Volume 5, Issue 1 (Continuously Updated 2022)
Func Disabil J 2022, 5(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Riazi A, Firouzi N, Salehi R. Evaluating the Performance of Anterior Segment Optical Coherence Tomography MS-39 in Evaluating Tear Film and Comparing the Results With Tear Break-up Time Results by Slit Lamp. Func Disabil J 2022; 5 (1) : 56
URL: http://fdj.iums.ac.ir/article-1-187-en.html
URL: http://fdj.iums.ac.ir/article-1-187-en.html
1- Department of Optometry, Rehabilitation Research Center, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Optometry, Faculty of Rehabilitation, Iran University of Medical Sciences, Tehran, Iran. ,Nargesfiroozi1374@gmail.com
3- Department of Rehabilitation Managment, Faculty of Rehabilitation, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Optometry, Faculty of Rehabilitation, Iran University of Medical Sciences, Tehran, Iran. ,
3- Department of Rehabilitation Managment, Faculty of Rehabilitation, Iran University of Medical Sciences, Tehran, Iran.
Keywords: Tear film, Non-invasive tear film breakup time (NIBUT), Tear break-up time (TBUT), Optical coherence tomography (OCT) MS-39, Slit lamp
Full-Text [PDF 1085 kb]
(819 Downloads)
| Abstract (HTML) (1810 Views)
Full-Text: (665 Views)
Introduction
The human tear film has 3 layers, the outer layer of which is a lipid, which prevents the evaporation of the aqueous layer and maintains the thickness of the tear film, and its defect causes dry eyes [1]. Dry eye is a multifactorial disease related to tears and the ocular surface, which causes symptoms of eye discomfort, visual impairment, and tear film instability with the potential to damage the ocular surface. This problem is associated with increased osmolarity of the tear film and inflammation of the ocular surface [2].
Evaluating tear stability has several methods, one of which is the tear break-up time (TBUT) test. A TBUT of less than 10 second indicates tear film instability [3]. TBUT tests can be evaluated by invasive and non-invasive methods. The most common invasive method is the silt-lamp TBUT test [4]. This is done by applying a wet fluorescein strip to the bulbar conjunctiva and asking the patient to blink several times and then stare straight ahead. Using a wide light and a cobalt blue filter, the examiner records when he sees a black amoeba-shaped spot or more in the corneal tear film. The appearance of this black spot shows that the tear film is “broken” [5].
However, fluorescein has a destabilizing effect on the tear film and can underestimate the original values (causing the tear film to break earlier), in addition, it is more difficult to perform the TBUT test in some people. Some people react more strongly to the entry of any type of foreign substance (including fluorescein) and produce more intense reflex tears, which causes errors in the results. Seeing the tear film breaking with the naked eye causes a delay in recording the result, and a digital camera can provide a more accurate result. For this reason, in recent years, a tendency exists toward non-invasive methods to evaluate the tear film in natural conditions [3]. One of these non-invasive methods is non-invasive tear film breakup time (NIBUT) with the anterior segment-optical coherence tomography (AS-OCT) MS-39 device. Advanced analysis of tear film with AS-OCT MS-39 is possible according to the chief security officer (CSO) company via Placido disk technology, called NIBUT [6]. Since this feature is newly added to the OCT device, it is necessary to check whether the results provided by this device can be reliable in people who do not cooperate to perform the usual TBUT test with the slit lamp device, and these two methods can be replaced in necessary cases.
Since several different methods evaluate dry eye, each with advantages and disadvantages, it is essential to find a method that has the most advantages and the least disadvantages. Therefore, this study aims to investigate the performance of the MS-39 anterior segment OCT device in tear film examination compared to the TBUT test with a slit lamp.
Materials and Methods
The data collection method in this study is an observational clinical test method. The first device used is the anterior OCT MS-39 made by the Italian chief security officer (CSO) company, the 2019 version of which was used in this research. This device uses a Placido screen that lights up in red to evaluate the tear film. The working method of the device is that the device takes a video from the tear film to perform the test and records the time when the Placido rings collide as the result of the NIBUT test. The test is repeated three times with an interval of 30 second and then the average of the three results is taken. We waited 5 minutes to make sure that the tear film was restored. Then TBUT test was taken from the same eye of the same participant with a slit lamp device (Hagg-Streit model). In this way, fluorescein was instilled in the eye conjunctiva using a fluorescein tape. We waited for 3 second. Then the person was asked to blink three times and then stare forward behind the slit lamp without blinking (the person should not look at the light). We looked at the person’s eyes with a cobalt blue filter and the time of formation of black spots in the tear film was recorded as the result of the TBUT test in seconds. Thirty seconds after the end of this stage, the person was asked to blink three times and the test was repeated. The test was repeated three times. Then the results were averaged. first, the NIBUT method was performed with the MS-39 anterior segment OCT device because the TBUT method with a slit lamp is invasive and can affect the tear film and distort the results of subsequent tests.
The statistical methods in this study included descriptive methods of mean and data dispersion to average the results of two tests, analytical methods including paired t-tests to compare two methods together, and the distribution matching test of two methods with non-parametric tests. The statistical population included people aged 18 to 35 years who were referred to Negah ophthalmology hospital in Tehran City, Iran, and had no history of laser refractive surgery or disease involving the anterior segment. The sampling method in this study is the non-probability sampling method.
The calculation of the sample size according to Eroglu et al.’s article [7] and considering TBUT as the primary outcome has been calculated with the paired t method as follows: according to the above article and considering TAIL equal to 2, and the impact size equal to 0.897; If α err prob is considered at 0.05; The non-central parameter δ is 3.913, fundamental t is 2.101 and df is 18, which is 19 eyes according to the calculation of the sample size, which is obtained by considering the probability of a 20% drop out of the sample size of 23 eyes.
The inclusion criteria included people aged 18-35 years because this age group has better cooperation. Also, people who do not have a history of anterior eye surgery can enter the examination because no change was observed in the structure of their eyes. Also, people without a history of eye disease will provide more reliable results.
The exclusion criteria included any pre-test assessment that disturbs the stability of the tear film and lack of appropriate cooperation during the test.
Results
In this study, 23 eyes of 23 people were evaluated. The participants in this study included 16 women (69%) and 7 men (31%). The age range of people is 18 to 35 years with an average of 4.456±29.30 years.
