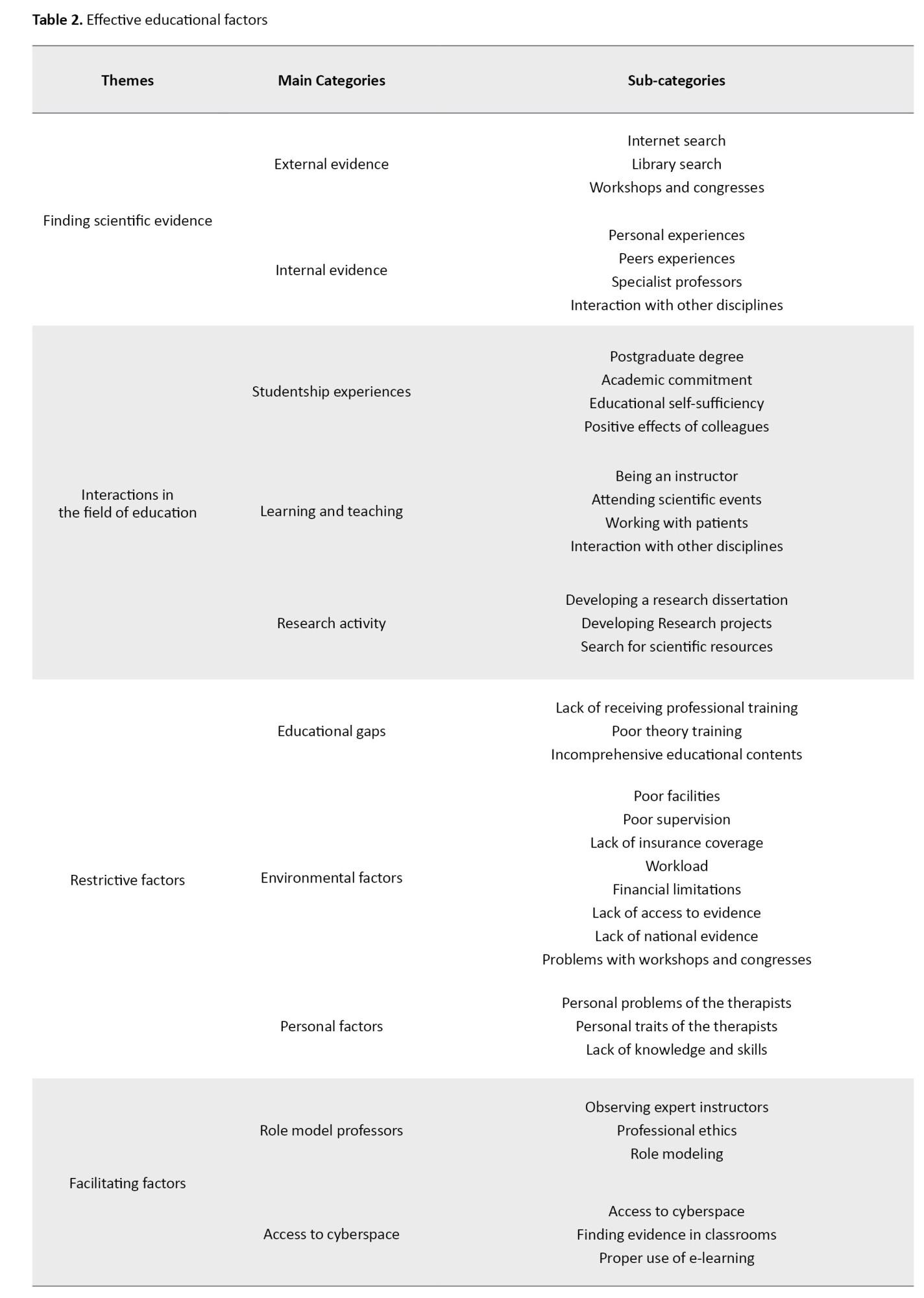
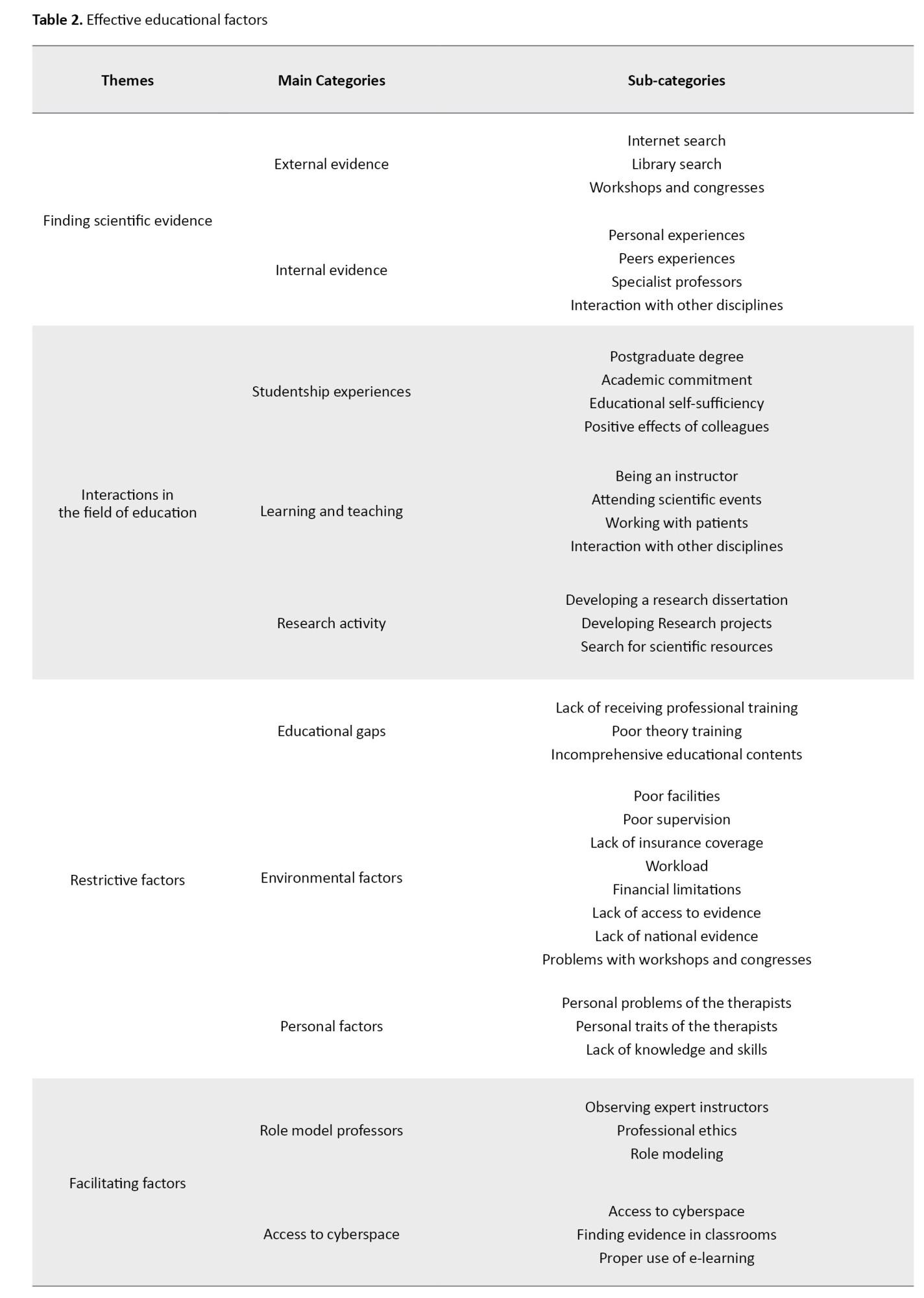
Four themes, 10 categories, and 37 subcategories have been extracted from the study. From the analysis of the data obtained from the interviews, four main themes, namely, “learning to find scientific evidence”, “interaction in the field of education,” “restrictive factors,” and “facilitating factors” emerged (Table 2).
1st theme: Learning to find scientific evidence
After data analysis, rehabilitation professionals seek evidence to implement evidence-based practice. They use both “formal education”, and “self-learning ability “.
Formal education
Participants in this study sought formal education as the 1st step to accessing the relevant scientific information. To achieve this goal, they used four approaches “specialist professors”, “library searches”, “peers experiences” and “participating workshops and congresses”.
Library search and the use of specialist librarians are also other methods of learning to find the best evidence base.
"The library is a great place to find different topics, especially librarians help people how to search. ....” (Participant No. 1).
Attending workshops and congresses was another useful method to seek evidence and stay up to date. In this regard, an occupational therapist said:
“The courses run as workshops, I think, can help, and the cues that the workshops provide help me to go into details and to search for more information in that particular field.” (Participant No. 15).
Self-learning ability
From the participants’ perspective to find valid evidence, in addition to using formal education, it is beneficial to use self-learning ability. Participants in this study used their experiences, search the internet, and interact with other disciplines to explore the evidence.
Searching the Internet to find relevant papers as well as reviewing pertinent websites are two important actions of rehabilitation specialists to access information. One audiologist said, “I usually surf the internet to find out about hearing loss or therapeutic processes…I read case reports or even visit websites that share their clinical experiences. (Participant No. 5)
2nd theme: Interaction in the field of education student life experiences
According to the participants in this study, attending postgraduate courses and being a student has a critical role and provides the condition for using EBP.
