Volume 5, Issue 1 (Continuously Updated 2022)
Func Disabil J 2022, 5(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hakimzadeh Yazdi Z, Azimi Khorasani A, Riazi A. Validity and Version of the Vision-related Quality of Life Questionnaire. Func Disabil J 2022; 5 (1) : 57
URL: http://fdj.iums.ac.ir/article-1-184-en.html
URL: http://fdj.iums.ac.ir/article-1-184-en.html
1- Department of Optometry, School of Paramedical Sciences, Mashhad University of Medical Sciences, Mashhad, Iran.
2- Refractive Errors Research Center, Department of Optometry, School of Paramedical Sciences, Mashhad University of Medical Sciences, Mashhad, Iran.
3- Department of Optometry, Rehabilitation Research Center, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran. ,abbas.riazi@gmail.com
2- Refractive Errors Research Center, Department of Optometry, School of Paramedical Sciences, Mashhad University of Medical Sciences, Mashhad, Iran.
3- Department of Optometry, Rehabilitation Research Center, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 1122 kb]
(701 Downloads)
| Abstract (HTML) (2037 Views)
Full-Text: (785 Views)
Introduction
Vision has a significant impact on daily functioning, and social activities as well as affect physical and emotional well-being. Visual impairment can be caused by disease, trauma, or congenital and degenerative conditions [1]. Previous studies have shown that lifespan and quality of life (QoL) are significantly influenced by vision impairment [2]. This type of impairment is associated with falls, orientation and mobility problems, dependence on daily functioning, depression, life stress, and social isolation [2-6]. Visually impaired people are constantly involved in coping with challenges and needs for daily life [4] and most of them do not have adequate information and assistance to adapt to the vision impairment.
Assessment of visual function may not demonstrate all crucial aspects of vision impairment from the patient’s perspective, therefore, considerable interest is observed in using patient-reported outcomes (PRO) that depict functional vision (ability to perform vision-related activities) and vision-related quality of life (VRQoL) [7-14]. PRO is increasingly used to evaluate the benefits of treatment or interventions, patient satisfaction, cost-effectiveness, performance-related rehabilitation programs, and VRQoL [5, 15, 16]. Outcome measurement can be used for patients, caregivers, managers, government, and funding organizations [17-19].
Although no distinct agreement exists to describe QoL, it is generally accepted as a multidimensional patient’s perceived structure [9]. Also, this is a vague concept that is difficult to define and measure accurately [20]. According to the World Health Organization (WHO), QoL is “individuals perception of their position in life in the context of the culture and value systems in which they live and about their goals, expectations, standards, and concerns” [1, 9, 21, 22]. The VRQoL relates to those aspects of QoL affected by vision and is associated with the culture and values of the community, in which individuals live [22].
Currently, the importance of evaluating QoL to assess patient-centered outcomes in healthcare is widely accepted [23]. Low-vision services attempt to increase independence and improve the QoL of visually impaired patients [24]. For example, one of the main goals of glaucoma and age-related macular degeneration (AMD) treatment is to maintain and recover the patient’s performance of instrumental activities of daily living (IADL) and VRQoL [25]. Functional independence is assessed by the ability to perform IADLs [26, 27]. More recently, the focus has largely been on developing performance-based IADLs as outcome measures, rather than entirely relying on self-report instruments [26].
It is well known that family, community, and place of birth affect an individual’s views about defining QoL. Personality, collective memory, and history play an essential role in measuring QoL. Similarly, hereditary and genetic predispositions, environmental constraints and opportunities, and general government actions, expectations, requirements, rights, and obligations affect the definition of quality in individuals and places. Thus, a particular vision impairment assessment questionnaire is necessary for each community. Very few VRQoL instruments have been developed primarily in low-income countries [28-30]. Although various studies have not been conducted to evaluate the effect of visual impairment on Iranian people, some researchers in Iran try to translate some existing questionnaires to evaluate the QoL of visually impaired people [9, 31]. For instance, the 39-item National eye institute visual functioning questionnaire (NEI-VFQ-39) [9] is undoubtedly one of the most universally used questionnaires to evaluate the visually impaired QoL. However, it does not cover essential aspects of Iranian visually impaired lives, problems, and concerns, such as economic issues, public facilities, and cultural states. These aspects have been well addressed in the Iranian low vision questionnaire (ILVQ). This study designed and validated the credibility of an Iranian instrument assessing the impact of visual impairment on different aspects of life, such as daily vision-dependent activities, the effect of the environment, and social relationships.
Materials and Methods
This is a cross-sectional descriptive study that was conducted at Yazd blind society institute, under the supervision of the state welfare organization in Yazd Province, Iran. Informed consent was obtained from patients individually to participate in the study.
Participants
A total of 70 visually impaired and legally blind patients participated in this study, and 10 patients participated in the project for designing the instrument items. Later the data from the other 60 individuals were utilized in statistical analysis and results. The inclusion criteria included habitual distance visual acuity (VA) for low vision individuals logMAR 0.5–1.0(20/60-20/200) in the better eye and less than 1.0 logMAR (20/200) for legally blind people in the better eye, adult (≥18 years of age), informed consent, any type of ocular disease, no hearing and physical disabilities based on individual reports that they were able to manage a conversation in a quiet room [4, 16, 27, 32], and ability to speak Persian. The Snellen E chart at a distance of 4 m, which was converted to 6 m due to limited space, was used to determine the VA for each eye of the individuals.