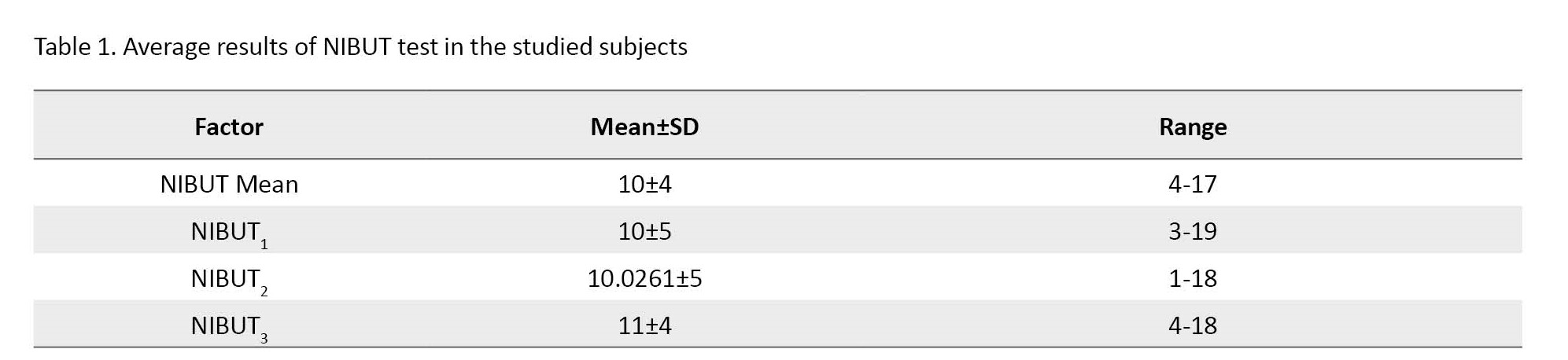
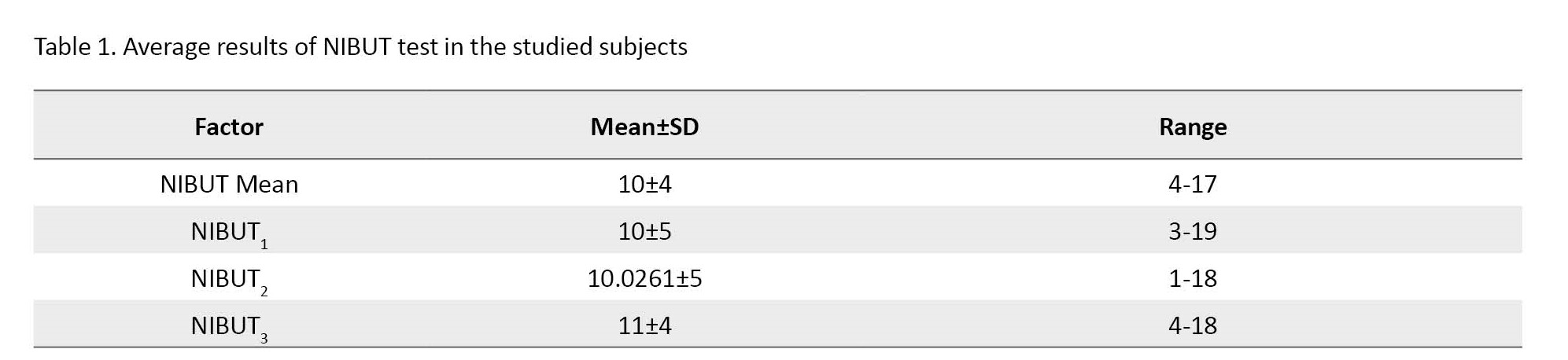
Average results of NIBUT test in the studied subjects
According to Table 1, the total average results of the NIBUT test in participants is 10 s. The maximum amount of NIBUT is 17 s and the minimum amount is 4 s, that is, the range of changes of this variable is from 4 s to 17 s (13 s). The average results of the first NIBUT evaluation (NIBUT1) in the studied subjects are 10 s, the average results of the second NIBUT evaluation (NIBUT2) is 10.0261 s, and the average results of the third NIBUT evaluation (NIBUT3) is 11 s.
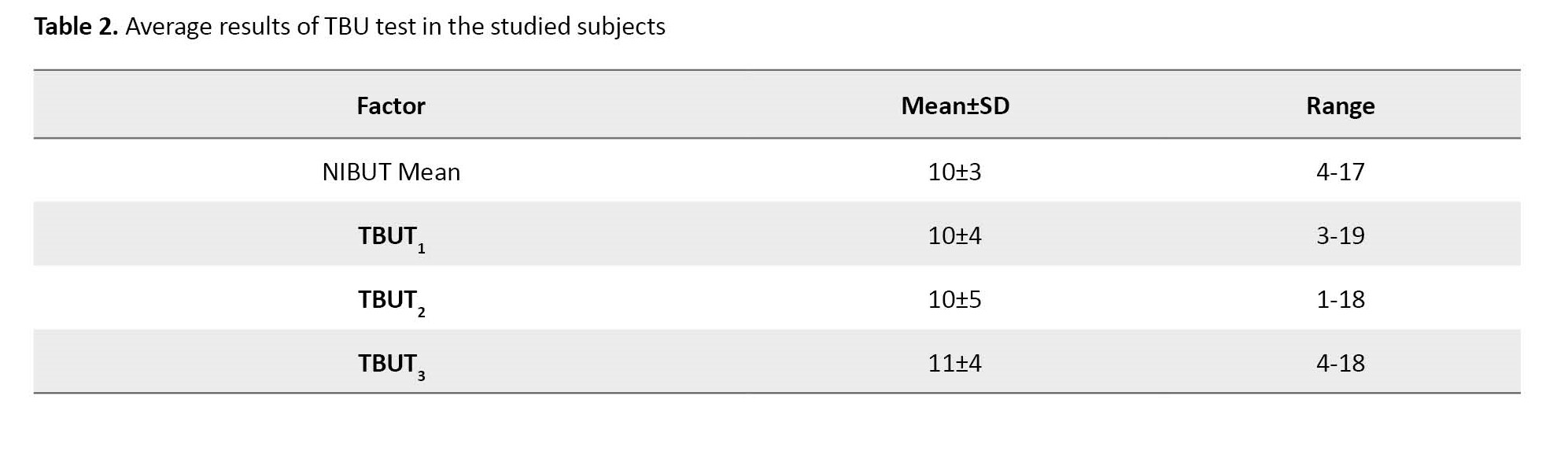
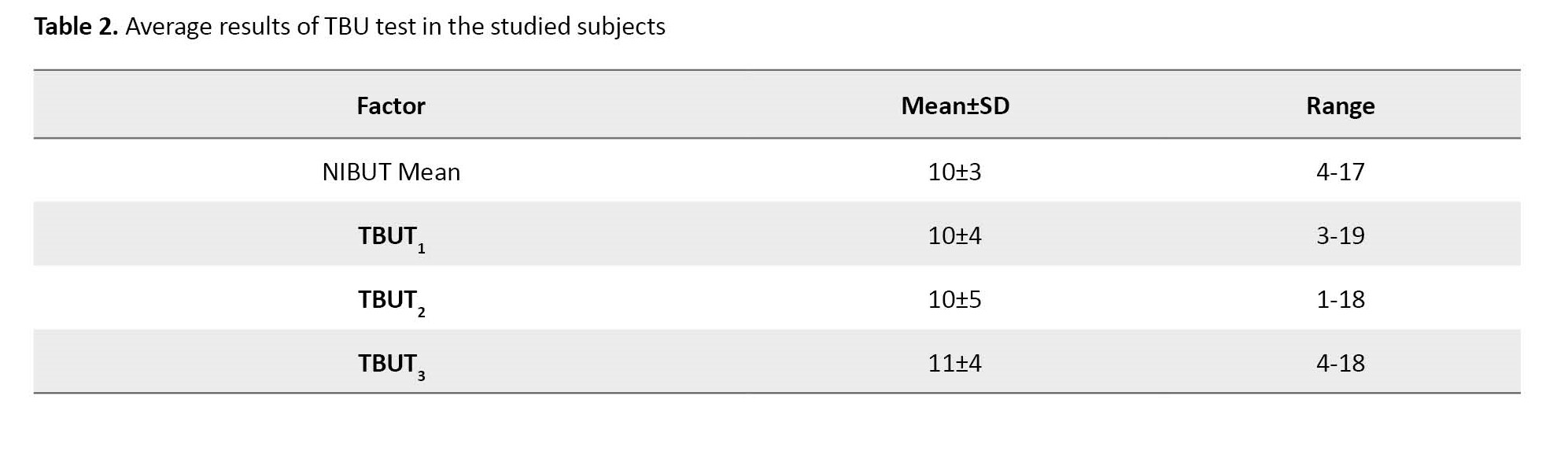
Average results of TBUT test in the studied subjects
According to Table 2, the average results of the TBUT test in the participants is 10 s. The maximum amount of TBUT is 17 s and the minimum is 4 s, that is, the range of changes of this variable is from 4 s to 17 s (13 s). The average results of the first evaluation of TBUT (TBUT1) in participants are 10.0870 s, the average results of the second evaluation of TBUT (TBUT2) in participants are 10 s, and the average results of the third evaluation of TBUT (TBUT3) in participants are also 10 s.