A speech therapist elaborated on the impact of academic studentship and said:” wel... I think my years of experience in postgraduate degree play a significant role because the cases you interact with are more relevant to the education and research you are engaged in …. It is a way to bridge the theory-practice gap and interconnect them. (Participant No. 1)
Teaching and learning
Participants with university teaching experience spoke extensively about the impact of teaching and learning activities, and teaching and learning were considered crucial drivers for greater use of the EBP. A faculty member emphasized the importance of being a teacher at university and said:
“Well…I try to have more to say to students each time I teach a specific course… And if something has already been outdated, is under question, or if there’s any doubt about it, I try to make them aware of it and highlight the lack of information and inform them about the new concepts.”(Participant No. 13)
Engagement in research activity
The other notion mentioned by the participants was the stimulating effect of research activities. One of the participants said: “look…, for example, if a journal club is held … if we are active, we should prepare something to present for every session. This implies that we all learn together which, I think is a great help. This increases my motivation so I read more and more and apply my findings to practice to integrate the evidence with the cases I encounter (Participant No. 16).
3rd theme: Restrictive factors
The participants’ statements identified a category that revealed the barriers to learning to use the best evidence, divided into three sub-categories, “educational gap”, “environmental factors” and “individual factors".
Educational Gap
Many participants in this study emphasized that they did not receive evidence-based practice education in universities. The optometrist’s view on the educational gap was:
“Did I have a professor to explain such a concept to me? This teacher leads me as a student in a specific direction and tells the students to go and search a specific website. Teachers encourage students to read papers as a class activity… do scanning for the method section of a scientific paper... Explain the keywords of the paper to students to let them read more papers in that area (Participant No. 7).
Environmental factors
Lack of adequate facilities and poor clinical spaces were other barriers facing therapists in the education of EBP. One of the therapists working in the private sector said: “I don’t know why, maybe due to their commitment, but one problem is that few colleagues work in a suitable environment compatible with what references say about the clinics and their properties…. since it is essential in EBP. I mean, if I am supposed to work with a hearing-impaired child, I need to have appropriate clinical facilities for this purpose according to EBP. If I work with an autism child, I have to design a workroom specifically for children with autism. If this does not happen, I cannot implement evidence-based practice. At least I am sure that this is true about autism.” (Participant No. 4).
Personal factors
According to the participants in this study, one of the most important barriers is those related to the therapists and their conditions. “The therapist’s problems,” “personality traits,” and “lack of knowledge and skills” are the critical barriers to therapists emerging from the analysis of data.
Feeling overconfident about one’s knowledge and clinical abilities were other obstacles associated with the therapists’ personality traits. “One participant pinpointed the false perception of graduate students about their abilities and said:
“Most students feel saturated upon graduating from college and perceive themselves specialists who no longer need to learn. This is something only felt by students who feel they do not need it anymore… perhaps they don’t feel they know everything but they think what they know is enough (Participant No.1).
4th theme: Facilitating factors
This category includes education that is already available to participants to use EBP and promotes this process. The extracted facilitators included “role model professors “ and “access to cyberspace.”
Role model professors
The experience of one participant on the facilitator role of successful professors was as below:” once in the clinic I encounter a complicated case suffering poor growth of the corpus callosum. My colleagues introduced Dr... who is an expert in this field. I met him and he introduced a book to me that was very helpful. Since this was a new case and I had no previous experience working with a similar patient, the guidance of this professor was beneficial to me “(Participant No. 2).
E-learning
Participants in this study believed that the existence of education, such as YouTube and educational websites is another category that facilitates finding evidence-based medicine. A participant highlighted the role of social networks, saying, “now, the recent increase in using YouTube has created a great opportunity for colleagues to share their experiences.” (Participant No.12)
Discussion
In this study, effective factors in the education of EBP in rehabilitation sciences have been examined. In one study participated by three groups of speech and language pathologists, physiotherapists, and occupational therapists, reference books were named as the most popular sources of information referred to by the participants for clinical decision-making. However, the participants claimed that although such references are readily available, they may not contain very recent scientific evidence [18].
Physiotherapists have described peer experiences as the 1st source of information for clinical decision-making, and have introduced seeking research sources as their 2nd source of scientific data [19]. Occupational therapists who had a clinical practice in New Zealand, Australia [20] Canada [21], and the United States [22]also mentioned colleagues’ clinical experiences as their most used source of clinical information rather than research findings [23].