Instrument development
Phase 1: Item selection
The first step in developing an assessment is to identify the content of the instrument’s items. Content development was conducted using existing ADL and VRQoL instruments. The items were designed based on WHO in three domains of independence, social relationships, and environment [33]. The reviewed questionnaires were the low vision quality-of-life questionnaire (LVQoL) [34], the national eye institute visual function questionnaire (NEI-VFQ25) [35], the impact of visual impairment (IVI) [36], the 10-item vision core measure 1 (VCM1) [12], veterans affairs low-vision visual functioning questionnaire (VA LV VFQ-48) [24], Timor Lest vision-specific quality-of-life instrument (TL-VSQoL) [28], Indian vision function questionnaire (IND-VFQ) [29], Melbourne low-vision ADL index (MLVAI) [32], and very low vision instrumental activities of daily living (IADL-VLV) [27]. A total of 43 items were selected for interviews with 10 visually impaired patients. The items were chosen from the above-mentioned instruments according to the authors’ knowledge, experiences, and viewpoints about the background, circumstances, and culture of the Iranian visually impaired. The face-to-face interview was conducted with the participants. Each item was read to them, and they were asked to express their opinions about each item by choosing an option from “very important,” “important,” and “not important” [27]. Finally, each person was asked, “What is the most important problem and concern that visual impairment has caused in your life?” [16]. The preliminary 35-item instrument was developed in two observation and interview sections (Table 1).
.jpg)
Phase 2: Response scale:
To specify the approximate time for the performance-based section of the questionnaire, three normal subjects aged 22, 30, and 41 years with simulated vision impairment participated and the time of finishing this part of the questionnaire was recorded. This section will take approximately 15-20 minutes to complete [32]. Items for VRQoL instruments tend to be graded based on the Likert scale which is usually graded according to a five-point score [11, 37] (Tables 2 and 3).
.jpg)
.jpg)
Phase 3: Psychometric pilot evaluation:
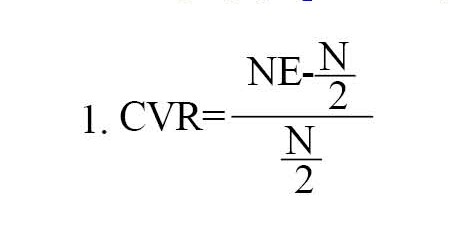
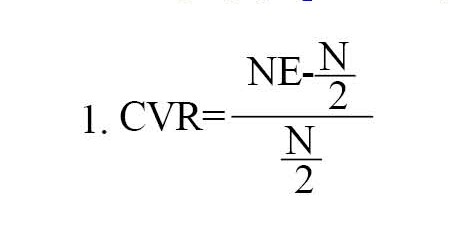
The instrument was designed for visually impaired individuals aged 18 and older [4, 27, 32, 38]. If subjects wear glasses daily, they should use their glasses to complete the questionnaire [35]. If the patients’ current glasses were significantly different from the new refraction, they would wear their previous glasses without any modification due to simulate the individual’s real-life conditions. The questionnaire should be conducted without any visual aids and devices [8]. We applied the standard methods [16, 32] for psychometric evaluation, including the determination of internal consistency, reliability, and validity. The preliminary ILVQ was distributed among 30 patients to assess the face and content validity of the questionnaire. Next, the preliminary ILVQ was administered to a group of six experts in low vision to use their opinions on the face validity of the instrument. Therefore, a semi-final ILVQ was developed. The content validity of the ILVQ was evaluated using Lawshe’s content validity ratio method. To this end, two methods of content validity ratio (CVR) and content validity index (CVI) methods were used. To determine the CVR, and necessity of items, the low vision specialists were asked to assess each item according to a three-part range of “essential”, “important, but not essential”, and “unnecessary”. The critical CVR value given by six experts is 1.00. Then, the answers are calculated by Equation 1. NE is the number of specialists who have chosen the “essential” option and N is the total number of specialists [39] (Equation 1).
To determine the CVI, and relevancy of items, the low vision specialists were asked to assess each item based on a four-part range of 1=not relevant, 2=somewhat relevant, 3=quite relevant, and 4=highly relevant. Then, for each item, the CVI is computed as the number of experts giving a rating of 3 or 4, divided by the number of experts. The acceptable CVI value of six experts must be at least 0.83 [40]. To construct validity, factor analysis was used. Principal component analysis and varimax rotation were used to conduct factor analysis. Internal reliability was evaluated using Cronbach’s alpha coefficient, as regards external reliability and stability, the test-retest analyses were conducted by re-performing the test on a group of 30 subjects from the research community twice at 15-day intervals. The intraclass correlation coefficient method was also used to evaluate the repeatability.
Results
In this study, 43(71.7%) females and 17(28.3%) males participated. The age range of people was 20 to 60 years (31.28±8.37). The visual acuity ranged from 20/60 to no light perception (NLP). The minimum and maximum scores of the ILVQ are 20 and 112, respectively, with potential scores from zero to 128. The Mean±SD total raw score was 60.61±24.01 and the Mean±SD scores of the observation and interview sections were 29.56±12.84 and 31.10±12.13, respectively. Table 1 lists Mean±SD scores from each item. The average score of ILVQ was higher in visually impaired males (65.41±27.11) than in females (56.91±23.81). However, this difference was not significant statistically. Table 4 lists the demographic characteristics of the participants.
.jpg)
Validity: The content validity of the questionnaire was assessed using Lawshe’s content validity ratio method. After calculating CVR and CVI, items 6, 7, and 11 (telling time with a wristwatch and wall clock as well as threading a needle) were omitted. The CVR and CVI’s calculated values indicate that the ILVQ’s content validity is sufficient for research. For construct validity, factor analysis was utilized. To conduct factor analysis, the principal component analysis with varimax rotation was used. The Kaiser-Meyer-Oaklin (KMO) index was measured to be 0.8, which proved the sampling adequacy and the suitable sample size. The results of factor analysis identified five components that specified 78% of the variance and variability of variables. The three components (the first, the second, and the third) were extracted that had the highest internal reliability. The second factor expressed observation items and areas of the independence level. The first factor included items relevant to the environment and the individual’s ability to conduct activities in the environment. The third factor included items in social relationships.
Internal Reliability: Cronbach’s alpha was determined to evaluate the internal reliability of the instrument. Cronbach’s alpha is reliable when factor analysis has already been done which is considered in this study [10]. Cronbach’s alpha values above 0.70 demonstrate satisfying internal construct validity. In this study, the internal reliability was calculated at 0.96 with Cronbach’s alpha coefficient. The Cronbach’s alpha coefficient of observation and interview sections were computed at 0.95 and 0.93, respectively.
