Volume 5, Issue 1 (Continuously Updated 2022)
Func Disabil J 2022, 5(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mohan M, Deb R. Barriers and Facilitators of Community Integration of People With Spinal Cord Injuries Living in Low and Middle-Income Countries: A Systematic Review. Func Disabil J 2022; 5 (1) : 50
URL: http://fdj.iums.ac.ir/article-1-179-en.html
URL: http://fdj.iums.ac.ir/article-1-179-en.html
1- Department of Anthropology, Amity University, Noida, India. , meenakshim89@gmail.com
2- Department of Anthropology, Amity University, Noida, India.
2- Department of Anthropology, Amity University, Noida, India.
Keywords: Spinal cord injury, Low- and middle-income countries, Challenges, Quality of life, Health related issues, Resilience
Full-Text [PDF 1365 kb]
(1399 Downloads)
| Abstract (HTML) (2605 Views)
Full-Text: (1163 Views)
1. Introduction
Spinal Cord Injury (SCI) is an irreversible and potentially life-threatening health condition [1]. It has significant consequences at individual and social levels. The incidence of SCI was higher in low- and middle-income countries (8.72 per 100000 persons) compared with high-income countries (13.69 per 100000 persons). Road traffic accidents, followed by falls, were the most common mechanism of SCI worldwide [2]. SCI not only causes severe disability but also affects body organs resulting in various secondary complications, such as urinary tract infection, severe constipation, breathing difficulty, pressure sores, etc. These secondary complications are the major reasons for the high mortality rate [3, 4, 5]. The two most common clinical manifestations of spinal cord injury are paraplegia and quadriplegia [6]. SCI significantly impacts a person’s Quality of Life (QoL) which expresses physical, psychological, and social participation and functioning. In addition, work, leisure, and daily activities are adversely affected.
Despite the best efforts of medical treatment, SCI patients encounter various physical and mental challenges when they return home. In recent years, the healthcare model has shifted more towards patient-centered care [7]. This care helps improve the quality of life of people with such disabilities through a bio-psychosocial approach. Healthcare professionals aim to maximize functional independence, prevent secondary problems, improve physical functioning, and encourage community reintegration [8]. Even after discharge from the rehabilitation centers, SCI individuals face difficulty participating in the community due to accessibility, affordability, and acceptability issues. This study focuses on determining the issues influencing SCI patients’ engagement in community activities. These issues can be categorized as barriers or facilitators of community participation of people with SCI.
2. Materials and Methods
A systematic literature search was done in Scopus, PsycINFO, and PubMed databases for the relevant studies published from 2010 to 2020. This systematic review is based on PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The protocol was registered in the PROSPERO database (CRD42020206998). Figure 1 displays the consort flow diagram for the reviewed studies. The included articles were those published in the last 10 years (March 2010 to March 2020) conducting on SCI individuals diagnosed with a traumatic or non-traumatic injury, aged above 18 years, living in the community, and discharged from the hospital.
Other than original research, review articles should report the data for SCI from the Low- and middle-income countries (LMICs) [9] and be published in English. Furthermore, these studies aimed to assess the outcome of community reintegration in terms of community access, involvement, independence, and quality of life. Most of the criteria analyzed or measured in the studies were connected to work or employment, sports involvement, anxiety, stress, stigma, and accessibility. Articles were excluded if they did not assess the barriers or facilitators of SCI persons in the community and were not written in English.
Search strategy
The study aims to address the factors which affect the community integration of the SCI individuals in LMIC. The full search and article screening was performed independently by two authors (MM & RD) and compared for consensus.
A PRISMA guideline was followed in four phases: identification, screening, eligibility, and inclusion. Scopus, PsycINFO, and PubMed databases were used for the primary search of studies with the keywords of “spinal cord injury”, “tetraplegia”, “paraplegia”, and “challenges”. These keywords were cross-linked with “community reintegration”, “community participation”, “community access”, “psychological”, “social”, “cultural”, and “culture”. The keywords have been selected by identifying synonyms used by respective databases and Cochrane Library MeSH (Medical Subject Headings) terms contained in the title, abstract and subject descriptors. Boolean operators “AND” and “OR” were used in the literature search. An expanded search was conducted by reviewing citations and references from articles retrieved in the initial search. Duplicate citations were identified and removed through Salesforce Einstein analytics software or MS Excel, and the included abstracts were screened. Finally, the authors reviewed the full text of the articles for eligibility.
Quality assessment
In the present review, the difference in the philosophical origins and methodological approaches of qualitative and quantitative study designs required a specific tool for each type of approach. There is no single validated checklist for all types of qualitative studies [10], so the critical appraisal skills programme (CASP, 2018) 10-step assessment tool was selected. This tool has been previously well-evaluated [11, 12] and is relatively easy to use. The quality assessment for quantitative studies (effective public health practice project [EPHPP] -Thomas Tool, 2010) was used to guide the assessment of quantitative study quality. This tool is recommended for its versatility in application, and its content and construct validity has already been established [10].
Data abstraction
The studies were grouped, described, and evaluated according to their methodological similarities. The qualitative and quantitative studies’ findings were dovetailed to enable interpretation of the findings into a coherent summary of the current evidence on the topic. It included SCI individual characteristics (sample size, age, gender, and injury details), authors details, study design, population, and outcomes of interest. Data were extracted from the studies focusing on the community integration, quality of life, work or employment, financial hardships, stigma, accessibility, optimism, and participation in leisure activities. The data were presented as the scale’s group mean, Standard Deviation (SD), and categories [13].
Data synthesis
Of the 26 studies eligible for review, six had qualitative designs (Arya et al., 2016; Akter et al., 2019; Dorjbal et al., 2020; Irshad et al., 2012; Øderud et al., 2014; Moshi et al., 2020) and 20 had quantitative designs (Ganesh et al., 2015; Busthomy Rofi’IAYA et al., 2019; Gautam et al., 2019; Bhattarai et al., 2020; Bhattarai et al., 2018; Bhattarai et al., 2017; Hossain et al., 2019; Kader et al., 2017; Adhikari et al., 2020; Darain et al., 2017; Scovil et al., 2012; Sekaran et al., 2010; Xue et al., 2016; Selvaraj et al., 2010; Kumar et al., 2016; Kalyani et al., 2014; Moshi H et al., 2020; Hossain et al., 2015; Atobatele et al., 2018; Gupta et al., 2011). The publication year ranged from 2010 to 2020. There were six articles from Nepal, five from India, four from Bangladesh, three from Sri Lanka, two from Pakistan, two from Tanzania, one from Nigeria, one from Indonesia, one from Zimbabwe, and one from Mongolia.