Based on the results, it may be possible to consider individual factors as the basic motivators leading therapists to learn EBP, which is enforced by other stimuli in the context of clinical practice. For instance, a therapist with high self-expectation to provide the best treatment for the patients is more willing to use Evidence-based Practice when faced with a clinical challenge and a rare case of clinical interest [24].
In addition, one of these barriers is the lack of proficiency in English, which is the global language of science and evidence. Today, most scientific evidence, such as papers and reference books published in English [23, 25], and limited papers are published in languages other than English [26]. Therefore, it seems that not only Iranian therapists, but many other therapists in other countries are facing language problems. In addition, this issue has been reported in many studies on nurses [20]. Studies conducted on occupational therapists in Iran, Germany, and other countries have confirmed similar findings [25, 27]. The lack of facilities for using EBP has been cited in previous studies and the participants of the present study confirmed it [27].
Physicians [28], and hand therapists in the United States [29], have reported restrictions in accessing full-text papers in many studies, therapists in New Zealand [30], Australian occupational therapists [31], and Iranian occupational therapists [27], it can conclude that such barriers are universal. The presence of instructors who motivate and encourage the practice of evidence-based medicine was one of the facilitators that some of the participants expressed, which has been implicated in other studies [32].
Conclusion
Nowadays, when we are subject to extensive changes in all fields, the use of EBP is a necessity. The findings of this study showed that EBP is an educational (practical) process. Effective educational factors in evidence-based performance begin by considering the needs of the patients and then looking for the best methods to find the best evidence. Finally, they considered the triple principles of the best evidence medical education, which include the use of available scientific evidence, clinical experiences, and the client’s needs. For treatment, it integrates these parameters and, proper and timely education plays a fundamental role in this process.
Ethical Considerations
Compliance with ethical guidelines
This study has been approved by the Ethics Committee of the Iran University of Medical Sciences (IR.IUMS.1400.101).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, Supervision: Mohammad Hasan Keshavarzi, Seyedeh Zahra Nahardani; Methodology: Mohammad Hasan Keshavarzi, Seyedeh Zahra Nahardani , and Maryam Jalali; Investigation and Writing–review & editing: Marzieh Pashmdarard and Seyedeh Zahra Nahardani; Writing–original draft: Mohammad Hasan Keshavarzi and Seyedeh Zahra Nahardani.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We thank the Rehabilitation Research Center at Iran University of Medical Sciences and all the participants in the study without their valuable contributions it was not possible to complete this project.
References
The development and reform in training require an understanding of the education process, modern methods of implementation, recognition of financial resources and facilities, and awareness of the role and duties of human resources. The inability to properly plan to utilize the skills needed by the learners, such as clinical reasoning, problem-solving and critical thinking has made it necessary to keep up with the recent developments in the field [1, 2].
Evidence-based therapy is a systematic process that involves finding, analyzing, and utilizing the best scientific research to help make scientific reasoning. This process begins with designing a clinical question, continuing with the search for relevant resources, and evaluating its credibility, validity, reliability, and usefulness, which ends with the implementation of clinical research findings and evaluating treatment effectiveness [3].
Evidence-based practice (EBP) individualizes healthcare decision-making and service delivery by “the conscientious, explicit, judicious and reasonable use of the best available evidence”, integrating clinical expertise, and patient values and preferences with the best available research information” [4, 5]. EBP has many benefits, such as making services more effective for each individual, more responsive to clients and their families, providing equal treatment to clients based on scientific evidence, up-to-date therapists, improving the quality of service, enhancing professional credibility, encouraging adherence to ethical principles, promoting interdisciplinary collaboration and communication, encouraging continued learning, promoting service delivery, more appropriate clinical decision-making, establishing appropriate communication between research and clinical services, and the need to use it in many health [6, 7].
In Iran, many efforts have been made to improve rehabilitation services to play a more constructive role in the health system [8]. In addition, the use of EBP does not ignore the clinicians’ experiences; rather it considers these experiences necessary to integrate with scientific evidence and patients’ needs [9] which are of great importance in the rehabilitation field. Therefore, rehabilitation specialists can properly improve the level of service delivery and provide healthier, more qualified, shorter, more effective, reasonable, accurate, and patient-oriented treatments [10].
Much research has been conducted on EBP in rehabilitation fields in different countries [11]. Most of the literature published in the last two decades and along with the emergence and expansion of EBP in the field of rehabilitation sciences were published by scholars of this field and have attempted to promote this process and introduce its benefits of it [6, 7, 12].
Most of these studies have been conducted using a quantitative method, and have largely examined the therapists’ knowledge, attitude, and practice toward EBP [11, 13]. In this study, general documents for other professions have been used. While each discipline has its particular conditions that can influence the intake of EBP, cultural conditions are also influential in this regard [14]. Considering the importance of EBP in rehabilitation sciences and meeting the community’s needs, this study aimed to explain the effective educational factors in adopting EBP in the fields of rehabilitation sciences.