Reliability: To assess the external reliability and stability, the test-rtest method was re-performing on a group of 30 people from the research community twice at 15-day intervals. The correlation coefficient of both tests was calculated. Most of the items had a correlation coefficient above 0.90, and the correlation coefficient for the total score of the two stages was 0.94 (P<0.001). Thus, the instrument has satisfactory external reliability and stability. Furthermore, the results of comparing the average test-retest scores (60.61±24.01 and 61.12±23.87, respectively) of the participants did not show a considerable difference, which demonstrates the external reliability. To evaluate repeatability, the intraclass correlation coefficient (ICC) method was performed. The value of this index was calculated at 0.96 (P<0.001), which demonstrates the high repeatability of the ILVQ.
Discussion
In this study, the method of development of an Iranian low vision quality of life questionnaire (ILVQ), and its validity, and reliability are reported. According to comparing the Mean±SD score of total test scores in men and women, ILVQ is not gender-dependent and can be used to evaluate QoL among visually impaired people regardless of their gender. Similarly, the LVQoL, one of the most reliable questionnaires to evaluate the QoL in visually impaired people, is independent of gender and other demographic information [34].
The ability to use credit cards in different situations, such as card readers and ATMs, is necessary not only for every individual but also for visually impaired people in different parts of the worlds. This problem has not been well addressed in many vision-related functional and QoL questionnaires. Economic conditions and associated issues may cause many problems, and accordingly, may cause insecurities, for instance, fear of robbery. Many visually impaired people reported the misuse of their credit cards. They believed that this problem resulted from their inability to use credit cards independently. This can result in other problems, such as creating a sense of helplessness and blaming oneself and others partially sighted. Furthermore, it can lead to increased dependence of low-vision individuals on their relatives. As a result, these types of difficulties have been well addressed in the ILVQ.
The ability of people with vision impairment to afford the economic costs of their lives is essential. In many cases, the origin of vision loss can be poverty, in a situation where a person has not been able to cure their eye disease due to its costs, and the resulting visual impairment. Visually impaired people in Iran are mainly dependent on their relatives. And economic pressure is imposed on the family. Economic issues have not been considered in LVQoL [34], NEI-VFQ-25 [35], IVI [36], VCM1 [12], and any other well-known VRQoL instruments. The ILVQ has mainly assessed this problem with two items, “having a job” and the “ability to cover living expenses”.
It is essential to know that life in Iran is more collected and less independent compared to developed countries. People are inextricably linked with other family members, relatives, acquaintances, friends, neighbors, and related citizens. Iranian visually impaired people do not believe much in an independent life. Therefore, they are not encouraged to be independent and do personal activities and independence. In many cases, they live with their parents or a close family member for the rest of their lives. Educating parents and relatives to encourage the visually impaired to live independently is not considered as an item in many questionnaires, such as LVQoL [34], NEI-VFQ-25 [35], IVI [36], VCM1 [12] which is due to the difference in attitudes and culture of each society towards disability. This concern has been well addressed in the ILVQ.
Although, almost all VRQoLs include time announcements with a wall clock, wristwatch, and thread needles as important items, most Iranian visually impaired people did not consider these three items as requirements! The reason for removing the first two items is the development of technologies. Using mobile phones has become very common these days all over the world. “We check the time using cell phones,” said the visually impaired Iranians. Therefore, these items were removed and items about mobile phone use were added. Mobile phone usability was not included in previous VRQoLs. For visually impaired people, it is essential to use mobile phones and the internet to connect with others, friends, entertainment, and information. Currently, many Iranian visually impaired people use a mobile phone as a magnifier. Many applications for magnification can be installed into mobile phones and used them as a magnifier. Visually impaired people learned to take a picture of any text and then use magnification facilities on cell phones for easy reading. Finally, the reason for removing thread needles is that many Iranian visually impaired people do not sew and do not need thread needles because they live with their relatives and others do for them. Therefore, these items are not necessary for our questionnaire. It should be noted that the questionnaires need to be updated as lifestyle changes over time.
The insecurity and risks caused by accidents in unfamiliar outdoor environments are one of the consequences of vision impairment [41]. In many areas in different cities in Iran, the needs of the partially sighted have not been considered, which creates potential risks. Hazards, such as falling and accidents can induce physical disability and increase mortality. Any unsafe environment, including non-standard structures, uneven passages, and sidewalks, construction operations on passages and streets, possible potholes in alleys and streets, the possibility of collisions with vehicles and shop signs, lack of special paths for the visually impaired in office buildings, etc. pose a danger to the visually impaired people. While no item exists about the risk of hazard and its relevant insecurity in the well-known questionnaires, including LVQoL [34] and NEI-VFQ-25 [35], ILVQ has been considered similar to IVI [36] and VCM1 [12].
The possibility of using public transportation is another essential item for visually impaired people in Iran. This item has not been included in some reliable instruments, such as NEI-VFQ-25 [35] and LVQoL [34]. This could result from the advanced and safe public transportation as well as attention to the needs of the low vision people in the transportation system in developed countries. However, many public transportation stations and platforms, such as buses and subway trains, are not modified for visually impaired individuals in Iran. The ability to utilize public transportation plays a key role in the lifestyle of visually impaired people. They can participate more in society and have education and entertainment, socialize with others, and so forth, which affects mentality, mental health, and QoL. This problem is vital for visually impaired Iranians and therefore it is well addressed in the ILVQ. Moreover, some items in ILVQ, such as climbing up and down stairs, crossing the street, and going shopping are similar to other VRQoL instruments, including LVQoL [34] and IVI [36]. Among these similar items, crossing the street is a crucial issue for low vision individuals. The potential dangers that this poses to them, including dysfunction, disability, and fear of falls and fractions, must be considered. Lack of safety in sidewalk for pedestrians as well as the shortage of suitable routes for partially sighted to cross the street is one of the basic problems in Iran that is considered in the ILVQ. These kinds of difficulties for visually impaired Iranian have been reported in other studies [41].