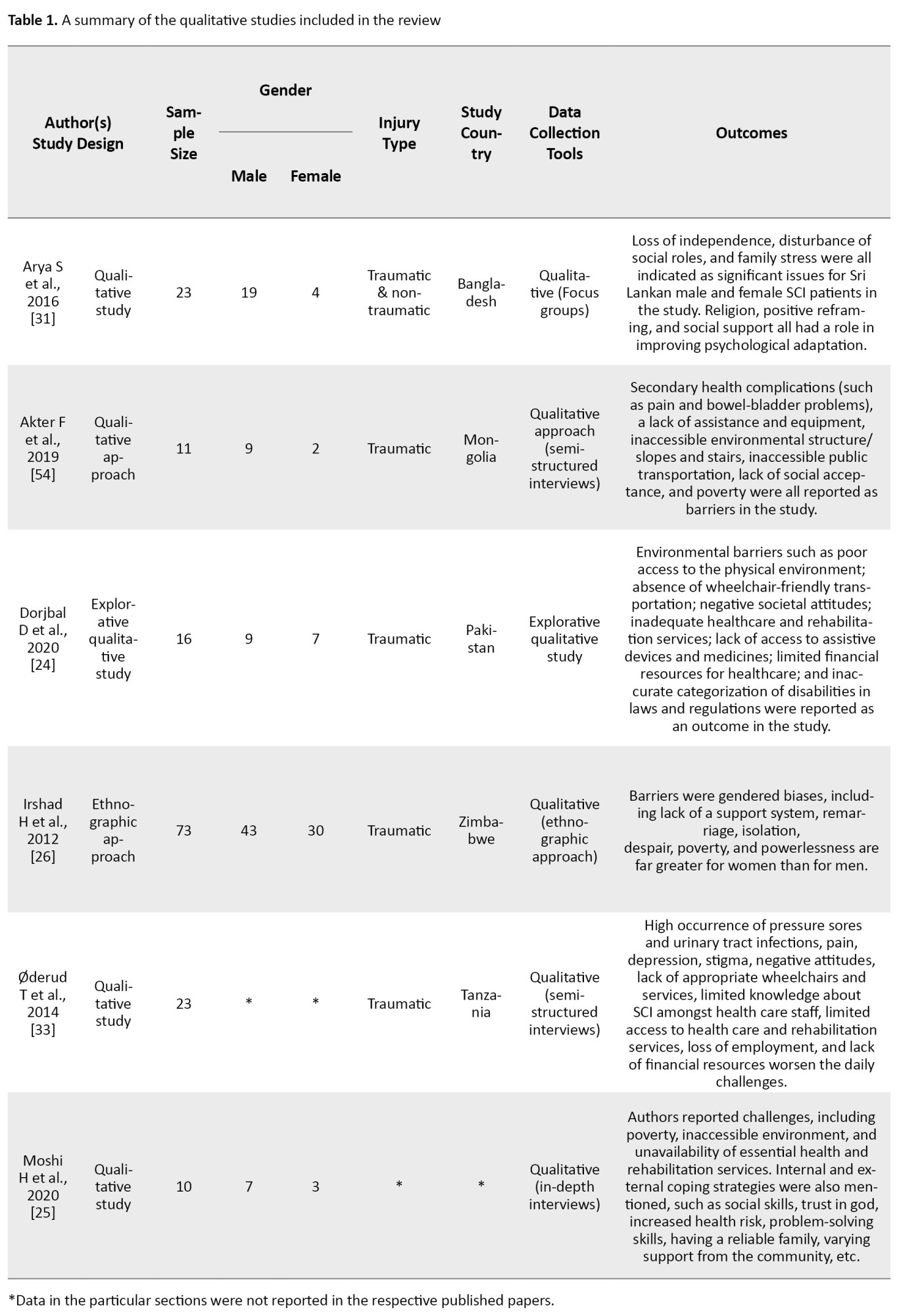
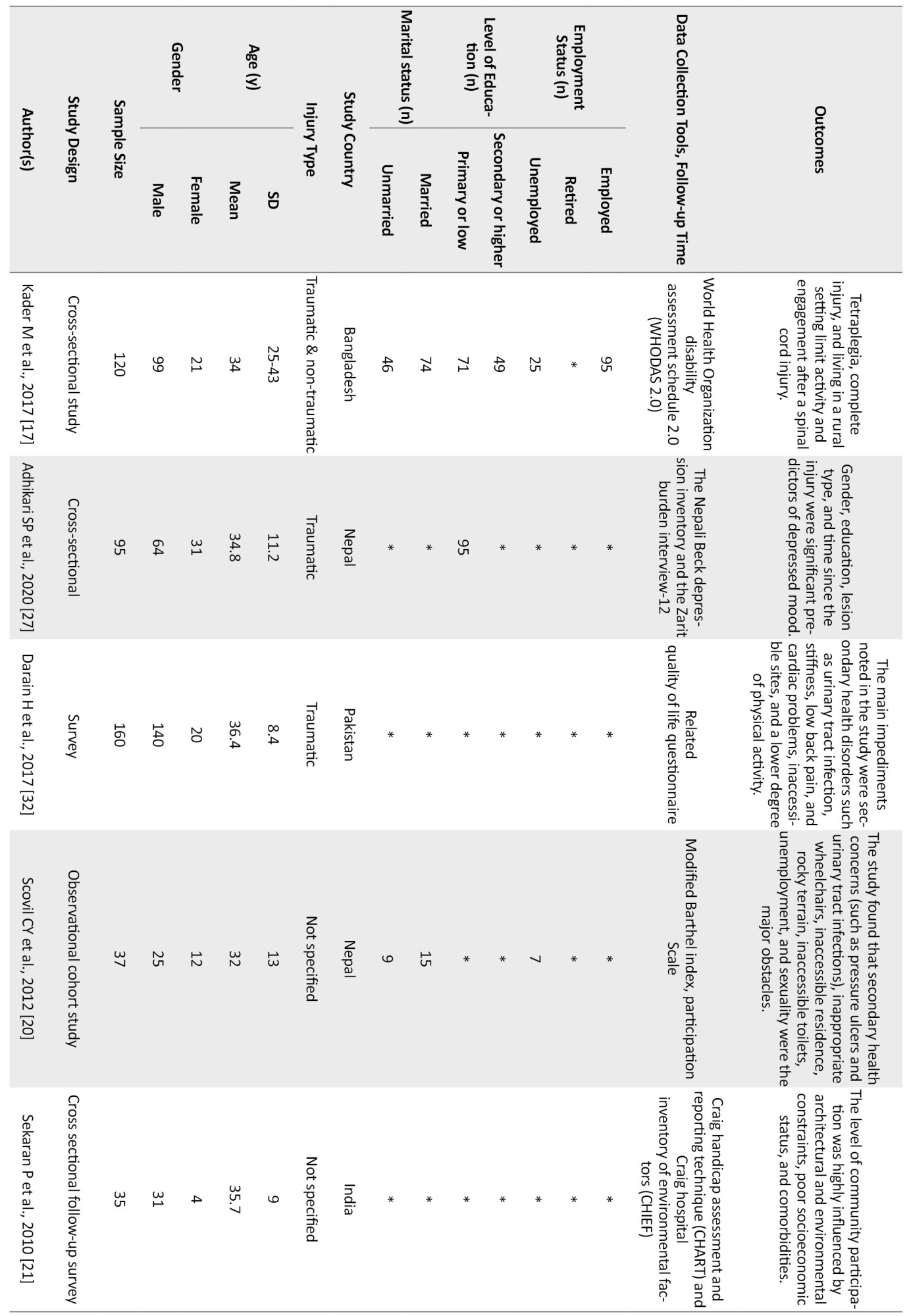
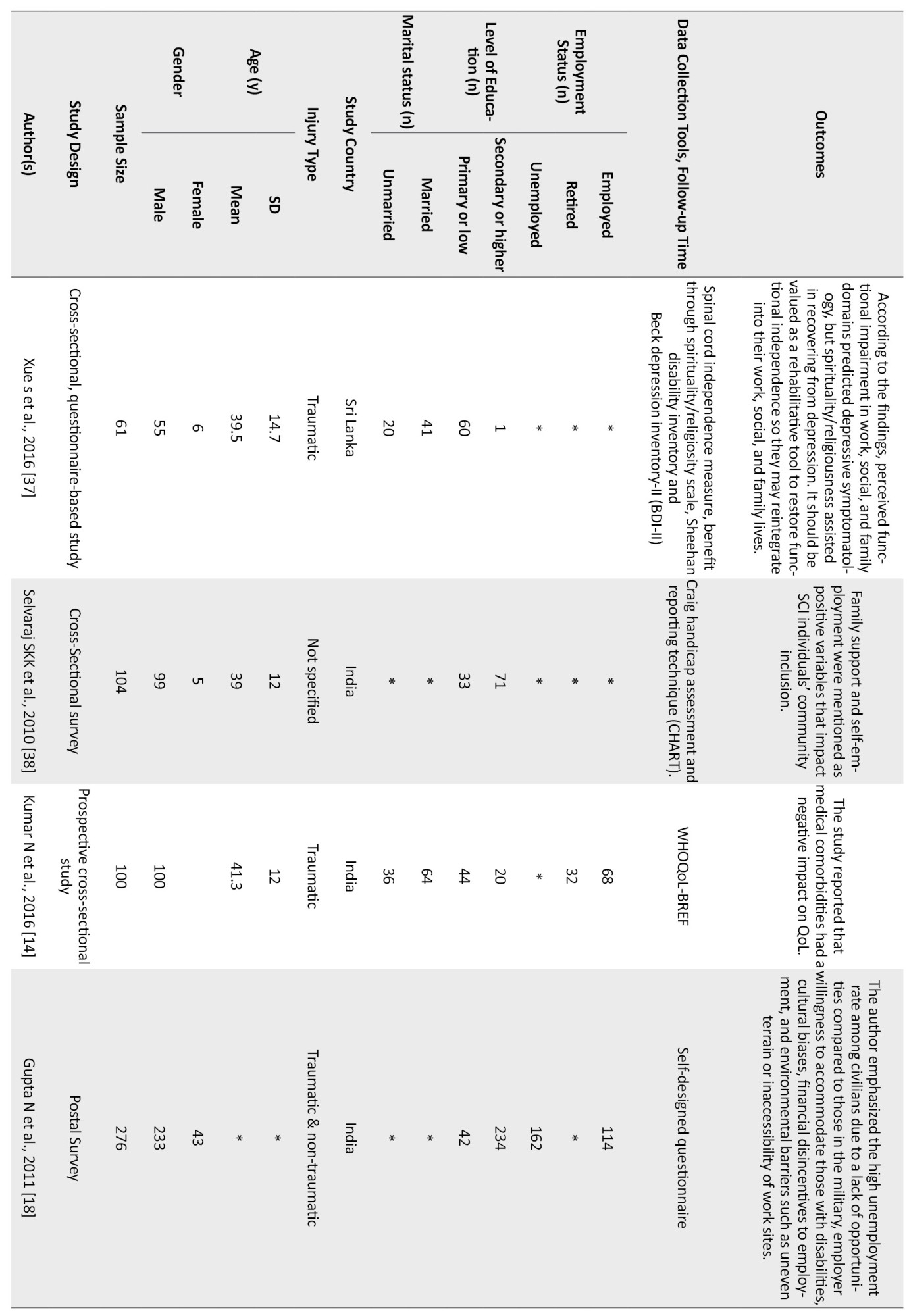
The qualitative studies were all community reintegration focused, involving specific barriers/challenges while participating in the community after SCI (Akter et al. 2019; Dorjbal et al. 2020), and factors that negatively affect the participation like gendered biases that was mentioned in Irshad et al. (2012) study. Similarly, Arya et al. (2016) and Moshi et al. (2020) mentioned the factors or coping strategies which positively affect the community participation of SCI individuals. A summary of the selected studies is presented in Table 1.