Materials and Methods
This study used inductive qualitative content analysis to interpret subjective data scientifically, encode data through a regular process, and identify themes and patterns [15, 16]. All interviews were tape-recorded and then transcribed and analyzed. All principles of informed consent, anonymity, confidentiality, the right to withdraw from participation at any time, and ethical obligations were fully observed in the present research.
Accordingly, 16 face-to-face interviews were conducted with rehabilitation health professionals aged 24-43 until each new interview yielded little or no new data. This study was performed in April-September 2021. Table 1 lists the demographic characteristics of the participants. The research setting in this study was public, private clinics, hospitals, colleges, or any other center where rehabilitation experts provide services. The Graneheim and Lundman methods were used to analyze the data [17].
The interview transcripts were profoundly read several times, then meaningful units were extracted and the initial codes were formed by classifying similarities and differences. In the last step, the main themes emerged from the original codes and the main categories.
Trustworthiness
To ensure the trustworthiness of the data, Lincoln and Guba’s four evaluative criteria, including credibility, dependability, transferability, and conformability, were used [15]. In this study, the prolonged engagement of the researcher with the participants, interviews with both men and women, member check of transcriptions and the extracted primary codes by the interviewees, data analysis by a team of researchers, and maximum variation sampling, were performed to enhance the credibility of the data. To establish dependability, in every step of coding, three separate researchers who were familiar with qualitative analysis and were experts in the area under study audited the interview transcriptions, both the transcriptions and the obtained codes, and their comments and suggestions were considered in the data analysis. Transferability was ensured through maximum variation sampling, clear, and transparent reporting of the data and results, enabling auditability.
Results
Four themes, 10 categories, and 37 subcategories have been extracted from the study. From the analysis of the data obtained from the interviews, four main themes, namely, “learning to find scientific evidence”, “interaction in the field of education,” “restrictive factors,” and “facilitating factors” emerged (Table 2).
1st theme: Learning to find scientific evidence
After data analysis, rehabilitation professionals seek evidence to implement evidence-based practice. They use both “formal education”, and “self-learning ability “.
Formal education
Participants in this study sought formal education as the 1st step to accessing the relevant scientific information. To achieve this goal, they used four approaches “specialist professors”, “library searches”, “peers experiences” and “participating workshops and congresses”.
Library search and the use of specialist librarians are also other methods of learning to find the best evidence base.
"The library is a great place to find different topics, especially librarians help people how to search. ....” (Participant No. 1).
Attending workshops and congresses was another useful method to seek evidence and stay up to date. In this regard, an occupational therapist said:
“The courses run as workshops, I think, can help, and the cues that the workshops provide help me to go into details and to search for more information in that particular field.” (Participant No. 15).
Self-learning ability
From the participants’ perspective to find valid evidence, in addition to using formal education, it is beneficial to use self-learning ability. Participants in this study used their experiences, search the internet, and interact with other disciplines to explore the evidence.
Searching the Internet to find relevant papers as well as reviewing pertinent websites are two important actions of rehabilitation specialists to access information. One audiologist said, “I usually surf the internet to find out about hearing loss or therapeutic processes…I read case reports or even visit websites that share their clinical experiences. (Participant No. 5)
2nd theme: Interaction in the field of education student life experiences
According to the participants in this study, attending postgraduate courses and being a student has a critical role and provides the condition for using EBP.
A speech therapist elaborated on the impact of academic studentship and said:” wel... I think my years of experience in postgraduate degree play a significant role because the cases you interact with are more relevant to the education and research you are engaged in …. It is a way to bridge the theory-practice gap and interconnect them. (Participant No. 1)
Teaching and learning
Participants with university teaching experience spoke extensively about the impact of teaching and learning activities, and teaching and learning were considered crucial drivers for greater use of the EBP. A faculty member emphasized the importance of being a teacher at university and said:
“Well…I try to have more to say to students each time I teach a specific course… And if something has already been outdated, is under question, or if there’s any doubt about it, I try to make them aware of it and highlight the lack of information and inform them about the new concepts.”(Participant No. 13)
Engagement in research activity
The other notion mentioned by the participants was the stimulating effect of research activities. One of the participants said: “look…, for example, if a journal club is held … if we are active, we should prepare something to present for every session. This implies that we all learn together which, I think is a great help. This increases my motivation so I read more and more and apply my findings to practice to integrate the evidence with the cases I encounter (Participant No. 16).