According to the average score obtained for each question, it seems that the environmental domain has caused the greatest level of disability and concern in visually impaired people in Iran. Therefore, one of the most critical problems for Iranian visually impaired people is performing activities in their environment without dependency on others. This finding indicates basic planning and attitude to evaluate environmental conditions rather than visual conditions. It is not worthwhile to enhance the QoL of these people by just examining their visual conditions, measuring their ability to conduct daily routines, and prescribing low-vision optical devices. It is essential to consider the environmental difficulties for this group of people. In other words, environmental modification is necessary.
Conclusion
The 32-item instrument (ILVQ) was created with observation and interview sections, which is highly valid and reliable to assess the quality of life in the general low vision population in Iran as well as culturally similar communities.
Clinical Relevance: Much vision-related quality of life (VRQoL) questionnaires have already been developed. However, some items of these instruments did not work due to advanced technologies.
Ethical Considerations
Compliance with ethical guidelines
The research was approved by the Research Ethics Committee of Mashhad University of Medical Sciences (Code IR.MUMS.REC.1396.138).
Funding
This study was supported by the Iran University of Medical Sciences.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank Yazd blind society institute and the participants for their cooperation and time.
References
Vision has a significant impact on daily functioning, and social activities as well as affect physical and emotional well-being. Visual impairment can be caused by disease, trauma, or congenital and degenerative conditions [1]. Previous studies have shown that lifespan and quality of life (QoL) are significantly influenced by vision impairment [2]. This type of impairment is associated with falls, orientation and mobility problems, dependence on daily functioning, depression, life stress, and social isolation [2-6]. Visually impaired people are constantly involved in coping with challenges and needs for daily life [4] and most of them do not have adequate information and assistance to adapt to the vision impairment.
Assessment of visual function may not demonstrate all crucial aspects of vision impairment from the patient’s perspective, therefore, considerable interest is observed in using patient-reported outcomes (PRO) that depict functional vision (ability to perform vision-related activities) and vision-related quality of life (VRQoL) [7-14]. PRO is increasingly used to evaluate the benefits of treatment or interventions, patient satisfaction, cost-effectiveness, performance-related rehabilitation programs, and VRQoL [5, 15, 16]. Outcome measurement can be used for patients, caregivers, managers, government, and funding organizations [17-19].
Although no distinct agreement exists to describe QoL, it is generally accepted as a multidimensional patient’s perceived structure [9]. Also, this is a vague concept that is difficult to define and measure accurately [20]. According to the World Health Organization (WHO), QoL is “individuals perception of their position in life in the context of the culture and value systems in which they live and about their goals, expectations, standards, and concerns” [1, 9, 21, 22]. The VRQoL relates to those aspects of QoL affected by vision and is associated with the culture and values of the community, in which individuals live [22].
Currently, the importance of evaluating QoL to assess patient-centered outcomes in healthcare is widely accepted [23]. Low-vision services attempt to increase independence and improve the QoL of visually impaired patients [24]. For example, one of the main goals of glaucoma and age-related macular degeneration (AMD) treatment is to maintain and recover the patient’s performance of instrumental activities of daily living (IADL) and VRQoL [25]. Functional independence is assessed by the ability to perform IADLs [26, 27]. More recently, the focus has largely been on developing performance-based IADLs as outcome measures, rather than entirely relying on self-report instruments [26].
It is well known that family, community, and place of birth affect an individual’s views about defining QoL. Personality, collective memory, and history play an essential role in measuring QoL. Similarly, hereditary and genetic predispositions, environmental constraints and opportunities, and general government actions, expectations, requirements, rights, and obligations affect the definition of quality in individuals and places. Thus, a particular vision impairment assessment questionnaire is necessary for each community. Very few VRQoL instruments have been developed primarily in low-income countries [28-30]. Although various studies have not been conducted to evaluate the effect of visual impairment on Iranian people, some researchers in Iran try to translate some existing questionnaires to evaluate the QoL of visually impaired people [9, 31]. For instance, the 39-item National eye institute visual functioning questionnaire (NEI-VFQ-39) [9] is undoubtedly one of the most universally used questionnaires to evaluate the visually impaired QoL. However, it does not cover essential aspects of Iranian visually impaired lives, problems, and concerns, such as economic issues, public facilities, and cultural states. These aspects have been well addressed in the Iranian low vision questionnaire (ILVQ). This study designed and validated the credibility of an Iranian instrument assessing the impact of visual impairment on different aspects of life, such as daily vision-dependent activities, the effect of the environment, and social relationships.
Materials and Methods
This is a cross-sectional descriptive study that was conducted at Yazd blind society institute, under the supervision of the state welfare organization in Yazd Province, Iran. Informed consent was obtained from patients individually to participate in the study.
Participants
A total of 70 visually impaired and legally blind patients participated in this study, and 10 patients participated in the project for designing the instrument items. Later the data from the other 60 individuals were utilized in statistical analysis and results. The inclusion criteria included habitual distance visual acuity (VA) for low vision individuals logMAR 0.5–1.0(20/60-20/200) in the better eye and less than 1.0 logMAR (20/200) for legally blind people in the better eye, adult (≥18 years of age), informed consent, any type of ocular disease, no hearing and physical disabilities based on individual reports that they were able to manage a conversation in a quiet room [4, 16, 27, 32], and ability to speak Persian. The Snellen E chart at a distance of 4 m, which was converted to 6 m due to limited space, was used to determine the VA for each eye of the individuals.