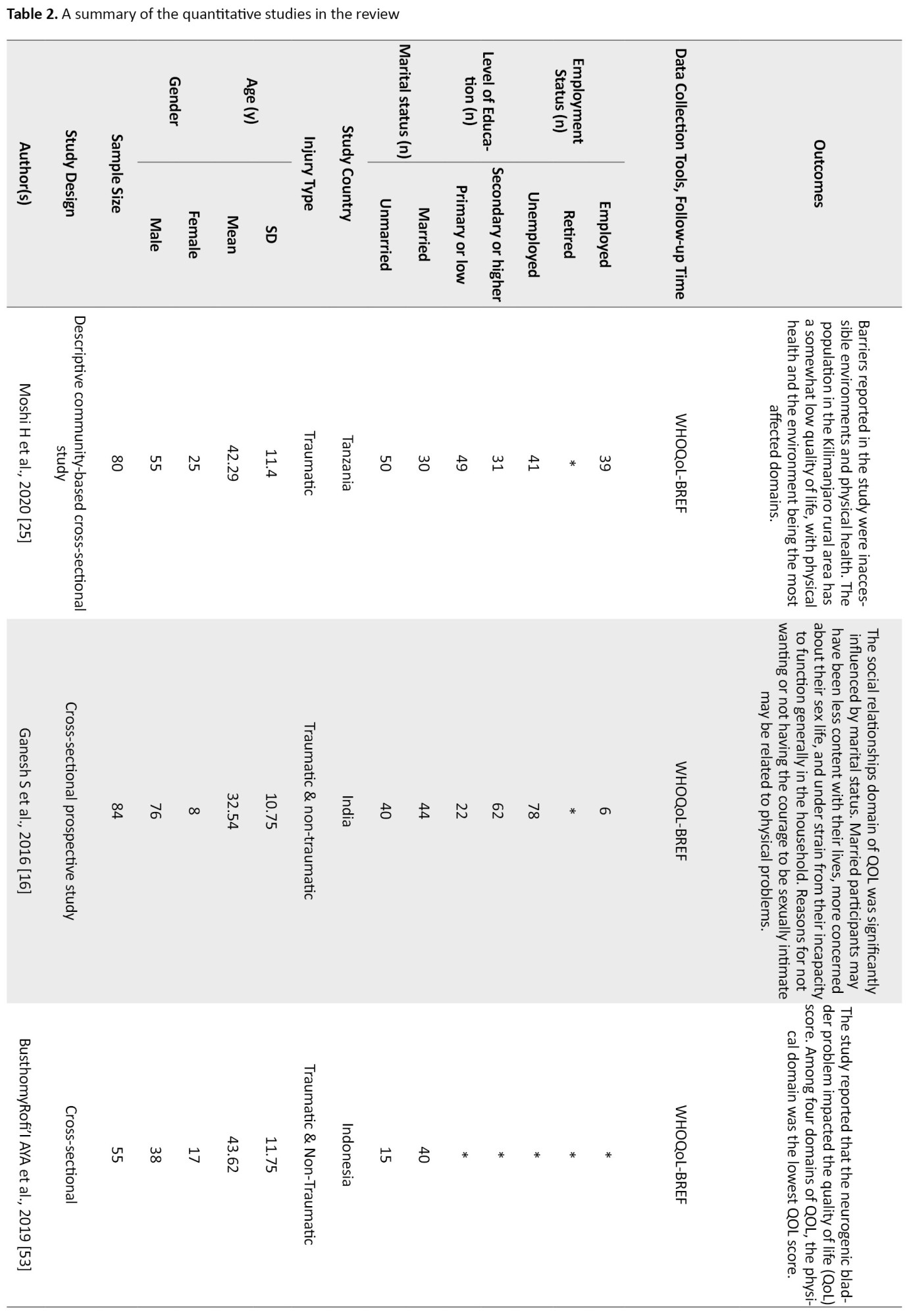
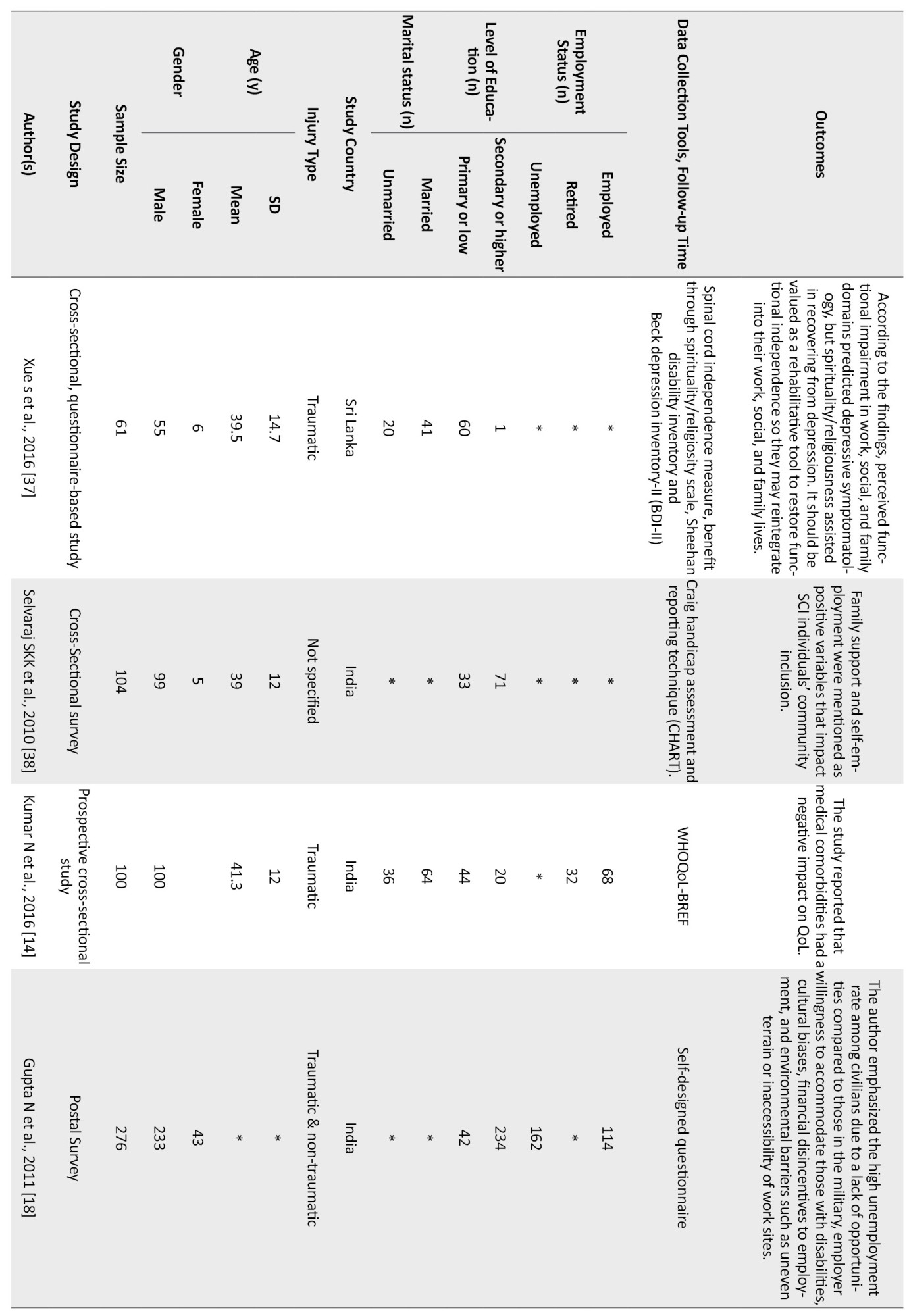
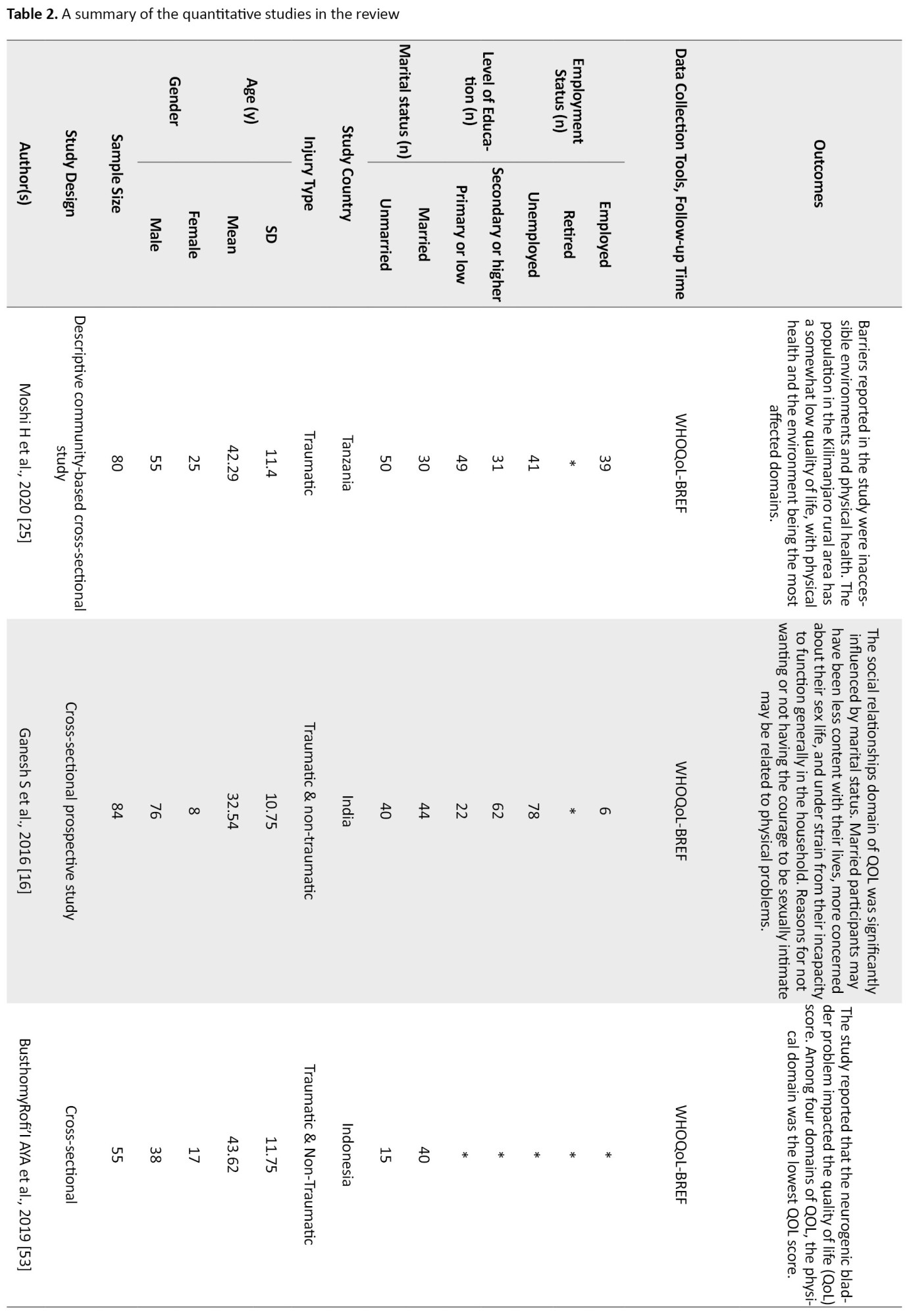
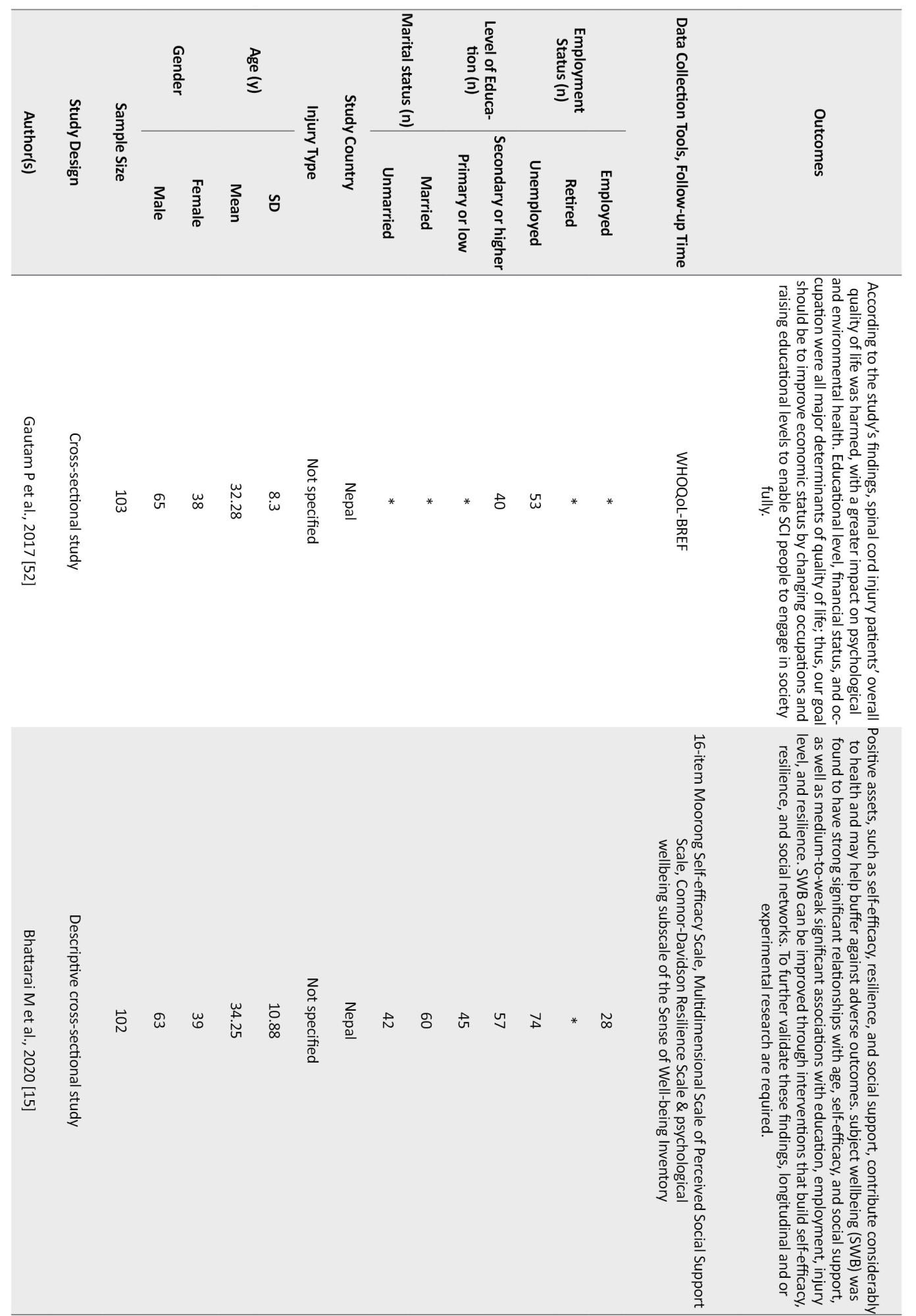
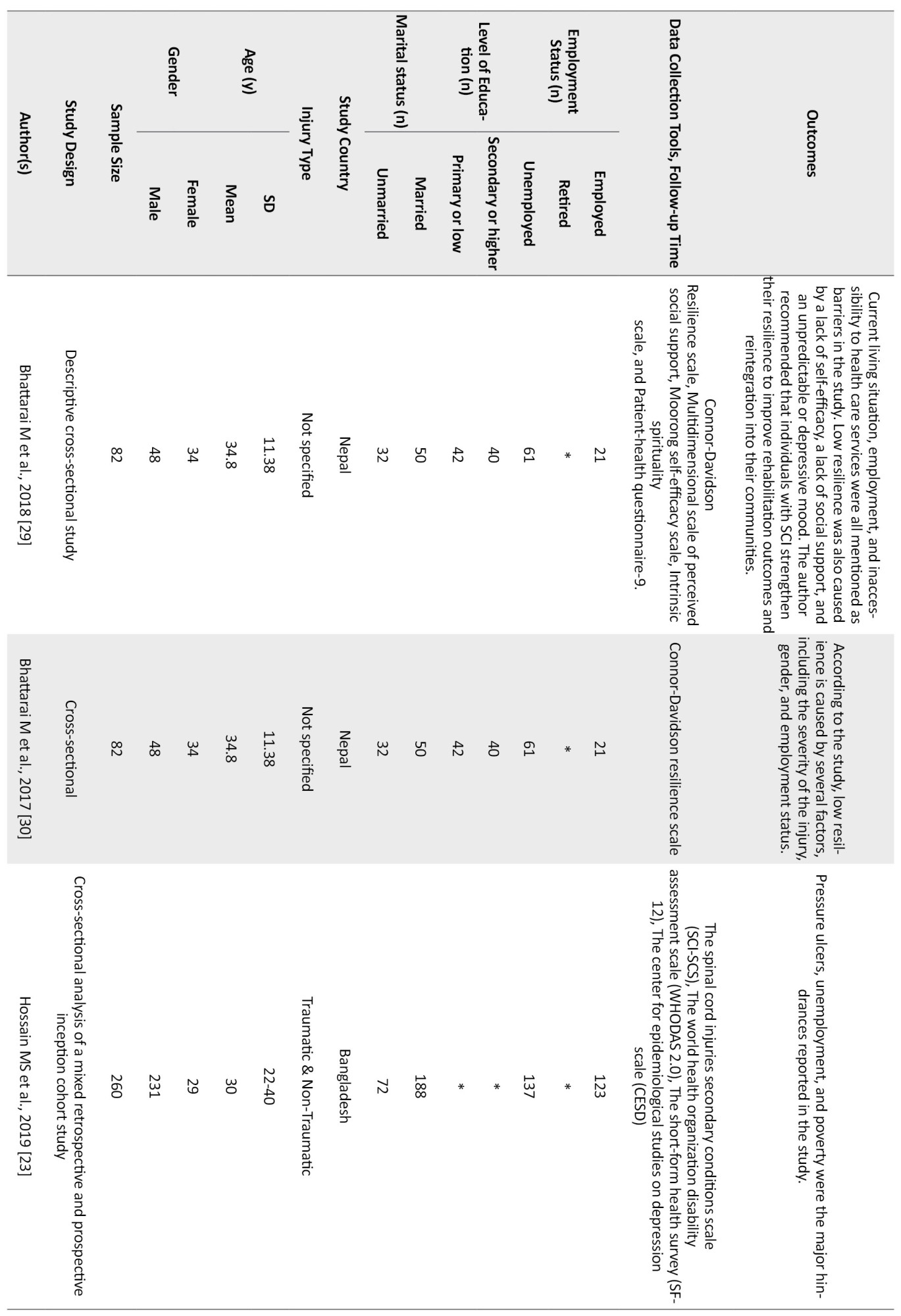
Of the quantitative studies, six had only focused on the factors which affect the community integration of SCI people (Adhikari et al., 2020; Darain et al., 2017; Kader et al., 2017; Selvaraj et al., 2010; Sekaran et al., 2010; Scovil et al., 2012). In contrast, the others discussed SCI people’s Quality of Life (QoL) and their resilience status. Two studies (Xue et