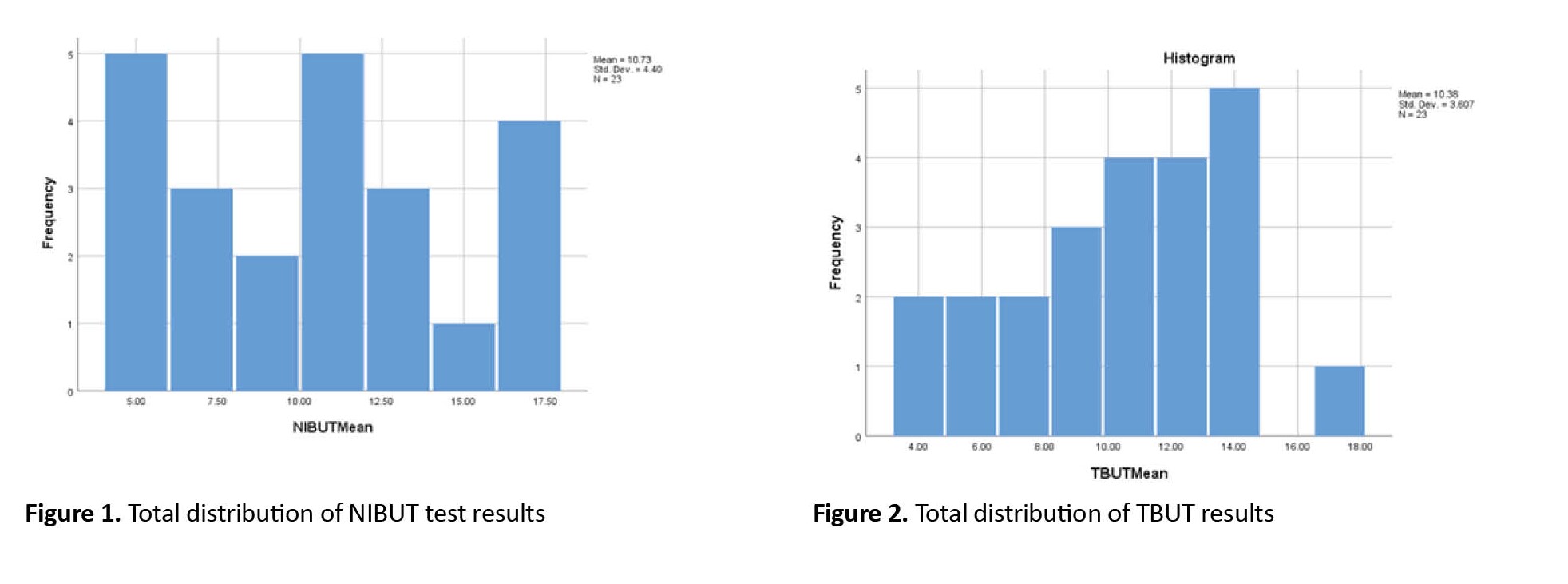
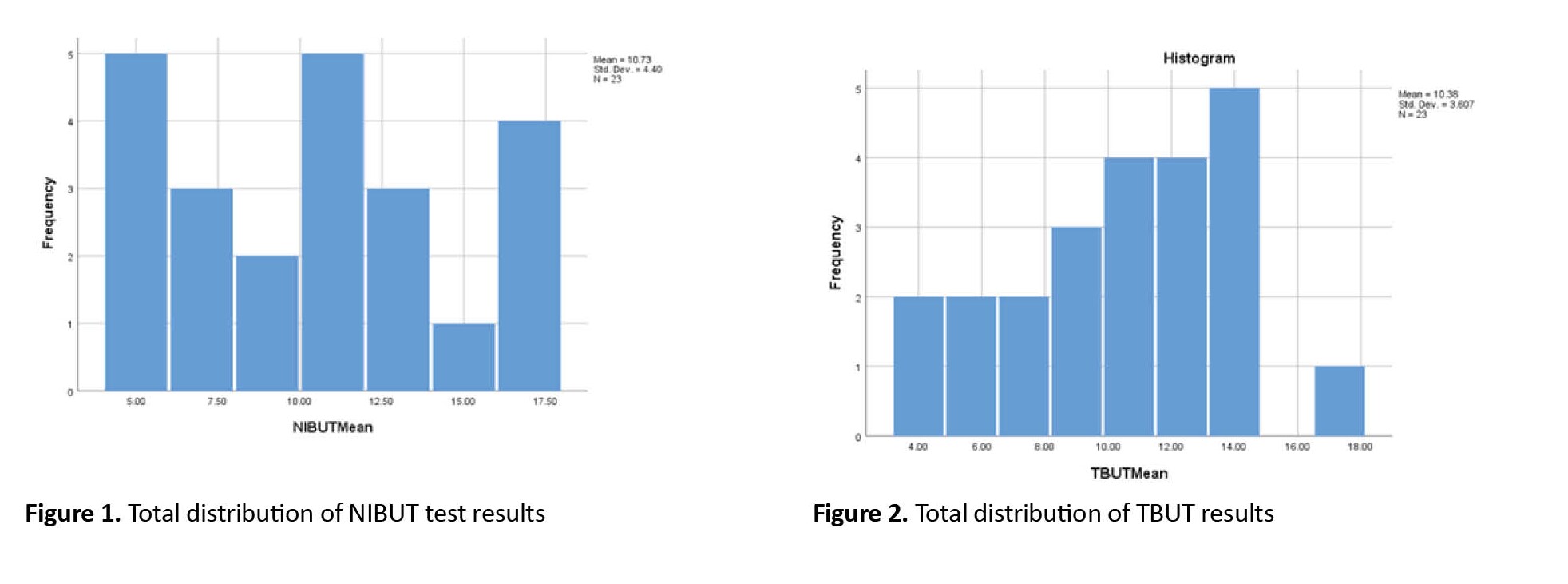
Total distribution of the results of the NIBUT test in the studied subjects
According to the Figure 1, the average NIBUT variable in this study is 10s. Its minimum value is 4 and its maximum value is 17s, and its standard deviation is 4s. The distribution histogram of this variable is shown (Figure 1).