Instrument development
Phase 1: Item selection
The first step in developing an assessment is to identify the content of the instrument’s items. Content development was conducted using existing ADL and VRQoL instruments. The items were designed based on WHO in three domains of independence, social relationships, and environment [33]. The reviewed questionnaires were the low vision quality-of-life questionnaire (LVQoL) [34], the national eye institute visual function questionnaire (NEI-VFQ25) [35], the impact of visual impairment (IVI) [36], the 10-item vision core measure 1 (VCM1) [12], veterans affairs low-vision visual functioning questionnaire (VA LV VFQ-48) [24], Timor Lest vision-specific quality-of-life instrument (TL-VSQoL) [28], Indian vision function questionnaire (IND-VFQ) [29], Melbourne low-vision ADL index (MLVAI) [32], and very low vision instrumental activities of daily living (IADL-VLV) [27]. A total of 43 items were selected for interviews with 10 visually impaired patients. The items were chosen from the above-mentioned instruments according to the authors’ knowledge, experiences, and viewpoints about the background, circumstances, and culture of the Iranian visually impaired. The face-to-face interview was conducted with the participants. Each item was read to them, and they were asked to express their opinions about each item by choosing an option from “very important,” “important,” and “not important” [27]. Finally, each person was asked, “What is the most important problem and concern that visual impairment has caused in your life?” [16]. The preliminary 35-item instrument was developed in two observation and interview sections (Table 1).
.jpg)
Phase 2: Response scale:
To specify the approximate time for the performance-based section of the questionnaire, three normal subjects aged 22, 30, and 41 years with simulated vision impairment participated and the time of finishing this part of the questionnaire was recorded. This section will take approximately 15-20 minutes to complete [32]. Items for VRQoL instruments tend to be graded based on the Likert scale which is usually graded according to a five-point score [11, 37] (Tables 2 and 3).
.jpg)
.jpg)
Phase 3: Psychometric pilot evaluation:
The instrument was designed for visually impaired individuals aged 18 and older [4, 27, 32, 38]. If subjects wear glasses daily, they should use their glasses to complete the questionnaire [35]. If the patients’ current glasses were significantly different from the new refraction, they would wear their previous glasses without any modification due to simulate the individual’s real-life conditions. The questionnaire should be conducted without any visual aids and devices [8]. We applied the standard methods [16, 32] for psychometric evaluation, including the determination of internal consistency, reliability, and validity. The preliminary ILVQ was distributed among 30 patients to assess the face and content validity of the questionnaire. Next, the preliminary ILVQ was administered to a group of six experts in low vision to use their opinions on the face validity of the instrument. Therefore, a semi-final ILVQ was developed. The content validity of the ILVQ was evaluated using Lawshe’s content validity ratio method. To this end, two methods of content validity ratio (CVR) and content validity index (CVI) methods were used. To determine the CVR, and necessity of items, the low vision specialists were asked to assess each item according to a three-part range of “essential”, “important, but not essential”, and “unnecessary”. The critical CVR value given by six experts is 1.00. Then, the answers are calculated by Equation 1. NE is the number of specialists who have chosen the “essential” option and N is the total number of specialists [39] (Equation 1).
To determine the CVI, and relevancy of items, the low vision specialists were asked to assess each item based on a four-part range of 1=not relevant, 2=somewhat relevant, 3=quite relevant, and 4=highly relevant. Then, for each item, the CVI is computed as the number of experts giving a rating of 3 or 4, divided by the number of experts. The acceptable CVI value of six experts must be at least 0.83 [40]. To construct validity, factor analysis was used. Principal component analysis and varimax rotation were used to conduct factor analysis. Internal reliability was evaluated using Cronbach’s alpha coefficient, as regards external reliability and stability, the test-retest analyses were conducted by re-performing the test on a group of 30 subjects from the research community twice at 15-day intervals. The intraclass correlation coefficient method was also used to evaluate the repeatability.
Results
In this study, 43(71.7%) females and 17(28.3%) males participated. The age range of people was 20 to 60 years (31.28±8.37). The visual acuity ranged from 20/60 to no light perception (NLP). The minimum and maximum scores of the ILVQ are 20 and 112, respectively, with potential scores from zero to 128. The Mean±SD total raw score was 60.61±24.01 and the Mean±SD scores of the observation and interview sections were 29.56±12.84 and 31.10±12.13, respectively. Table 1 lists Mean±SD scores from each item. The average score of ILVQ was higher in visually impaired males (65.41±27.11) than in females (56.91±23.81). However, this difference was not significant statistically. Table 4 lists the demographic characteristics of the participants.
.jpg)
Validity: The content validity of the questionnaire was assessed using Lawshe’s content validity ratio method. After calculating CVR and CVI, items 6, 7, and 11 (telling time with a wristwatch and wall clock as well as threading a needle) were omitted. The CVR and CVI’s calculated values indicate that the ILVQ’s content validity is sufficient for research. For construct validity, factor analysis was utilized. To conduct factor analysis, the principal component analysis with varimax rotation was used. The Kaiser-Meyer-Oaklin (KMO) index was measured to be 0.8, which proved the sampling adequacy and the suitable sample size. The results of factor analysis identified five components that specified 78% of the variance and variability of variables. The three components (the first, the second, and the third) were extracted that had the highest internal reliability. The second factor expressed observation items and areas of the independence level. The first factor included items relevant to the environment and the individual’s ability to conduct activities in the environment. The third factor included items in social relationships.
Internal Reliability: Cronbach’s alpha was determined to evaluate the internal reliability of the instrument. Cronbach’s alpha is reliable when factor analysis has already been done which is considered in this study [10]. Cronbach’s alpha values above 0.70 demonstrate satisfying internal construct validity. In this study, the internal reliability was calculated at 0.96 with Cronbach’s alpha coefficient. The Cronbach’s alpha coefficient of observation and interview sections were computed at 0.95 and 0.93, respectively.
Reliability: To assess the external reliability and stability, the test-rtest method was re-performing on a group of 30 people from the research community twice at 15-day intervals. The correlation coefficient of both tests was calculated. Most of the items had a correlation coefficient above 0.90, and the correlation coefficient for the total score of the two stages was 0.94 (P<0.001). Thus, the instrument has satisfactory external reliability and stability. Furthermore, the results of comparing the average test-retest scores (60.61±24.01 and 61.12±23.87, respectively) of the participants did not show a considerable difference, which demonstrates the external reliability. To evaluate repeatability, the intraclass correlation coefficient (ICC) method was performed. The value of this index was calculated at 0.96 (P<0.001), which demonstrates the high repeatability of the ILVQ.