3rd theme: Restrictive factors
The participants’ statements identified a category that revealed the barriers to learning to use the best evidence, divided into three sub-categories, “educational gap”, “environmental factors” and “individual factors".
Educational Gap
Many participants in this study emphasized that they did not receive evidence-based practice education in universities. The optometrist’s view on the educational gap was:
“Did I have a professor to explain such a concept to me? This teacher leads me as a student in a specific direction and tells the students to go and search a specific website. Teachers encourage students to read papers as a class activity… do scanning for the method section of a scientific paper... Explain the keywords of the paper to students to let them read more papers in that area (Participant No. 7).
Environmental factors
Lack of adequate facilities and poor clinical spaces were other barriers facing therapists in the education of EBP. One of the therapists working in the private sector said: “I don’t know why, maybe due to their commitment, but one problem is that few colleagues work in a suitable environment compatible with what references say about the clinics and their properties…. since it is essential in EBP. I mean, if I am supposed to work with a hearing-impaired child, I need to have appropriate clinical facilities for this purpose according to EBP. If I work with an autism child, I have to design a workroom specifically for children with autism. If this does not happen, I cannot implement evidence-based practice. At least I am sure that this is true about autism.” (Participant No. 4).
Personal factors
According to the participants in this study, one of the most important barriers is those related to the therapists and their conditions. “The therapist’s problems,” “personality traits,” and “lack of knowledge and skills” are the critical barriers to therapists emerging from the analysis of data.
Feeling overconfident about one’s knowledge and clinical abilities were other obstacles associated with the therapists’ personality traits. “One participant pinpointed the false perception of graduate students about their abilities and said:
“Most students feel saturated upon graduating from college and perceive themselves specialists who no longer need to learn. This is something only felt by students who feel they do not need it anymore… perhaps they don’t feel they know everything but they think what they know is enough (Participant No.1).
4th theme: Facilitating factors
This category includes education that is already available to participants to use EBP and promotes this process. The extracted facilitators included “role model professors “ and “access to cyberspace.”
Role model professors
The experience of one participant on the facilitator role of successful professors was as below:” once in the clinic I encounter a complicated case suffering poor growth of the corpus callosum. My colleagues introduced Dr... who is an expert in this field. I met him and he introduced a book to me that was very helpful. Since this was a new case and I had no previous experience working with a similar patient, the guidance of this professor was beneficial to me “(Participant No. 2).
E-learning
Participants in this study believed that the existence of education, such as YouTube and educational websites is another category that facilitates finding evidence-based medicine. A participant highlighted the role of social networks, saying, “now, the recent increase in using YouTube has created a great opportunity for colleagues to share their experiences.” (Participant No.12)
Discussion
In this study, effective factors in the education of EBP in rehabilitation sciences have been examined. In one study participated by three groups of speech and language pathologists, physiotherapists, and occupational therapists, reference books were named as the most popular sources of information referred to by the participants for clinical decision-making. However, the participants claimed that although such references are readily available, they may not contain very recent scientific evidence [18].
Physiotherapists have described peer experiences as the 1st source of information for clinical decision-making, and have introduced seeking research sources as their 2nd source of scientific data [19]. Occupational therapists who had a clinical practice in New Zealand, Australia [20] Canada [21], and the United States [22]also mentioned colleagues’ clinical experiences as their most used source of clinical information rather than research findings [23].
Based on the results, it may be possible to consider individual factors as the basic motivators leading therapists to learn EBP, which is enforced by other stimuli in the context of clinical practice. For instance, a therapist with high self-expectation to provide the best treatment for the patients is more willing to use Evidence-based Practice when faced with a clinical challenge and a rare case of clinical interest [24].
In addition, one of these barriers is the lack of proficiency in English, which is the global language of science and evidence. Today, most scientific evidence, such as papers and reference books published in English [23, 25], and limited papers are published in languages other than English [26]. Therefore, it seems that not only Iranian therapists, but many other therapists in other countries are facing language problems. In addition, this issue has been reported in many studies on nurses [20]. Studies conducted on occupational therapists in Iran, Germany, and other countries have confirmed similar findings [25, 27]. The lack of facilities for using EBP has been cited in previous studies and the participants of the present study confirmed it [27].
Physicians [28], and hand therapists in the United States [29], have reported restrictions in accessing full-text papers in many studies, therapists in New Zealand [30], Australian occupational therapists [31], and Iranian occupational therapists [27], it can conclude that such barriers are universal. The presence of instructors who motivate and encourage the practice of evidence-based medicine was one of the facilitators that some of the participants expressed, which has been implicated in other studies [32].