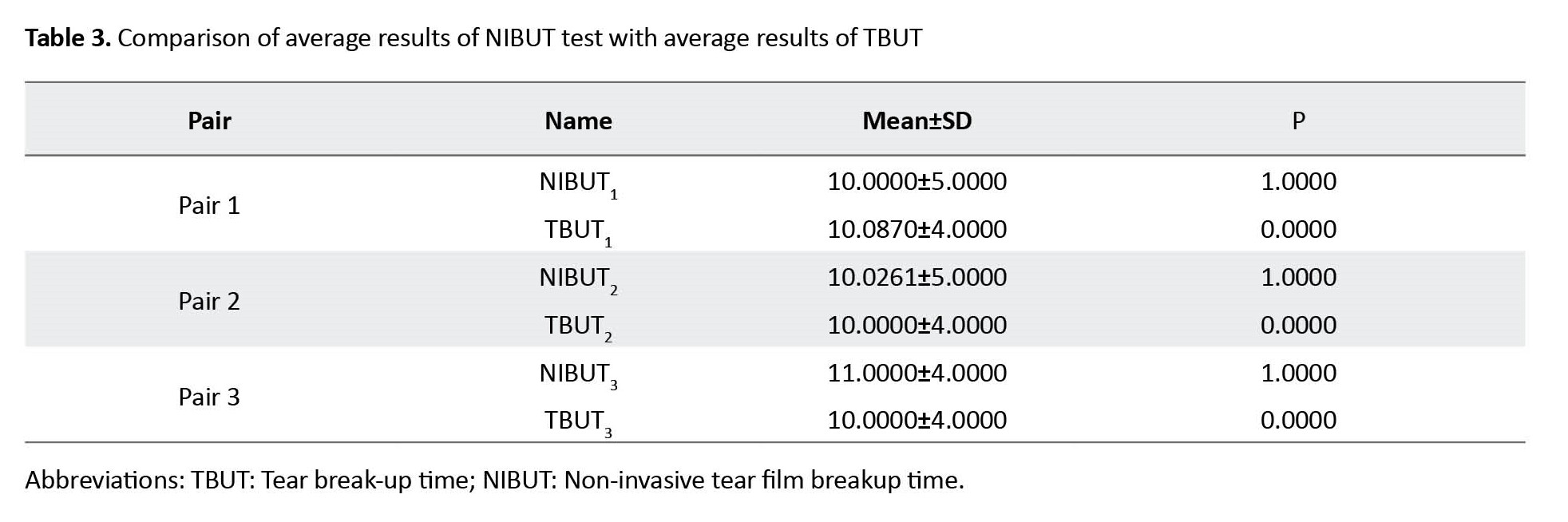
Total distribution of the results of the TBUT in the studied subjects
According the Figure 2, the average TBUT variable in the studied subjects is 10 seconds. Its minimum value is 4s, its maximum value is 17s, and its standard deviation is 3s. The histogram of the distribution of this variable is shown (Figure 2).
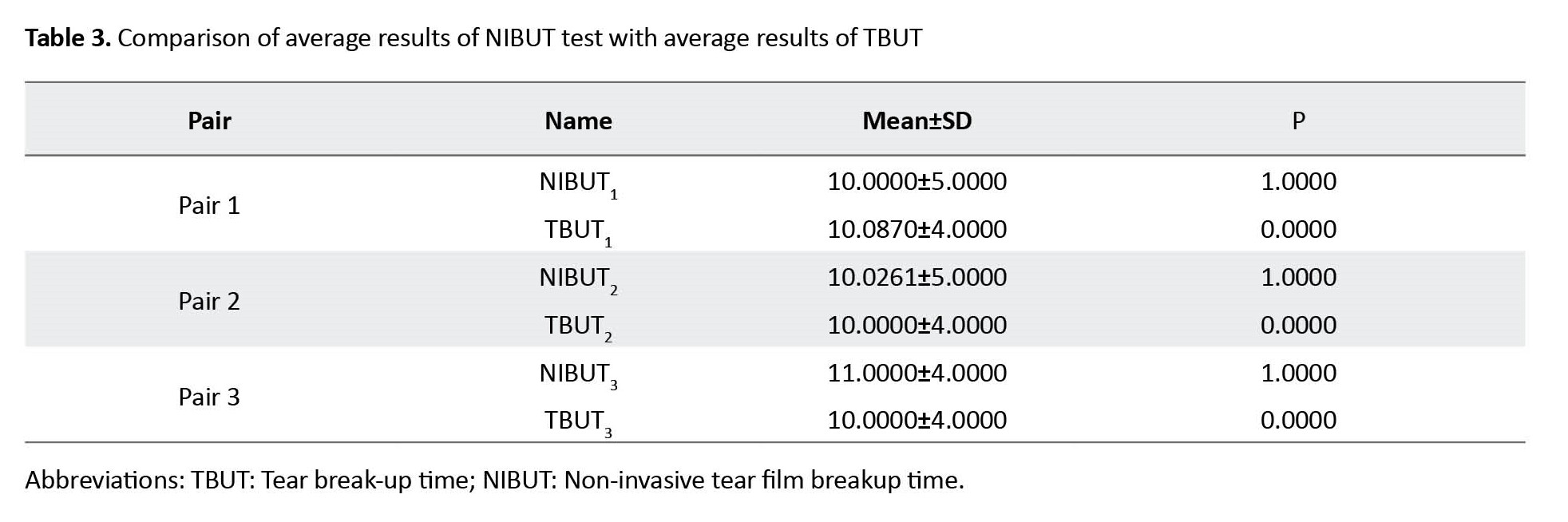
Comparison of average results of the NIBUT with average results of TBUT
According to Table 3, The total average of both variables is equal to 10 seconds. The average evaluation of the first-time NIBUT is equal to 10s and the average evaluation of the first-time TBUT is equal to 10.0870s. The average evaluation of the second-time NIBUT is equal to 10.0261s and the average evaluation of the second-time TBUT is equal to 10.0000s. The average evaluation of the third time NIBUT is 11s and the average evaluation of the third time TBUT is 10 s.