Discussion
In this study, the method of development of an Iranian low vision quality of life questionnaire (ILVQ), and its validity, and reliability are reported. According to comparing the Mean±SD score of total test scores in men and women, ILVQ is not gender-dependent and can be used to evaluate QoL among visually impaired people regardless of their gender. Similarly, the LVQoL, one of the most reliable questionnaires to evaluate the QoL in visually impaired people, is independent of gender and other demographic information [34].
The ability to use credit cards in different situations, such as card readers and ATMs, is necessary not only for every individual but also for visually impaired people in different parts of the worlds. This problem has not been well addressed in many vision-related functional and QoL questionnaires. Economic conditions and associated issues may cause many problems, and accordingly, may cause insecurities, for instance, fear of robbery. Many visually impaired people reported the misuse of their credit cards. They believed that this problem resulted from their inability to use credit cards independently. This can result in other problems, such as creating a sense of helplessness and blaming oneself and others partially sighted. Furthermore, it can lead to increased dependence of low-vision individuals on their relatives. As a result, these types of difficulties have been well addressed in the ILVQ.
The ability of people with vision impairment to afford the economic costs of their lives is essential. In many cases, the origin of vision loss can be poverty, in a situation where a person has not been able to cure their eye disease due to its costs, and the resulting visual impairment. Visually impaired people in Iran are mainly dependent on their relatives. And economic pressure is imposed on the family. Economic issues have not been considered in LVQoL [34], NEI-VFQ-25 [35], IVI [36], VCM1 [12], and any other well-known VRQoL instruments. The ILVQ has mainly assessed this problem with two items, “having a job” and the “ability to cover living expenses”.
It is essential to know that life in Iran is more collected and less independent compared to developed countries. People are inextricably linked with other family members, relatives, acquaintances, friends, neighbors, and related citizens. Iranian visually impaired people do not believe much in an independent life. Therefore, they are not encouraged to be independent and do personal activities and independence. In many cases, they live with their parents or a close family member for the rest of their lives. Educating parents and relatives to encourage the visually impaired to live independently is not considered as an item in many questionnaires, such as LVQoL [34], NEI-VFQ-25 [35], IVI [36], VCM1 [12] which is due to the difference in attitudes and culture of each society towards disability. This concern has been well addressed in the ILVQ.
Although, almost all VRQoLs include time announcements with a wall clock, wristwatch, and thread needles as important items, most Iranian visually impaired people did not consider these three items as requirements! The reason for removing the first two items is the development of technologies. Using mobile phones has become very common these days all over the world. “We check the time using cell phones,” said the visually impaired Iranians. Therefore, these items were removed and items about mobile phone use were added. Mobile phone usability was not included in previous VRQoLs. For visually impaired people, it is essential to use mobile phones and the internet to connect with others, friends, entertainment, and information. Currently, many Iranian visually impaired people use a mobile phone as a magnifier. Many applications for magnification can be installed into mobile phones and used them as a magnifier. Visually impaired people learned to take a picture of any text and then use magnification facilities on cell phones for easy reading. Finally, the reason for removing thread needles is that many Iranian visually impaired people do not sew and do not need thread needles because they live with their relatives and others do for them. Therefore, these items are not necessary for our questionnaire. It should be noted that the questionnaires need to be updated as lifestyle changes over time.
The insecurity and risks caused by accidents in unfamiliar outdoor environments are one of the consequences of vision impairment [41]. In many areas in different cities in Iran, the needs of the partially sighted have not been considered, which creates potential risks. Hazards, such as falling and accidents can induce physical disability and increase mortality. Any unsafe environment, including non-standard structures, uneven passages, and sidewalks, construction operations on passages and streets, possible potholes in alleys and streets, the possibility of collisions with vehicles and shop signs, lack of special paths for the visually impaired in office buildings, etc. pose a danger to the visually impaired people. While no item exists about the risk of hazard and its relevant insecurity in the well-known questionnaires, including LVQoL [34] and NEI-VFQ-25 [35], ILVQ has been considered similar to IVI [36] and VCM1 [12].
The possibility of using public transportation is another essential item for visually impaired people in Iran. This item has not been included in some reliable instruments, such as NEI-VFQ-25 [35] and LVQoL [34]. This could result from the advanced and safe public transportation as well as attention to the needs of the low vision people in the transportation system in developed countries. However, many public transportation stations and platforms, such as buses and subway trains, are not modified for visually impaired individuals in Iran. The ability to utilize public transportation plays a key role in the lifestyle of visually impaired people. They can participate more in society and have education and entertainment, socialize with others, and so forth, which affects mentality, mental health, and QoL. This problem is vital for visually impaired Iranians and therefore it is well addressed in the ILVQ. Moreover, some items in ILVQ, such as climbing up and down stairs, crossing the street, and going shopping are similar to other VRQoL instruments, including LVQoL [34] and IVI [36]. Among these similar items, crossing the street is a crucial issue for low vision individuals. The potential dangers that this poses to them, including dysfunction, disability, and fear of falls and fractions, must be considered. Lack of safety in sidewalk for pedestrians as well as the shortage of suitable routes for partially sighted to cross the street is one of the basic problems in Iran that is considered in the ILVQ. These kinds of difficulties for visually impaired Iranian have been reported in other studies [41].
According to the average score obtained for each question, it seems that the environmental domain has caused the greatest level of disability and concern in visually impaired people in Iran. Therefore, one of the most critical problems for Iranian visually impaired people is performing activities in their environment without dependency on others. This finding indicates basic planning and attitude to evaluate environmental conditions rather than visual conditions. It is not worthwhile to enhance the QoL of these people by just examining their visual conditions, measuring their ability to conduct daily routines, and prescribing low-vision optical devices. It is essential to consider the environmental difficulties for this group of people. In other words, environmental modification is necessary.
Conclusion
The 32-item instrument (ILVQ) was created with observation and interview sections, which is highly valid and reliable to assess the quality of life in the general low vision population in Iran as well as culturally similar communities.
Clinical Relevance: Much vision-related quality of life (VRQoL) questionnaires have already been developed. However, some items of these instruments did not work due to advanced technologies.