al., 2016; Bhattarai et al., 2020; Selvaraj et al., 2010) focused on the facilitators which helped the SCI individuals cope with the challenges of participating in the community. A summary of the eligible studies is presented in Table 2.
3. Results
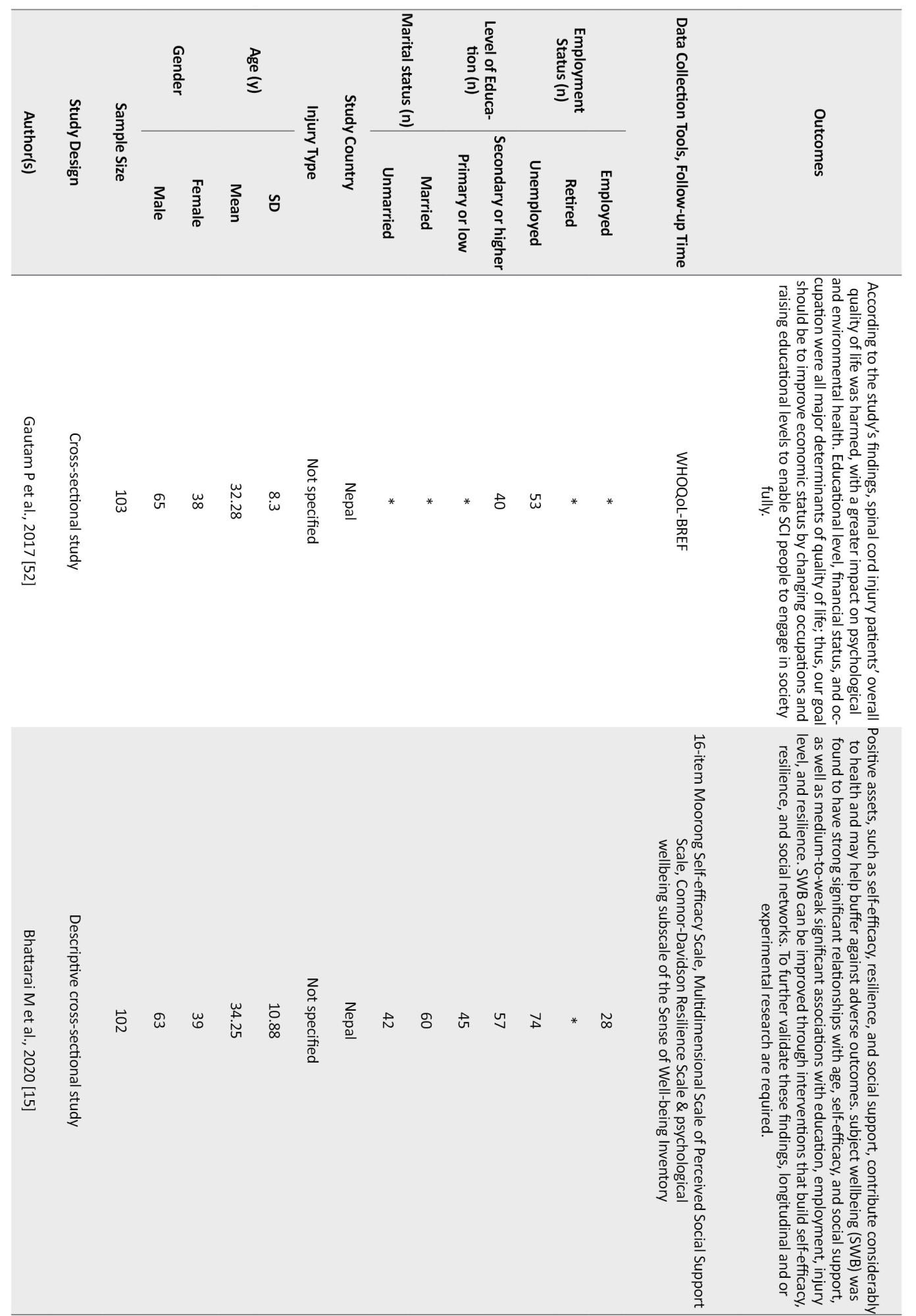
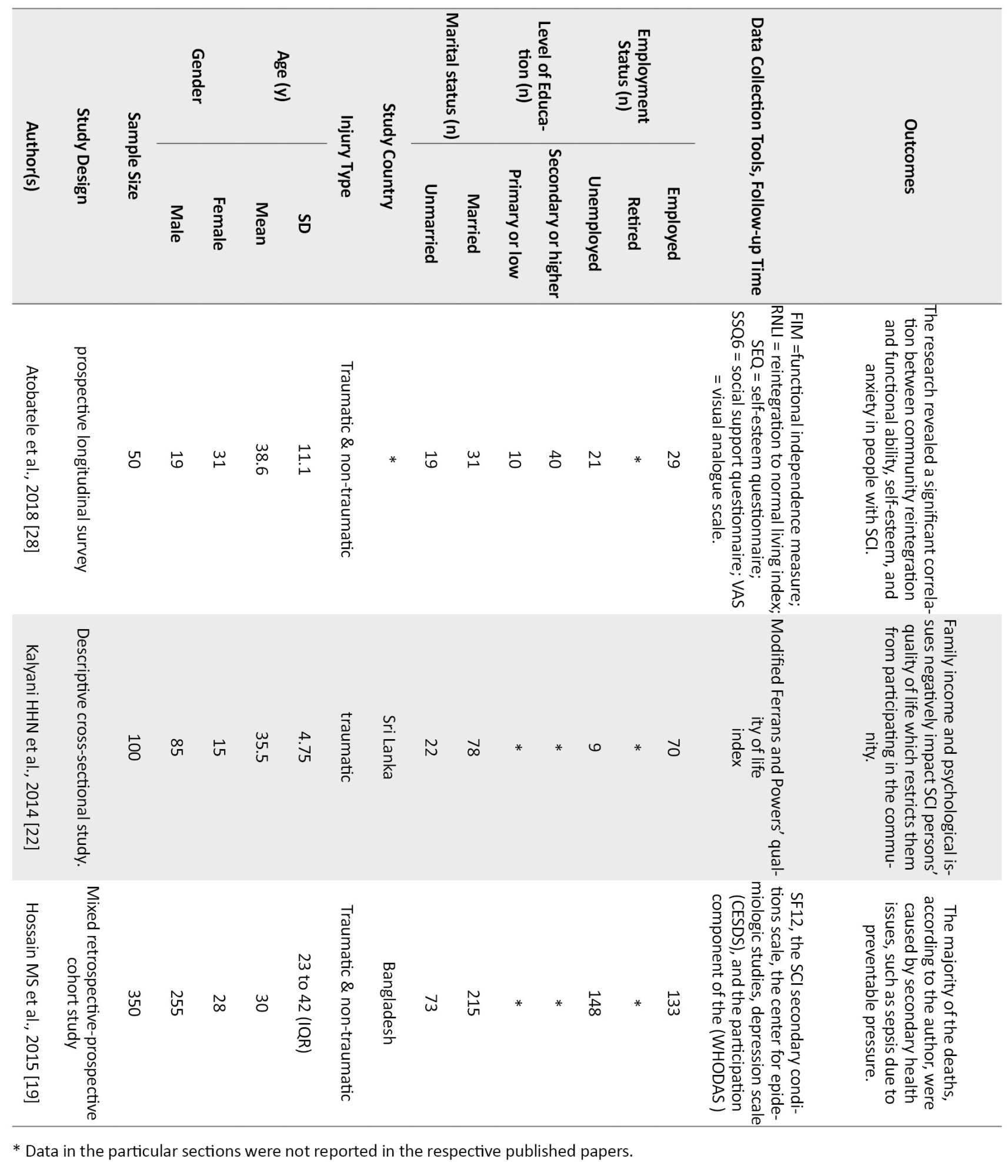
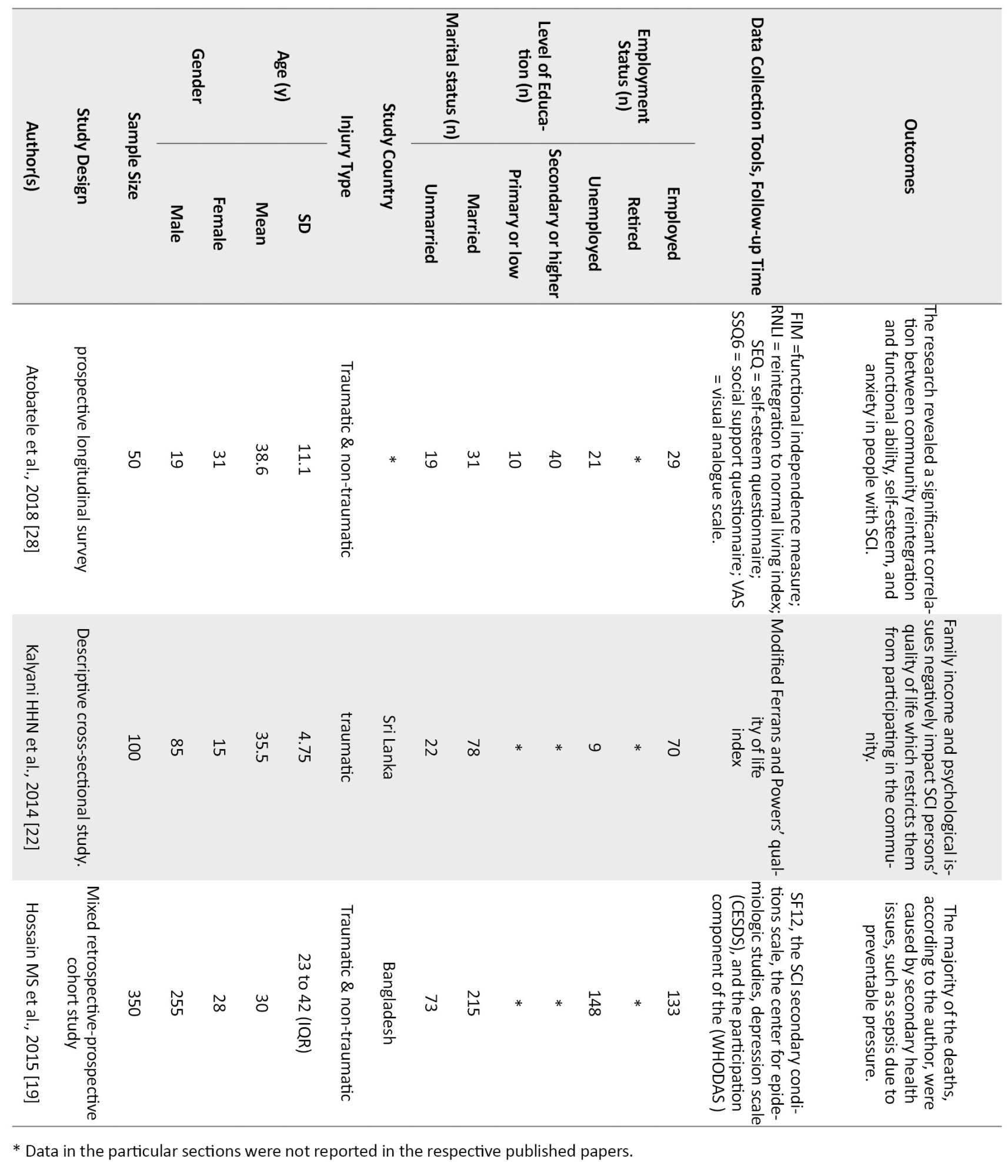
A total of 9020 articles were retrieved from the three different databases. Of those, 3722 duplicate articles were removed, and 5298 articles remained. After screening the titles and abstracts, 5186 articles were excluded, and 112 full-text articles were retrieved. An additional 86 articles were excluded because of having duplicate data; data population were not from LMIC, data included pediatric population, having included comorbidities, i.e., brain injury/dysfunction; no full-text in English; and lacking discussion of the challenges of community integration of SCI persons. In total, 26 articles (Figure 1) were included: 20 quantitative and 6 qualitative studies. A mixed-method study design was used for data synthesis. The data extracted from the studies were classified into six categories: environmental barriers, psychological barriers, cultural barriers, secondary health conditions, spirituality, and support from family or friends. These issues are all associated with the community reintegration of SCI individuals. The aim, method, and research design of all qualitative studies were clear (ranging from moderate to strong). Recruitment strategy, rigorous data analysis, and clear statement of findings were also appropriate (ranging from moderate to strong). Thus, all included studies were rated moderate to strong (Table 3).