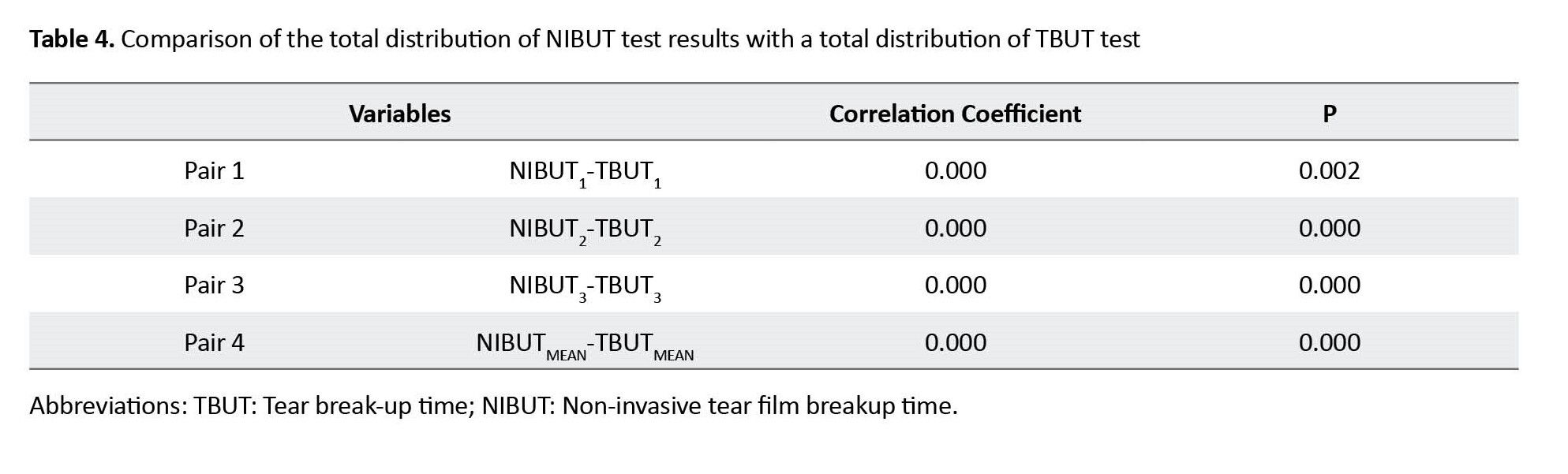
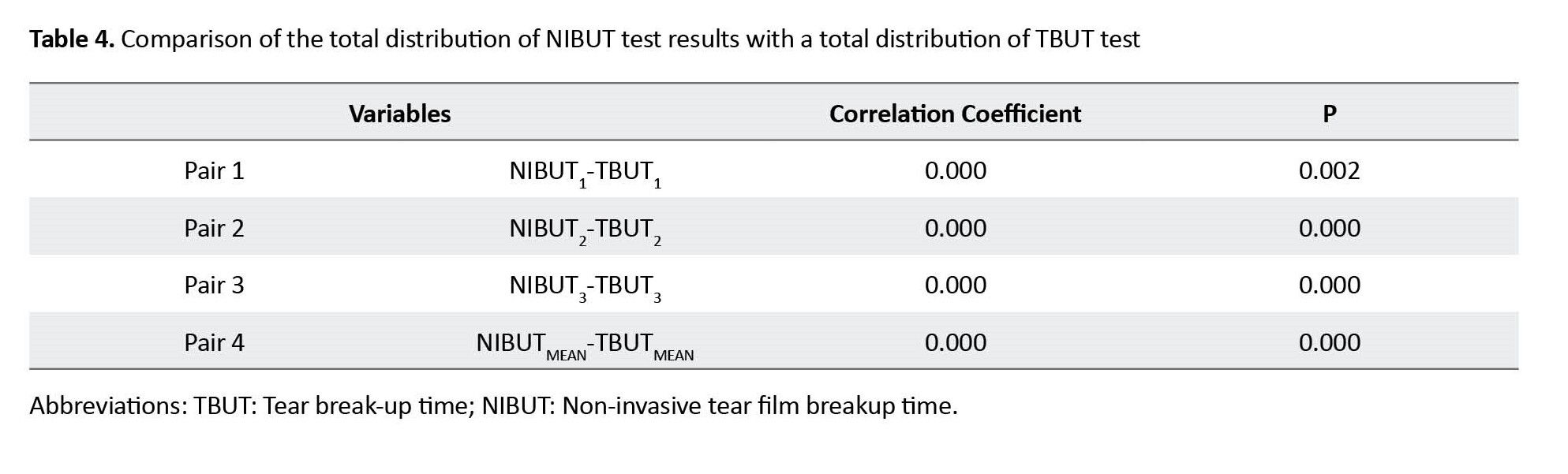
Comparison of the total distribution of the results of NIBUT test with a total distribution of TBUT test
According to Table 4, In the pair of NIBUT1 and TBUT1, the P value is equal to 0.002, in the pair of NIBUT2 and TBUT2 the P value is <0.001, in the pair of NIBUT3 and TBUT3 the P value is <0.001. Paired t-test in the case of the NIBUTMEAN and TBUTMEAN pair shows the P of these two variables is <0.001
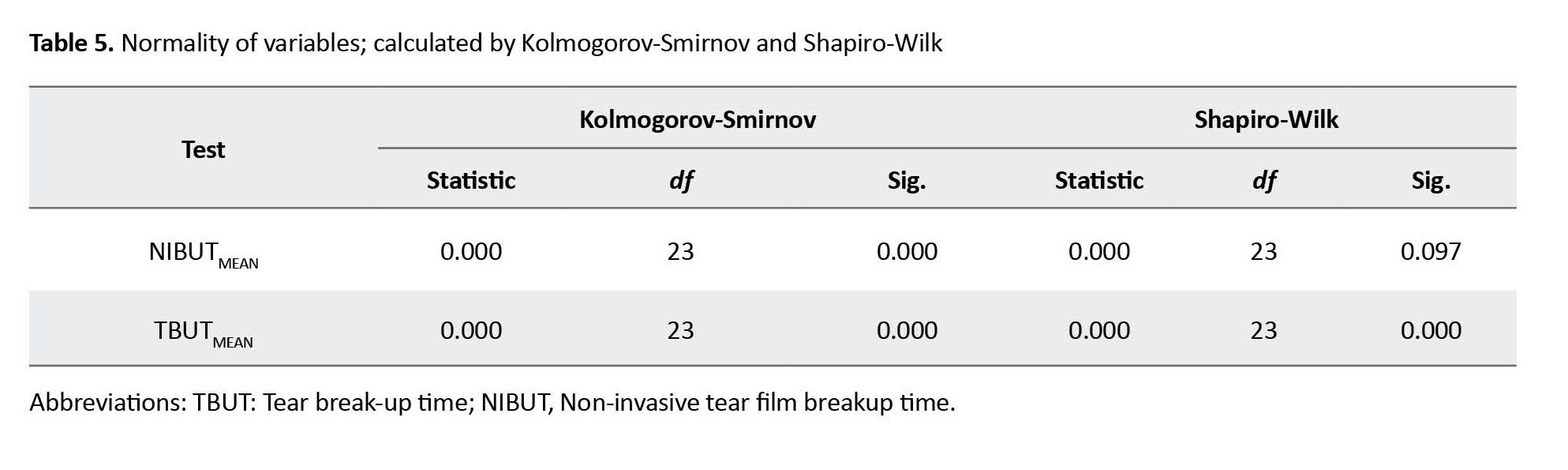
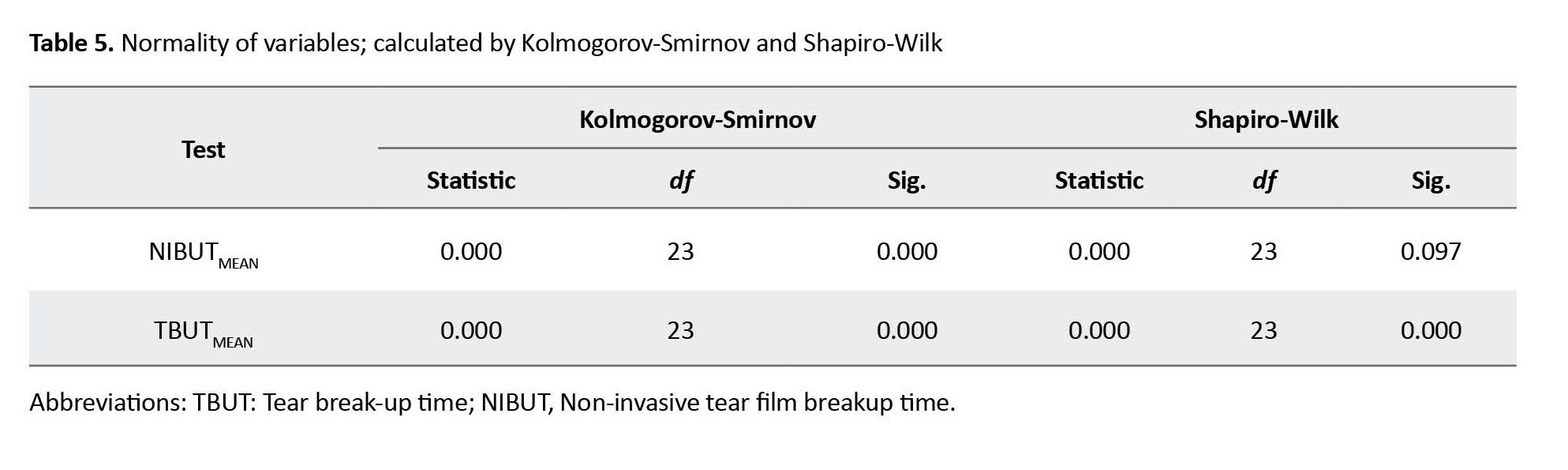
According to Table 5, In the tests of normality comparing NIBUTMEAN and TBUTMEAN with the Kolmogorov-Smirnov test, the significance level in both variables is 0.000. With the Shapiro-Wilk test, the level of significance in the NIBUTMEAN variable is 0.097 and in the TBUTMEAN variable is zero.