Conclusion
Nowadays, when we are subject to extensive changes in all fields, the use of EBP is a necessity. The findings of this study showed that EBP is an educational (practical) process. Effective educational factors in evidence-based performance begin by considering the needs of the patients and then looking for the best methods to find the best evidence. Finally, they considered the triple principles of the best evidence medical education, which include the use of available scientific evidence, clinical experiences, and the client’s needs. For treatment, it integrates these parameters and, proper and timely education plays a fundamental role in this process.
Ethical Considerations
Compliance with ethical guidelines
This study has been approved by the Ethics Committee of the Iran University of Medical Sciences (IR.IUMS.1400.101).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, Supervision: Mohammad Hasan Keshavarzi, Seyedeh Zahra Nahardani; Methodology: Mohammad Hasan Keshavarzi, Seyedeh Zahra Nahardani , and Maryam Jalali; Investigation and Writing–review & editing: Marzieh Pashmdarard and Seyedeh Zahra Nahardani; Writing–original draft: Mohammad Hasan Keshavarzi and Seyedeh Zahra Nahardani.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We thank the Rehabilitation Research Center at Iran University of Medical Sciences and all the participants in the study without their valuable contributions it was not possible to complete this project.
References
- Elahi N, Alhani F, Ahmadi F. [Effective education: Perceptions and experiences of nursing students (Persian)]. Iran J Med Educ. 2012; 12:2:110-9. [Link]
- Sohrabi Z, Koohestani HR, Nahardani SZ, Keshavarzi MH. Data on the knowledge, attitude, and performance of PhD students attending an educational course (Tehran, Iran). Data Brief. 2018; 21:1325-8. [DOI:10.1016/j.dib.2018.08.081] [PMID] [PMCID]
- Dysart AM, Tomlin GS. Factors related to evidence-based practice among US occupational therapy clinicians. Am J Occup Ther. 2002; 56(3):275-84. [DOI:10.5014/ajot.56.3.275] [PMID]
- Brackenbury T, Burroughs E, Hewitt LE. A qualitative examination of current guidelines for evidence-based practice in child language intervention. Lang Speech Hear Serv Sch. 2008; 39(1):78-88. [DOI:10.1044/0161-1461(2008/008)] [PMID]
- Walker BF, Stomski NJ, Hebert JJ, French SD. Evidence-based practice in chiropractic practice: A survey of chiropractors’ knowledge, skills, use of research literature and barriers to the use of research evidence. Complement Ther Med. 2014; 22(2):286-95. [DOI:10.1016/j.ctim.2014.02.007] [PMID]
- Raghavendra P. Teaching evidence-based practice in a problem-based learning course in speech-language pathology. Evid Based Commun Assess Interv. 2009; 3(4):232-7. [DOI:10.1080/17489530903399160]
- Roddam H, Skeat J. Embedding evidence-based practice in speech and language therapy: International examples. Hoboken: John Wiley & Sons; 2010. [DOI:10.1002/9780470686584]
- Sackett DL, Richardson WS, Straus SE, Richardson WS, Rosenberg W, Haynes RB. Asking answerable clinical questions. In: Evidence-based medicine: How to practice and teach EBM, Sackett DL, Richardson WS, Straus SE, Richardson WS, Rosenberg W, Haynes RB, editors. Edinburgh: Churchill Livingstone; 2000. [Link]
- Dodd B. Evidence-based practice and speech-language pathology: Strengths, weaknesses, opportunities and threats. Folia Phoniatr Logop. 2007; 59(3):118-29. [DOI:10.1159/000101770] [PMID]
- Alizadeh S, Nahardani SZ, Sohrabi Z, Doorfard M. [The effect of announced and unannounced formative tests on rehabilitation students’ final exam mean scores (Persian)]. Iran J Med Edu. 2015; 15:656-62. [Link]
- Tahmasebifard N, Nakhshab M, Shafiei M. [A primary study on the attitude, knowledge and behavior of speech and language pathologists toward evidence-based practice (Persian)]. J Res Rehabil Sci. 2012; 8(1):65-76. [Link]
- Lass NJ, Pannbacker M. The application of evidence-based practice to nonspeech oral motor treatments. Lang Speech Hear Serv Sch. 2008; 39(3):408-21. [DOI:10.1044/0161-1461(2008/038)] [PMID]