.jpg)
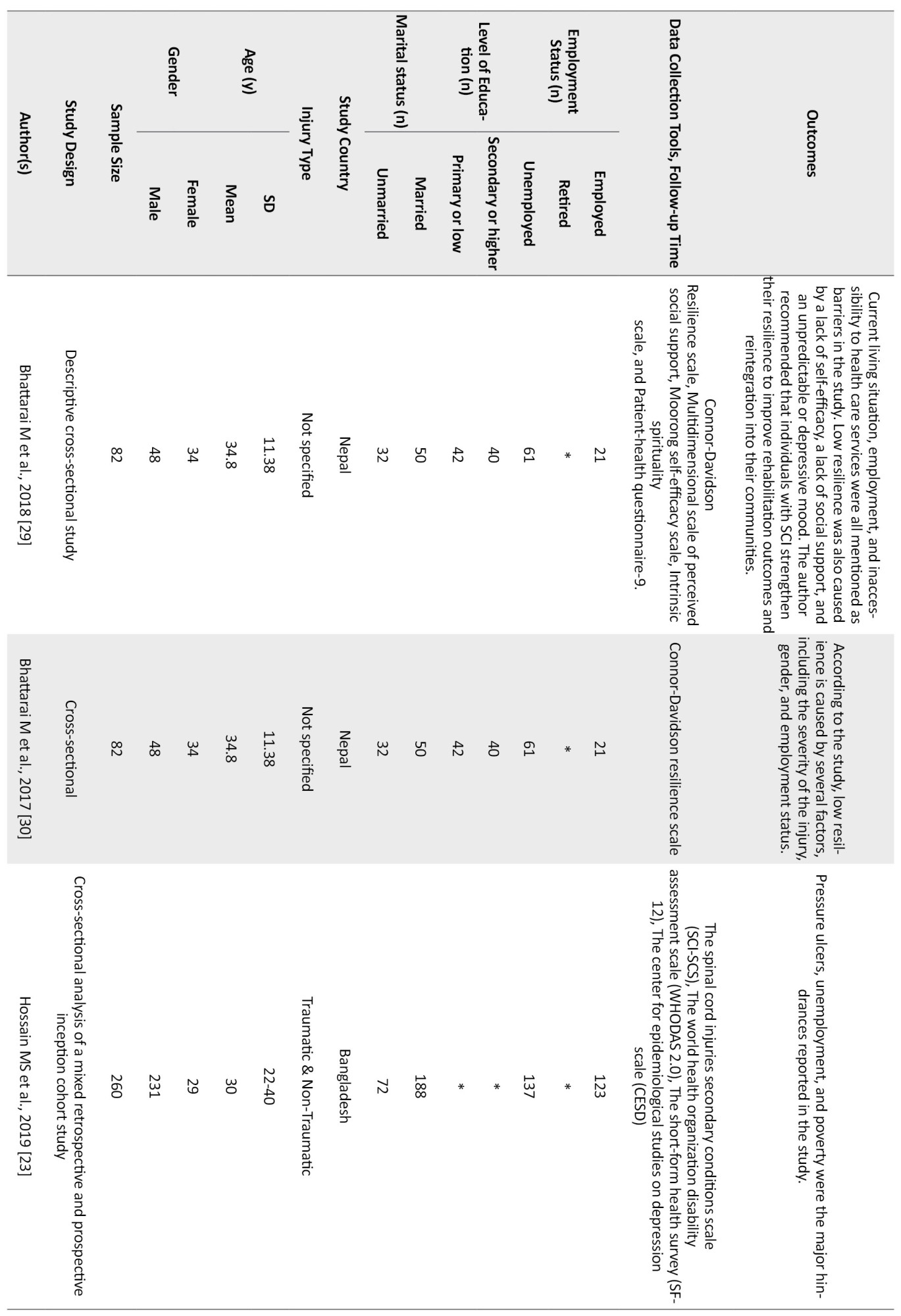
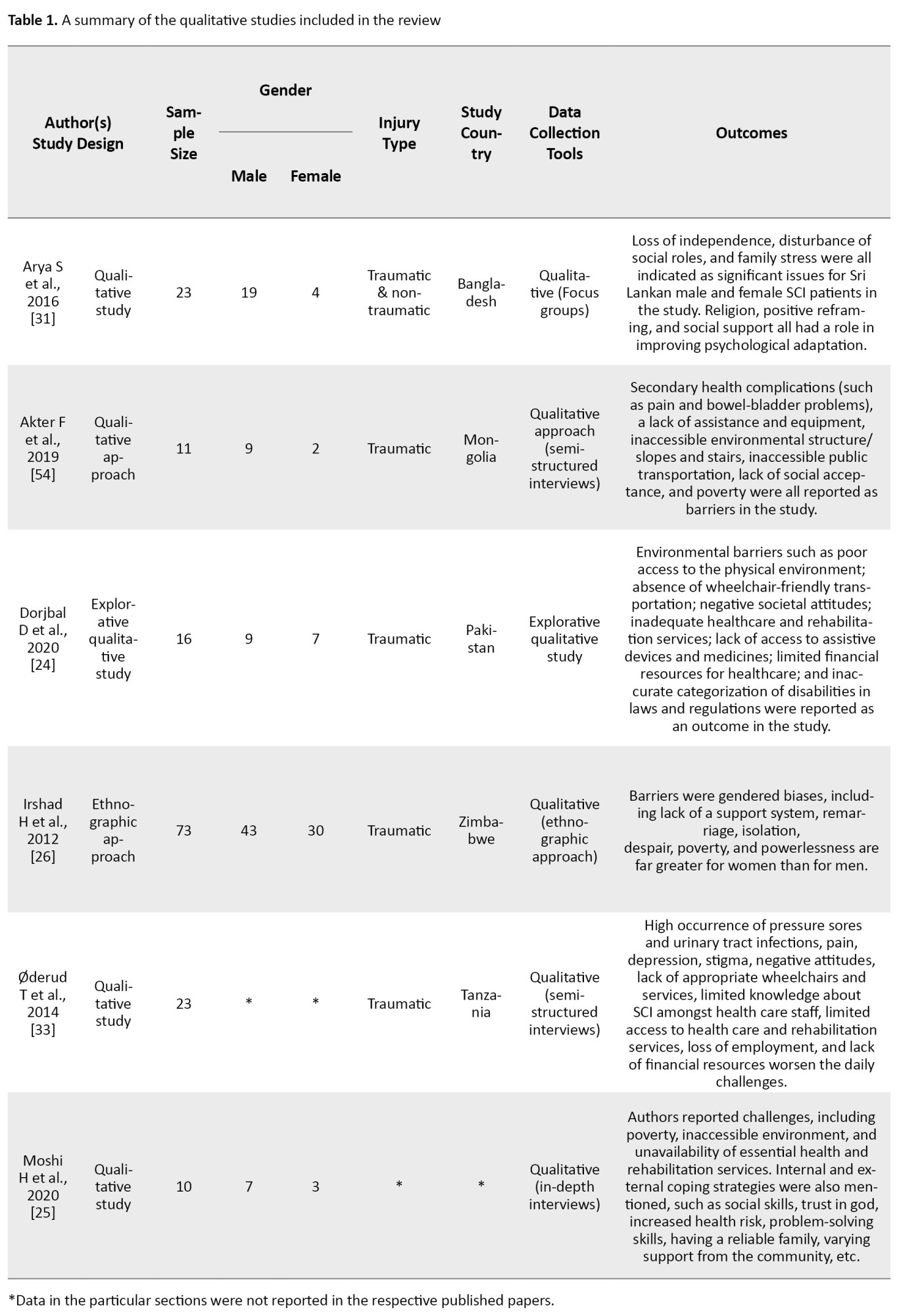
Furthermore, as per the Thomas tool, the global rating of quantitative studies ranged from weak to moderate; 15(75%) quantitative studies were moderate, while 5 (25%) studies were considered weak due to various factors like no declaration of withdrawals, no blinding, or no confounders reported (Table 4).
.jpg)
The rating decreased due to the factors like no clinical trial in the selected 20 studies; most studies were questionnaire-based, without intervention.
The total number of participants in the 26 studies was 2492. The maximum number of participants involved in a study was 350, and the lowest number in a study was 10. Of 2492 SCI participants, 1916 (76.8%) were males, and 486 (19.5%) were females. According to the literature, males were more affected by spinal cord injuries than females due to violence, reckless driving, participation in sports, etc. Epidemiological factors of SCI in India are different from Western countries [14]. The mean age in most of the studies ranges from 30 to 40 years. Most studies have mentioned socio-demographic data, i.e., 980 participants (39.3%) reported being married, 508 (20.3%) were single, and the marital status of 12 (0.48%) was not reported. Also, 555 participants (22.2%) reported primary or low education, whereas 685 (27.4%) fell in the category of secondary or higher education. Similarly, 35.2% of SCI individuals (in the selected studies) were unemployed, and only 29.9% were employed, except for one study [14], where 0.01% of participants were reported as retired or veterans at the time of data collection. Overall, there were only 10 quantitative studies that included all demographic information. The studies were conducted in different LMICs, including Nepal, India, Bangladesh, Sri Lanka, Pakistan, Tanzania, Nigeria, Indonesia, Zimbabwe, and Mongolia.
Categories in the studies reviewed
Environmental barriers
Eleven studies reported several environmental issues, including poor access to the physical environment, inappropriate wheelchairs, inadequate healthcare and rehabilitation services, no access to the medicines and healthcare, limited financial resources, and government policies which are considered challenges for SCI individuals to reintegrate into the community [15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25]. Living in rural areas is one of the significant barriers for people with SCI; the same was reported in a study conducted on 73 SCI participants in the rural areas of Kashmir and Pakistan, where the author addressed the earthquake reconstruction and rehabilitation as an unrealistic and poorly thought-out program. Participants in the study stated that they turned down the idea since it was difficult for them to leave their homes to do any work because there was no road accessible [26]. In addition, the literature supports that the current healthcare system in Mongolia is inadequate for the SCI population due to a lack of knowledge and well-trained rehabilitation experts [24]. Even secondary health issues arose due to a lack of competent and skilled care [24]. In addition, policy barriers, as well as the disability legislation, were reported in two studies [21, 24]. The Craig handicap assessment and reporting technique short form (CHART-SF) was chosen as the assessment tool in a quantitative study. The lowest average score was related to policy barriers because the majority of the participants were unaware of the government’s policies. Although most government programs encourage community reintegration, they have proven to be practically ineffective [21, 24].