Discussion
Considering that it is essential to study the comparison of different methods of evaluating dry eye and since the evaluation of dry eye is done better with the "tear break up time" method [8], it is a priority to find the best method to evaluate dry eye with this method. To evaluate dry eye through the tear film breakup method, invasive (TBUT) or non-invasive (NIBUT) methods can be used. In recent years, several non-invasive methods have been introduced to evaluate dry eyes. It is essential to evaluate the efficiency of these methods and compare them with the conventional method. Researchers, such as Petal et al. and Mengher et al. have conducted research to show that instilling fluorescein in the eye disturbs the stability of the tear film [9] and suggest that the accuracy of the TBUT test be reconsidered. Also, many studies have been conducted on the efficiency of non-invasive imaging systems compared to previous common methods. For example, Savini examined anterior segment OCT devices [10], and Lomorrollio and his colleagues conducted studies on the MS-39 AS-OCT device in keratoconic eyes [11].
In this study, TBUT as a method that requires the use of fluorescein is an invasive method and the NIBUT method with AS-OCT MS-39 device is a non-invasive method.
According to the information in the tables in the findings and comparing their results, it was determined that the total average of NIBUT test results is equal to the total average of TBUT test results, and this value is 10 second. In addition, the average of the first times of NIBUT evaluation, the average of the second time, and the average of the third times of NIBUT evaluation were also equal to the average of the first times, the second times, and the third times of TBUT evaluation, respectively. In checking normality, according to the Shapiro-Wilk analysis, the TBUT method has a lower statistic than the NIBUT method in terms of normal distribution, and it can be said that the distribution of the TBUT method with the Shapiro-Wilk test is closer to the normal distribution; however, this difference does not exist between the normal distribution and the Kolmogorov-Smirnov method, and the normality statistic for both methods is zero. The average of both methods in the research is the same and the average of these two methods does not differ significantly from each other. In terms of comparing the performance of both methods in evaluating tear film, choosing the evaluation method with each of the methods is the patient's choice and depends on the doctor. If the patient does not have a problem with the aggressive conditions of the test and does not intend to pay a high price for the evaluation, the TBUT method is more suitable, however, if the invasiveness of the method causes problems for the doctor and the patient, it is better to use the NIBUT method. The NIBUT method with the AS-OCT MS-39 device uses the general principles of the TBUT method and differs from the TBUT method only in the case of the use of fluorescein, and therefore the similarity of the two methods is logical. Of course, it can be concluded from this comparison that the use of fluorescein in examining tear film does not have a significant effect on the tear film and does not affect the results. These results have been obtained in similar studies in the past years, for example, Cox et al. also measured NIBUT and TBUT using the Oculus Keratograph 4 device [12] and fluorescein TBUT and concluded that the difference in the average agreement between these two methods is close to zero [13]. Similarly, Amaechi and Osunwoke investigated the relationship between invasive and non-invasive methods of breaking the tear film (TBUT and NIBUT) in young people, and according to their research, no significant difference was observed between the results of these two methods in young people [14]. Of course, Lan et al. compared NIBUT with TBUT using the K5 keratograph, and showed that NIBUT values were higher than TBUT values [15]. This result is contrary to the results of the present study. Since the echograph K5 is the first generation of this type of device [16]. This discrepancy may be due to the lack of proper performance of the K5 echograph device in evaluating the tear film. Of course, considering that the device is very similar to the AS-OCT MS-39 device in terms of the test rules, it is better to carry out research to compare the K5 and AS-OCT MS-39 echograph devices in the future to automatically compare the effectiveness of these two devices in NIBUT.
Conclusion
According to the obtained results, it can be concluded that the MS-39 device is effective to evaluate NIBUT and the results of evaluating tear film with this device are consistent with the usual slit lamp TBUT method.
According to the results of this study, the following are suggested:
1- In the future, the prevalence of dry eye should be compared with both methods, and it is also better to compare some other non-invasive methods with the non-invasive NIBUT method with the AS-OCT MS-39 device to make a more accurate assessment of the differences between the non-invasive methods and the invasive TBUT method.
2- It is suggested to compare these two methods in people with corneal surface diseases and severe dry eyes. This research was conducted in the age group of 18 to 35 years, it is better to evaluate the lower and upper age groups in the future.
3- It is suggested to conduct studies to compare these two methods in people who have undergone refractive or ocular surface surgeries to make a more complete comparison of the agreement of the results of both methods.
Among the limitations of this study was the production of reflex tears after using fluorescein. This evaluation was not performed in people under 18 years old and people over 35 years old (so that the average is not affected by the age of the prevalence of dry eye) as well as due to the prevalence of dry eye in people with a corneal surface disease and people with a history of eye surgery, these people were not included in the study so that the average results would not be affected by factors affecting dry eyes and the sample would follow a normal distribution.
Ethical Considerations
Compliance with ethical guidelines
The tenets of the Helsinki Declaration were followed and informed consent was obtained from all participants. This research has received ethics code in the research committee of the Rehabilitation Faculty of the Iran University of Medical sciences (Code: IR.IUMS.REC.1400.954).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-forprofit sectors.
Authors' contributions
Conceptualization, resources, writing– orginal draft, writing review, project administration, investigation: Narges Firouzi; Supervision and editing review: Abbas Riazi; Counsulting, data curation, statistics curation: Reza Salehi. Methodology: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
Thanks for the the advice of dear colleague Alireza Jamali.
References
The human tear film has 3 layers, the outer layer of which is a lipid, which prevents the evaporation of the aqueous layer and maintains the thickness of the tear film, and its defect causes dry eyes [1]. Dry eye is a multifactorial disease related to tears and the ocular surface, which causes symptoms of eye discomfort, visual impairment, and tear film instability with the potential to damage the ocular surface. This problem is associated with increased osmolarity of the tear film and inflammation of the ocular surface [2].
Evaluating tear stability has several methods, one of which is the tear break-up time (TBUT) test. A TBUT of less than 10 second indicates tear film instability [3]. TBUT tests can be evaluated by invasive and non-invasive methods. The most common invasive method is the silt-lamp TBUT test [4]. This is done by applying a wet fluorescein strip to the bulbar conjunctiva and asking the patient to blink several times and then stare straight ahead. Using a wide light and a cobalt blue filter, the examiner records when he sees a black amoeba-shaped spot or more in the corneal tear film. The appearance of this black spot shows that the tear film is “broken” [5].
However, fluorescein has a destabilizing effect on the tear film and can underestimate the original values (causing the tear film to break earlier), in addition, it is more difficult to perform the TBUT test in some people. Some people react more strongly to the entry of any type of foreign substance (including fluorescein) and produce more intense reflex tears, which causes errors in the results. Seeing the tear film breaking with the naked eye causes a delay in recording the result, and a digital camera can provide a more accurate result. For this reason, in recent years, a tendency exists toward non-invasive methods to evaluate the tear film in natural conditions [3]. One of these non-invasive methods is non-invasive tear film breakup time (NIBUT) with the anterior segment-optical coherence tomography (AS-OCT) MS-39 device. Advanced analysis of tear film with AS-OCT MS-39 is possible according to the chief security officer (CSO) company via Placido disk technology, called NIBUT [6]. Since this feature is newly added to the OCT device, it is necessary to check whether the results provided by this device can be reliable in people who do not cooperate to perform the usual TBUT test with the slit lamp device, and these two methods can be replaced in necessary cases.