- Zipoli Jr., RP, Kennedy M. Evidence-based practice among speech-language pathologists. Am J Speech Lang Pathol. 2005; 14(3):208-20. [DOI:10.1044/1058-0360(2005/021)] [PMID]
- de Beer J, Kalf JG. Evidence-based logopedie. Houten: Bohn Stafleu van Loghum; 2003. [Link]
- Moretti F, van Vliet L, Bensing J, Deledda G, Mazzi M, Rimondini M, et al. A standardized approach to qualitative content analysis of focus group discussions from different countries. Patient Educ Couns. 2011; 82(3):420-8. [DOI:10.1016/j.pec.2011.01.005] [PMID]
- Polit DF, Beck CT. Nursing research: Principles and methods. Philadelphi: Lippincott Williams & Wilkins; 2004. [Link]
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004; 24(2):105-12. [DOI:10.1016/j.nedt.2003.10.001] [PMID]
- Pain K, Magill-Evans J, Darrah J, Hagler P, Warren S. Effects of profession and facility type on research utilization by rehabilitation professionals. J Allied Health. 2004; 33(1):3-9. [PMID]
- Salbach NM, Veinot P, Rappolt S, Bayley M, Burnett D, Judd M, et al. Physical therapists’ experiences updating the clinical management of walking rehabilitation after stroke: A qualitative study. Phys Ther. 2009; 89(6):556-68. [DOI:10.2522/ptj.20080249] [PMID]
- Bartelt TC, Ziebert C, Sawin KJ, Malin S, Nugent M, Simpson P. Evidence-based practice: Perceptions, skills, and activities of pediatric health care professionals. J Pediatr Nurs. 2011; 26(2):114-21. [DOI:10.1016/j.pedn.2010.12.003] [PMID]
- Dubouloz CJ, Egan M, Vallerand J, von Zweck C. Occupational therapists’ perceptions of evidence-based practice. Am J Occup Ther. 1999; 53(5):445-53. [DOI:10.5014/ajot.53.5.445] [PMID]
- Cameron KA, Ballantyne S, Kulbitsky A, Margolis‐Gal M, Daugherty T, Ludwig F. Utilization of evidence‐based practice by registered occupational therapists. Occup Ther Int. 2005; 12(3):123-36. [DOI:10.1002/oti.1] [PMID]
- Dunlap PM, Holmberg JM, Whitney SL. Vestibular rehabilitation: Advances in peripheral and central vestibular disorders. Curr Opin Neurol. 2019; 32(1):137-44. [DOI:10.1097/WCO.0000000000000632] [PMID]
- Roberts AE, Barber G. Applying research evidence to practice. Br J Occup Ther. 2001; 64(5):223-7. [DO:10.1177/030802260106400503]
- Döpp CM, Steultjens EM, Radel J. A survey of evidence‐based practise among Dutch occupational therapists. Occup Ther Int. 2012; 19(1):17-27. [DOI:10.1002/oti.324] [PMID]
- Maher CG, Sherrington C, Elkins M, Herbert RD, Moseley AM. Challenges for evidence-based physical therapy: Accessing and interpreting high-quality evidence on therapy. Phys Ther. 2004; 84(7):644-54. [DOI:10.1093/ptj/84.7.644] [PMID]
- Lajevardi L, Rassafiani M, Shafaroodi N, Hassani Mehraban A, Ahmadi M. Quality of methodological design and level of research articles published by occupational therapists in Iranian scientific journals. World Fed Occup Ther Bull. 2011; 64(1):39-42. [DOI:10.1179/otb.2011.64.1.009]
- Green ML, Ruff TR. Why do residents fail to answer their clinical questions? A qualitative study of barriers to practicing evidence-based medicine. Acad Med. 2005; 80(2):176-82. [DOI:10.1097/00001888-200502000-00016] [PMID]
- Valdes K, von der Heyde R. Attitudes and opinions of evidence-based practice among hand therapists: A survey study. J Hand Ther. 2012; 25(3):288-96. [DOI:10.1016/j.jht.2012.02.001] [PMID]
- Schreiber J, Stern P, Marchetti G, Provident I. Strategies to promote evidence-based practice in pediatric physical therapy: A formative evaluation pilot project. Phys Ther. 2009; 89(9):918-33. [DOI:10.2522/ptj.20080260] [PMID]
- Lyons C, Brown T, Tseng MH, Casey J, McDonald R. Evidence‐based practice and research utilisation: Perceived research knowledge, attitudes, practices and barriers among Australian paediatric occupational therapists. Aust Occup Ther J. 2011; 58(3):178-86. [DOI:10.1111/j.1440-1630.2010.00900.x] [PMID]
- Khakpour A. Effectiveness of knowledge acquisition in medical education: An argumentative literature review of the resourcesâ s requirements. Future Med Educ J. 2020; 10(3):56-63. [DOI:10.22038/FMEJ.2020.40998.1271]
Type of Study: Research |
Subject:
Professional education and practice
Received: 2022/10/23 | Accepted: 2022/11/8 | Published: 2022/02/3
Received: 2022/10/23 | Accepted: 2022/11/8 | Published: 2022/02/3