Ethical Considerations
Compliance with ethical guidelines
The research was approved by the Research Ethics Committee of Mashhad University of Medical Sciences (Code IR.MUMS.REC.1396.138).
Funding
This study was supported by the Iran University of Medical Sciences.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank Yazd blind society institute and the participants for their cooperation and time.
References
- Adigun K, Oluleye TS, Ladipo MM, Olowookere SA. Quality of life in patients with visual impairment in Ibadan: A clinical study in primary care. J Multidiscip Healthc. 2014; 7:173-8. [DOI:10.2147/JMDH.S51359] [PMID] [PMCID]
- Peacock S, Misajon R, Iezzi A, Richardson J, Hawthorne G, Keeffe J. Vision and quality of life: Development of methods for the VisQoL vision-related utility instrument. Ophthalmic Epidemiol. 2008; 15(4):218-23. [DOI:10.1080/09286580801979417] [PMID] [PMCID]
- Pondorfer SG, Terheyden JH, Overhoff H, Stasch-Bouws J, Holz FG, Finger RP. Development of the vision impairment in low luminance questionnaire. Transl Vis Sci Technol. 2021; 10(1):5. [DOI:10.1167/tvst.10.1.5] [PMID] [PMCID]
- Sturrock BA, Xie J, Holloway EE, Lamoureux EL, Keeffe JE, Fenwick EK, et al. The influence of coping on vision-related quality of life in patients with low vision: A prospective longitudinal study. Invest Ophthalmol Vis Sci. 2015; 56(4):2416-22. [DOI:10.1167/iovs.14-16223] [PMID]
- Finger RP, Fenwick E, Marella M, Dirani M, Holz FG, Chiang PP-C, et al. The impact of vision impairment on vision-specific quality of life in Germany. Invest Ophthalmol Vis Sci. 2011; 52(6):3613-9. [DOI:10.1167/iovs.10-7127] [PMID]
- Hassell JB, Lamoureux EL, Keeffe JE. Impact of age related macular degeneration on quality of life. Br J Ophthalmol. 2006; 90(5):593-6. [DOI:10.1136/bjo.2005.086595] [PMID] [PMCID]
- Bennett CR, Bex PJ, Bauer CM, Merabet LB. The assessment of visual function and functional vision. Semin Pediatr Neurol. 2019; 31:30-40 [DOI:10.1016/j.spen.2019.05.006] [PMID] [PMCID]
- Riazi A, Dain SJ, Boon MY, Bridge C. Innovative strategies for adaptation to loss of vision. Clin Exp Optom. 2011; 94(1):98-102. [DOI:10.1111/j.1444-0938.2010.00543.x] [PMID]
- Asgari S, Hashemi H, Nedjat S, Shahnazi A, Fotouhi A. Persian version of the 25-item national eye institute visual functioning questionnaire (NEI-VFQ 39): A validation study. Iran J Ophthalmol. 2011; 23(3):5-14. [Link]
- de Boer MR, Moll AC, de Vet HC, Terwee CB, Völker-Dieben HJ, van Rens GH. Psychometric properties of vision‐related quality of life questionnaires: A systematic review. Ophthalmic Physiol Opt. 2004; 24(4):257-73. [DOI:10.1111/j.1475-1313.2004.00187.x] [PMID]
- Elliott DB, Pesudovs K, Mallinson T. Vision-related quality of life. Optom Vis Sci. 2007; 84(8):656-8. [DOI:10.1097/OPX.0b013e31814db01e] [PMID]
- Lamoureux EL, Pesudovs K, Pallant JF, Rees G, Hassell JB, Caudle LE, et al. An evaluation of the 10-item vision core measure 1 (VCM1) scale (the core module of the vision-related quality of life scale) using Rasch analysis. Ophthalmic Epidemiol. 2008; 15(4):224-33. [DOI:10.1080/09286580802256559] [PMID]
- Tadic V, Cooper A, Cumberland P, Lewando-Hundt G, Rahi JS, Vision-related Quality of Life Group. Development of the functional vision questionnaire for children and young people with visual impairment The FVQ_CYP. Ophthalmology. 2013; 120(12):2725-32. [DOI:10.1016/j.ophtha.2013.07.055] [PMID]
- McGuinness MB, Finger RP, Wu Z, Luu CD, Chen FK, Arnold JJ, et al. Properties of the impact of vision impairment and night vision questionnaires among people with intermediate age-related macular degeneration. Transl Vis Sci Technol. 2019; 8(5):3. [DOI:10.1167/tvst.8.5.3] [PMID] [PMCID]
- Jeter PE, Rozanski C, Massof R, Adeyemo O, Dagnelie G, Group PS. Development of the ultra-low vision visual functioning questionnaire (ULV-VFQ). Transl Vis Sci Technol. 2017; 6(3):11. [DOI:10.1167/tvst.6.3.11] [PMID] [PMCID]
- Li X, Chen J, Xu G, Zhong Y, Jang L, Lin L, et al. Development of an elderly low vision quality of life questionnaire for less-developed areas of China. Qual Life Res. 2015; 24(10):2403-13. [DOI:10.1007/s11136-015-0970-2] [PMID]
- Haymes SA, Johnston AW, Heyes AD. Preliminary investigation of the responsiveness of the Melbourne low vision ADL index to low-vision rehabilitation. Optom Vis Sci. 2001; 78(6):373-80. [DOI:10.1097/00006324-200106000-00008] [PMID]
- Haymes SA, Johnston AW, Heyes AD. A weighted version of the Melbourne low-vision ADL index: A measure of disability impact. Optom Vis Sci. 2001; 78(8):565-79. [DOI:10.1097/00006324-200108000-00008] [PMID]
- Pesudovs K, Burr JM, Harley C, Elliott DB. The development, assessment, and selection of questionnaires. Optom Vis Sci. 2007; 84(8):663-74. [DOI:10.1097/OPX.0b013e318141fe75] [PMID]
- Massof RW, Rubin GS. Visual function assessment questionnaires. Surv Ophthalmol. 2001; 45(6):531-48. [DOI:10.1016/S0039-6257(01)00194-1] [PMID]