Since several different methods evaluate dry eye, each with advantages and disadvantages, it is essential to find a method that has the most advantages and the least disadvantages. Therefore, this study aims to investigate the performance of the MS-39 anterior segment OCT device in tear film examination compared to the TBUT test with a slit lamp.
Materials and Methods
The data collection method in this study is an observational clinical test method. The first device used is the anterior OCT MS-39 made by the Italian chief security officer (CSO) company, the 2019 version of which was used in this research. This device uses a Placido screen that lights up in red to evaluate the tear film. The working method of the device is that the device takes a video from the tear film to perform the test and records the time when the Placido rings collide as the result of the NIBUT test. The test is repeated three times with an interval of 30 second and then the average of the three results is taken. We waited 5 minutes to make sure that the tear film was restored. Then TBUT test was taken from the same eye of the same participant with a slit lamp device (Hagg-Streit model). In this way, fluorescein was instilled in the eye conjunctiva using a fluorescein tape. We waited for 3 second. Then the person was asked to blink three times and then stare forward behind the slit lamp without blinking (the person should not look at the light). We looked at the person’s eyes with a cobalt blue filter and the time of formation of black spots in the tear film was recorded as the result of the TBUT test in seconds. Thirty seconds after the end of this stage, the person was asked to blink three times and the test was repeated. The test was repeated three times. Then the results were averaged. first, the NIBUT method was performed with the MS-39 anterior segment OCT device because the TBUT method with a slit lamp is invasive and can affect the tear film and distort the results of subsequent tests.
The statistical methods in this study included descriptive methods of mean and data dispersion to average the results of two tests, analytical methods including paired t-tests to compare two methods together, and the distribution matching test of two methods with non-parametric tests. The statistical population included people aged 18 to 35 years who were referred to Negah ophthalmology hospital in Tehran City, Iran, and had no history of laser refractive surgery or disease involving the anterior segment. The sampling method in this study is the non-probability sampling method.
The calculation of the sample size according to Eroglu et al.’s article [7] and considering TBUT as the primary outcome has been calculated with the paired t method as follows: according to the above article and considering TAIL equal to 2, and the impact size equal to 0.897; If α err prob is considered at 0.05; The non-central parameter δ is 3.913, fundamental t is 2.101 and df is 18, which is 19 eyes according to the calculation of the sample size, which is obtained by considering the probability of a 20% drop out of the sample size of 23 eyes.
The inclusion criteria included people aged 18-35 years because this age group has better cooperation. Also, people who do not have a history of anterior eye surgery can enter the examination because no change was observed in the structure of their eyes. Also, people without a history of eye disease will provide more reliable results.
The exclusion criteria included any pre-test assessment that disturbs the stability of the tear film and lack of appropriate cooperation during the test.
Results
In this study, 23 eyes of 23 people were evaluated. The participants in this study included 16 women (69%) and 7 men (31%). The age range of people is 18 to 35 years with an average of 4.456±29.30 years.
Average results of NIBUT test in the studied subjects
According to Table 1, the total average results of the NIBUT test in participants is 10 s. The maximum amount of NIBUT is 17 s and the minimum amount is 4 s, that is, the range of changes of this variable is from 4 s to 17 s (13 s). The average results of the first NIBUT evaluation (NIBUT1) in the studied subjects are 10 s, the average results of the second NIBUT evaluation (NIBUT2) is 10.0261 s, and the average results of the third NIBUT evaluation (NIBUT3) is 11 s.
Average results of TBUT test in the studied subjects
According to Table 2, the average results of the TBUT test in the participants is 10 s. The maximum amount of TBUT is 17 s and the minimum is 4 s, that is, the range of changes of this variable is from 4 s to 17 s (13 s). The average results of the first evaluation of TBUT (TBUT1) in participants are 10.0870 s, the average results of the second evaluation of TBUT (TBUT2) in participants are 10 s, and the average results of the third evaluation of TBUT (TBUT3) in participants are also 10 s.
Total distribution of the results of the NIBUT test in the studied subjects
According to the Figure 1, the average NIBUT variable in this study is 10s. Its minimum value is 4 and its maximum value is 17s, and its standard deviation is 4s. The distribution histogram of this variable is shown (Figure 1).
Total distribution of the results of the TBUT in the studied subjects
According the Figure 2, the average TBUT variable in the studied subjects is 10 seconds. Its minimum value is 4s, its maximum value is 17s, and its standard deviation is 3s. The histogram of the distribution of this variable is shown (Figure 2).
Comparison of average results of the NIBUT with average results of TBUT
According to Table 3, The total average of both variables is equal to 10 seconds. The average evaluation of the first-time NIBUT is equal to 10s and the average evaluation of the first-time TBUT is equal to 10.0870s. The average evaluation of the second-time NIBUT is equal to 10.0261s and the average evaluation of the second-time TBUT is equal to 10.0000s. The average evaluation of the third time NIBUT is 11s and the average evaluation of the third time TBUT is 10 s.
Comparison of the total distribution of the results of NIBUT test with a total distribution of TBUT test
According to Table 4, In the pair of NIBUT1 and TBUT1, the P value is equal to 0.002, in the pair of NIBUT2 and TBUT2 the P value is <0.001, in the pair of NIBUT3 and TBUT3 the P value is <0.001. Paired t-test in the case of the NIBUTMEAN and TBUTMEAN pair shows the P of these two variables is <0.001
According to Table 5, In the tests of normality comparing NIBUTMEAN and TBUTMEAN with the Kolmogorov-Smirnov test, the significance level in both variables is 0.000. With the Shapiro-Wilk test, the level of significance in the NIBUTMEAN variable is 0.097 and in the TBUTMEAN variable is zero.
Discussion
Considering that it is essential to study the comparison of different methods of evaluating dry eye and since the evaluation of dry eye is done better with the "tear break up time" method [8], it is a priority to find the best method to evaluate dry eye with this method. To evaluate dry eye through the tear film breakup method, invasive (TBUT) or non-invasive (NIBUT) methods can be used. In recent years, several non-invasive methods have been introduced to evaluate dry eyes. It is essential to evaluate the efficiency of these methods and compare them with the conventional method. Researchers, such as Petal et al. and Mengher et al. have conducted research to show that instilling fluorescein in the eye disturbs the stability of the tear film [9] and suggest that the accuracy of the TBUT test be reconsidered. Also, many studies have been conducted on the efficiency of non-invasive imaging systems compared to previous common methods. For example, Savini examined anterior segment OCT devices [10], and Lomorrollio and his colleagues conducted studies on the MS-39 AS-OCT device in keratoconic eyes [11].
In this study, TBUT as a method that requires the use of fluorescein is an invasive method and the NIBUT method with AS-OCT MS-39 device is a non-invasive method.
According to the information in the tables in the findings and comparing their results, it was determined that the total average of NIBUT test results is equal to the total average of TBUT test results, and this value is 10 second. In addition, the average of the first times of NIBUT evaluation, the average of the second time, and the average of the third times of NIBUT evaluation were also equal to the average of the first times, the second times, and the third times of TBUT evaluation, respectively. In checking normality, according to the Shapiro-Wilk analysis, the TBUT method has a lower statistic than the NIBUT method in terms of normal distribution, and it can be said that the distribution of the TBUT method with the Shapiro-Wilk test is closer to the normal distribution; however, this difference does not exist between the normal distribution and the Kolmogorov-Smirnov method, and the normality statistic for both methods is zero. The average of both methods in the research is the same and the average of these two methods does not differ significantly from each other. In terms of comparing the performance of both methods in evaluating tear film, choosing the evaluation method with each of the methods is the patient's choice and depends on the doctor. If the patient does not have a problem with the aggressive conditions of the test and does not intend to pay a high price for the evaluation, the TBUT method is more suitable, however, if the invasiveness of the method causes problems for the doctor and the patient, it is better to use the NIBUT method. The NIBUT method with the AS-OCT MS-39 device uses the general principles of the TBUT method and differs from the TBUT method only in the case of the use of fluorescein, and therefore the similarity of the two methods is logical. Of course, it can be concluded from this comparison that the use of fluorescein in examining tear film does not have a significant effect on the tear film and does not affect the results. These results have been obtained in similar studies in the past years, for example, Cox et al. also measured NIBUT and TBUT using the Oculus Keratograph 4 device [12] and fluorescein TBUT and concluded that the difference in the average agreement between these two methods is close to zero [13]. Similarly, Amaechi and Osunwoke investigated the relationship between invasive and non-invasive methods of breaking the tear film (TBUT and NIBUT) in young people, and according to their research, no significant difference was observed between the results of these two methods in young people [14]. Of course, Lan et al. compared NIBUT with TBUT using the K5 keratograph, and showed that NIBUT values were higher than TBUT values [15]. This result is contrary to the results of the present study. Since the echograph K5 is the first generation of this type of device [16]. This discrepancy may be due to the lack of proper performance of the K5 echograph device in evaluating the tear film. Of course, considering that the device is very similar to the AS-OCT MS-39 device in terms of the test rules, it is better to carry out research to compare the K5 and AS-OCT MS-39 echograph devices in the future to automatically compare the effectiveness of these two devices in NIBUT.
Conclusion
According to the obtained results, it can be concluded that the MS-39 device is effective to evaluate NIBUT and the results of evaluating tear film with this device are consistent with the usual slit lamp TBUT method.
According to the results of this study, the following are suggested:
1- In the future, the prevalence of dry eye should be compared with both methods, and it is also better to compare some other non-invasive methods with the non-invasive NIBUT method with the AS-OCT MS-39 device to make a more accurate assessment of the differences between the non-invasive methods and the invasive TBUT method.
2- It is suggested to compare these two methods in people with corneal surface diseases and severe dry eyes. This research was conducted in the age group of 18 to 35 years, it is better to evaluate the lower and upper age groups in the future.
3- It is suggested to conduct studies to compare these two methods in people who have undergone refractive or ocular surface surgeries to make a more complete comparison of the agreement of the results of both methods.
Among the limitations of this study was the production of reflex tears after using fluorescein. This evaluation was not performed in people under 18 years old and people over 35 years old (so that the average is not affected by the age of the prevalence of dry eye) as well as due to the prevalence of dry eye in people with a corneal surface disease and people with a history of eye surgery, these people were not included in the study so that the average results would not be affected by factors affecting dry eyes and the sample would follow a normal distribution.
Ethical Considerations
Compliance with ethical guidelines
The tenets of the Helsinki Declaration were followed and informed consent was obtained from all participants. This research has received ethics code in the research committee of the Rehabilitation Faculty of the Iran University of Medical sciences (Code: IR.IUMS.REC.1400.954).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-forprofit sectors.
Authors' contributions
Conceptualization, resources, writing– orginal draft, writing review, project administration, investigation: Narges Firouzi; Supervision and editing review: Abbas Riazi; Counsulting, data curation, statistics curation: Reza Salehi. Methodology: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
Thanks for the the advice of dear colleague Alireza Jamali.
References
- Kanski JJ, Bowling B. Clinical ophthalmology: A systematic approach. Amsterdam: Elsevier Health Sciences; 2011. [Link]
- Bron AJ. The definition and classification of dry eye disease. In: Chan C, editor. Dry eye. Essentials in ophthalmology. Heidelberg: Springer; 2014. [DOI:10.1007/978-3-662-44106-0_1]
- Lemp MA, Hamill JR Jr. Factors affecting tear film breakup in normal eyes. Arch Ophthalmol. 1973; 89(2):103-5. [DOI:10.1001/archopht.1973.01000040105007] [PMID]
- McGinnigle S, Naroo SA, Eperjesi F. Evaluation of dry eye. Surv Ophthalmol. 2012; 57(4):293-316. [DOI:10.1016/j.survophthal.2011.11.003] [PMID]
- Grosvenor TP. Primary care optometry. Amsterdam: Elsevier Health Sciences; 2007. [Link]
- No author. MS-39 [Internet]. 2019. [Updated 29 January 2023]. Available from: [Link]
- Eroglu FC, Karalezli A, Dursun R. Is optical coherence tomography an effective device for evaluation of tear film meniscus in patients with acne rosacea? Eye. 2016; 30(4):545-52. [DOI:10.1038/eye.2015.277] [PMID] [PMCID]
- Serin D, Karsloğlu S, Kyan A, Alagöz G. A simple approach to the repeatability of the Schirmer test without anesthesia: Eyes open or closed? Cornea. 2007; 26(8):903-6. [DOI:10.1097/ICO.0b013e3180950083] [PMID]
- Yokoi N, Komuro A. Non-invasive methods of assessing the tear film. Exp Eye Res. 2004; 78(3):399-407. [DOI:10.1016/j.exer.2003.09.020] [PMID]
- Savini G, Schiano-Lomoriello D, Hoffer KJ. Repeatability of automatic measurements by a new anterior segment optical coherence tomographer combined with Placido topography and agreement with 2 Scheimpflug cameras. J Cataract Refract Surg. 2018; 44(4):471-8. [DOI:10.1016/j.jcrs.2018.02.015] [PMID]
- Schiano-Lomoriello D, Bono V, Abicca I, Savini G. Repeatability of anterior segment measurements by optical coherence tomography combined with Placido disk corneal topography in eyes with keratoconus. Sci Rep. 2020;10:1124. [DOI:10.1038/s41598-020-57926-7] [PMID] [PMCID]
- Jiang Y, Ye H, Xu J, Lu Y. Noninvasive keratograph assessment of tear film break-up time and location in patients with age-related cataracts and dry eye syndrome. J Int Med Res. 2014; 42(2):494-502. [DOI:10.1177/0300060513504701] [PMID]
- Cox SM, Nichols KK, Nichols JJ. Measures of tear film breakup. Optom Vis Sci. 2015; 92(9):e257-63. [DOI:10.1097/OPX.0000000000000648] [PMID] [PMCID]
- Amaechi O, Osunwoke C. The relation between invasive and non-invasive tear break-up time in young adults. J Niger Optom Assoc. 2004; 11:29-32. [DOI:10.4314/jnoa.v11i1.64443]
- Lan W, Lin L, Yang X, Yu M. Automatic noninvasive tear breakup time (TBUT) and conventional fluorescent TBUT. Optom Vis Sci. 2014; 91(12):1412-8. [DOI:10.1097/OPX.0000000000000418] [PMID]
- Haslina WH, Shah S, Naroo SA. The validity of corneal topography measurement by a new corneal topographer. Contact Lens Anterior Eye. 2015; 38:e43. [DOI:10.1016/j.clae.2014.11.075]
Type of Study: Research |
Subject:
Optometry
Received: 2022/09/6 | Accepted: 2022/10/15 | Published: 2022/02/3
Received: 2022/09/6 | Accepted: 2022/10/15 | Published: 2022/02/3