- Wolffsohn J, Cochrane A, Watt N. Implementation methods for vision related quality of life questionnaires. Br J Ophthalmol. 2000; 84(9):1035-40. [DOI:10.1136/bjo.84.9.1035] [PMID] [PMCID]
- Bokhary KA, Suttle C, Alotaibi AG, Stapleton F, Boon MY. Development and validation of the 21‐item children’s vision for living scale (CVLS) by Rasch analysis. Clin Exp Optom. 2013; 96(6):566-76. [DOI:10.1111/cxo.12055] [PMID]
- Wong MHY, Fenwick E, Aw AT, Lamoureux EL, Seah LL. Development and validation of the Singapore thyroid eye disease quality of life questionnaire. Transl Vis Sci Technol. 2018; 7(5):14. [DOI:10.1167/tvst.7.5.14] [PMID] [PMCID]
- Stelmack JA, Szlyk JP, Stelmack TR, Demers-Turco P, Williams RT, Massof RW. Psychometric properties of the veterans affairs low-vision visual functioning questionnaire. Invest Ophthalmol Vis Sci. 2004; 45(11):3919-28. [DOI:10.1167/iovs.04-0208] [PMID]
- Peters D, Heijl A, Brenner L, Bengtsson B. Visual impairment and vision‐related quality of life in the early manifest glaucoma trial after 20 years of follow‐up. Acta Ophthalmol. 2015; 93(8):745-52. [DOI:10.1111/aos.12839] [PMID] [PMCID]
- Owsley C, McG/win G, Sloane ME, Stalvey BT, Wells J. Timed instrumental activities of daily living tasks: Relationship to visual function in older adults. Optom Vis Sci. 2001; 78(5):350-9. [DOI:10.1097/00006324-200105000-00019] [PMID]
- Finger RP, McSweeney SC, Deverell L, O’Hare F, Bentley SA, Luu CD, et al. Developing an instrumental activities of daily living tool as part of the low vision assessment of daily activities protocol. Invest Ophthalmol Vis Sci. 2014; 55(12):8458-66. [DOI:10.1167/iovs.14-14732] [PMID]
- du Toit R, Palagyi A, Ramke J, Brian G, Lamoureux EL. Development and validation of a vision-specific quality-of-life questionnaire for Timor-Leste. IInvest Ophthalmol Vis Sci. 2008; 49(10):4284-9. [DOI:10.1167/iovs.08-1893] [PMID]
- Gupta S, Viswanath K, Thulasiraj R, Murthy G, Lamping D, Smith S, et al. The development of the Indian vision function questionnaire: Field testing and psychometric evaluation. Br J Ophthalmol. 2005; 89(5):621-7. [DOI:10.1136/bjo.2004.050732] [PMID] [PMCID]
- Marmamula S, Mitchell W, Zebardast N, Locascio J, Barrenkala NR, Kumbham TR, et al. Impact of vision loss on visual function among elderly residents in the home for the aged in India: The Hyderabad ocular morbidity in elderly study. Transl Vis Sci Technol. 2020; 9(13):11. [DOI:10.1167/tvst.9.13.11] [PMID] [PMCID]
- Asgari S, Nedjat S, Hashemi H, Shahnazi A, Fotouhi A. [Quality of life in the group of patients with chronic eye disease (Persian)]. Iran J Epidemiol. 2012; 7(4):43-8. [Link]
- Haymes SA, Johnston AW, Heyes AD. The development of the Melbourne low-vision ADL index: A measure of vision disability. Invest Ophthalmol Vis Sci. 2001; 42(6):1215-25. [PMID]
- World Health Organization (WHO). Programme on mental health division of mental health and prevention of substance abuse. Geneva: World Health Organization; 1997. [Link]
- Wolffsohn JS, Cochrane AL. Design of the low vision quality-of-life questionnaire (LVQOL) and measuring the outcome of low-vision rehabilitation. Am J Ophthalmol. 2000; 130(6):793-802. [DOI:10.1016/S0002-9394(00)00610-3]
- Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD, et al. Development of the 25-list-item national eye institute visual function questionnaire. Arch Ophthalmol. 2001; 119(7):1050-8. [DOI:10.1001/archopht.119.7.1050] [PMID]
- Weih LM, Hassell JB, Keeffe J. Assessment of the impact of vision impairment. Invest Ophthalmol Vis Sci. 2002; 43(4):927-35. [PMID]
- Lamoureux EL, Pallant JF, Pesudovs K, Hassell JB, Keeffe JE. The impact of vision impairment questionnaire: An evaluation of its measurement properties using Rasch analysis. Invest Ophthalmol Vis Sci. 2006; 47(11):4732-41. [DOI:10.1167/iovs.06-0220] [PMID]
- Finger RP, Tellis B, Crewe J, Keeffe JE, Ayton LN, Guymer RH. Developing the impact of vision impairment-very low vision (IVI-VLV) questionnaire as part of the LoVADA protocol. Invest Ophthalmol Vis Sci. 2014; 55(10):6150-8. [DOI:10.1167/iovs.14-14731] [PMID]
- Ayre C, Scally AJ. Critical values for Lawshe’s content validity ratio: Revisiting the original methods of calculation. Meas Eval Couns Dev. 2014; 47(1):79-86. [DOI:10.1177/0748175613513808]
- Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health. 2007; 30(4):459-67. [DOI:10.1002/nur.20199] [PMID]
- Riazi A, Riazi F, Yoosfi R, Bahmeei F. Outdoor difficulties experienced by a group of visually impaired Iranian people. J Curr Ophthalmol. 2016; 28(2):85-90. [DOI:10.1016/j.joco.2016.04.002] [PMID] [PMCID]
Type of Study: Research |
Subject:
Optometry
Received: 2022/07/21 | Accepted: 2022/11/1 | Published: 2022/02/3
Received: 2022/07/21 | Accepted: 2022/11/1 | Published: 2022/02/3