Psychological barriers
Five studies [15, 27, 28, 29, 30] reported psychological barriers. The study participants reported their injuries as a life-altering event that brought them depression, anxiety, shock, failure, dependency, and hopelessness. A study on psychosocial factors among the Nepalese SCI population revealed that resilience was linked to demographic parameters such as gender, employment, and living place. As a result, interventions or rehabilitation should be targeted at specific psychosocial and demographic characteristics to increase community involvement among people with SCI [29]. The prevalence of depressed mood among individuals with traumatic SCI and the burden of caregiving among caregivers was high [27].
Another study conducted on Sri Lankan population used descriptive thematic analysis to illuminate psychological barriers. Participants in the study shared their feelings about how SCI has damaged their relationships. They rely entirely on their spouse like a child and cannot spend much time with their family. They were depressed as a result of these circumstances [31]. Female participants frequently mentioned broken family ties, although the nature of these breakups was different. Female participants expressed dissatisfaction with their inability to participate in family activities as they did before. Young adults, on the other hand, felt gloomy because they could not follow their careers as they desired before the injury. All preceding observations can be expressed as feelings of loneliness, hopelessness, and emptiness in the SCI individuals. Participants feel guilty about not being able to help or support their families. These feelings affect their quality of life and become barriers to participation in the community.
Cultural barriers
Two studies discussed the factors which comprise the cultural barriers: negligence, discrimination, stigma, negative attitude from the society and family members, acceptance, and gendered biases [24, 26]. The negative attitude of society and families toward SCI individuals after their injury was reported in a study conducted on the Mongolian population [24]. The findings of the study reported discrimination in the families (e.g., not being accepted by the girlfriend’s family), at work (e.g., not being hired because the recruiter did not feel they were capable of performing the job or being paid less), and in society (e.g., people believe that persons with disabilities are paying for previous bad deeds). In addition, the issue of gender biases was reported in a study conducted in six villages of Bagh District, Kashmir, and Pakistan; the findings revealed that the women were socially, emotionally, and financially isolated. In contrast, men received full social and emotional support from their families and friends. SCI women have a high degree of anxiety, depression, a sense of helplessness, and a cynical view of life due to the gendered biases and the concept of remarriages [26].
Secondary health conditions
Four quantitative [19, 20, 23, 32] and one qualitative [33] studies reported several secondary health complications, including the high occurrence of pressure sores, urinary tract infections, pain, neurogenic bladder, spasticity, contracture, tightness, and sleep problems, which were considered key factors for reducing the mobility and community participation in individuals with SCI. The spinal cord injuries secondary conditions scale (SCI-SCS) is a standardized and validated 16-item questionnaire used in a study to measure secondary complications, such as pressure ulcers, respiratory problems, postural hypotension, spasticity, and pain [19]. According to published studies, pressure ulcers are prevalent in people with SCI who live in LMICs [19, 34, 35]. Pressure ulcers are expected to be preventable with simple, low-cost methods, such as regular position changes and the use of cushions on wheelchairs [36]. These factors suggest that measures to prevent pressure ulcers should be prioritized in LMICs to increase the survival of spinal cord injury individuals after discharge from the hospital.
Facilitators
Five studies [30, 31, 37, 38, 39] revealed the characteristics that help people favorably manage SCI. Religious practice was the most common method for dealing with chronic problems. Generally, SCI participants relied on spiritual practices for comfort, consolation, and inner calm, especially during tough times. Some believed that religious figures were also responsible for or assisted in improving their physical conditions. SCI prompted not only religious yearning but also religious intensification in study participants. Karma also strongly impacted individuals’ attitudes and psychological health [31]. A study in Nepal reported that positive assets, such as self-efficacy, resilience, and social support, contribute considerably to health and buffer against adverse outcomes [15]. Subject wellbeing was found to have significant solid relationships with age, self-efficacy, and social support. For further validation of these findings, longitudinal and or experimental research is obligatory [15]. Moreover, a greater emphasis should be put on family involvement in SCI rehabilitation for social integration [38]. This issue had been proven statistically in a study where the Craig Handicap Assessment and Reporting Technique (CHART) scale was used to measure social integration after SCI [38].
4. Discussion
Overall findings of the review showed the diverse experience of 2692 SCI participants in 26 studies (qualitative and quantitative) that elucidate the barriers and facilitators of the SCI people’s reintegration into the community in low- and middle-income countries. This systematic review yielded enormous evidence reporting that physical environmental factors (such as access to public places, public transport, financial constraints, and unemployment) are the major hindrances for the SCI people to reintegrate into the community. Dorjbal et al. used an explorative qualitative study design with semi-structured interviews to study the lived experience of individuals with SCI in Mongolia. The study’s findings helped describe environmental barriers that impacted the development of secondary health conditions, limited activities, and participation in almost all areas of life. It has been seen that people with SCI often use healthcare services as compared to people without disabilities due to their secondary complications such as sepsis, pressure ulcers, and urinary tract infection [33, 40], and this condition impacts their quality of life [41, 42]. Hossain et al. (2016) conducted a mixed retrospective-prospective cohort design to determine survival after SCI in LMICs like Bangladesh. Findings of the study supported that cushions on wheelchairs and foam overlays on beds would help prevent the deaths amongst SCI individuals due to sepsis and pressure ulcers [19].
Furthermore, the present study observed the interrelationship between the barriers. If a person gets an appropriate healthcare facility, including appropriate wheelchairs, roads, and transportation for mobility, he or she is unlikely to bother about cultural and psychological issues. Environmental constraints mainly cause discrimination and a lack of confidence in SCI patients, leaving them completely reliant on their caregivers [24, 43]. A cross-sectional study was conducted by Muller et al. (2015). Their conclusion supported that those SCI individuals with better social support took lower scores in depression and higher scores in QoL [44].
Further, the United Nations stressed the significance of accessibility for individuals with physical disabilities to engage in community activities and considered the physical environmental barriers such as homes and public spaces, as well as public transit around the world [45, 46]. Due to limited transportation, mobility, and social impediments in LMICs, reintegration into society is a major challenge for SCI individuals. On the contrary, developed countries have shown a better quality of life than LMICs in terms of medical management, rate of morbidity/mortality, access to the physical environment, proper equipment, and so on [46]. People with SCI face various social hurdles, including low patient and family education, friend and family relationships, financial restrictions, unemployment, and social prejudices. The identified barriers regarding patient and family education during this review were further supported by studies that proved that enough knowledge and training skills were very useful to adjust to SCI [47]. Whereas unemployment and lack of vocational training after SCI are the substantial roadblocks that place a financial burden on the SCI individuals and their families [29, 48].
As per WHO factsheets, the global unemployment rate is more than 60% amongst the SCI population [49]. Published studies indicate that employment rates in low-resource countries range from 7% to 41% [18, 48]. Unemployment and low income may result in financial difficulties, an important factor affecting the QoL of people with SCI [16]. Financial hardships may also be associated with emotional problems. Studies indicate that unemployment rates are 10 times higher among SCI patients compared with the general population [20, 21, 50, 51]. Access to the place of work, employer attitudes, and patients’ beliefs in their abilities may influence the decision to resume employment after SCI. Singh R et al. (2007) found that employment status was associated with a higher QoL among those with SCI living in India [41]. Moreover, government policies, particularly social policies, significantly impact the participation of SCI people with physical disabilities [21, 26]. Social support, education level, financial standing, job security, and involvement in social and recreational activities have all been identified as factors that may affect a person’s ability to adjust to SCI.
The present systematic review also highlighted the facilitators that help SCI individuals overcome the hurdles mentioned above and help them participate in the community. A cross-sectional questionnaire-based study was conducted on the Sri Lankan population by Xue S et al. (2016). The study’s findings emphasized the need for rehabilitative programming to support patients’ spirituality/religiosity activities and mental wellbeing [37]. The most frequent approach for dealing with personal concerns was a religious practice. A similar study based on a focus group research design examined the coping mechanism after SCI. The findings suggested that spiritual practices provided solace, consolation, and inner quiet to participants, especially during difficult times, helping them participate in community activities well [31]. Social support provides a fundamental role in both depression and adjustment of SCI individuals. Persons who enjoy more social support recognize them as the reason behind the improvement in their condition. They are less emotionally distressed and report better life satisfaction and quality of life [38].
5. Conclusion
In conclusion, environmental, psychological, cultural, and health-related issues hamper SCI individuals from participating in the community. The majority of studies highlight specific key difficulties associated with these hurdles, such as acceptability, affordability, and accessibility, which include social/self/family acceptance, financial restrictions, lack of employment, and access to places, toilets, and residences. Furthermore, research has revealed that coping strategies such as spirituality/religiosity and family/friends support are essential for SCI people to reintegrate into the community fully. Individuals with SCI and their families should be an integral part of the rehabilitation team, as this will help them comprehend the effects of the injury and decrease the psychological burden. Healthcare professionals could strengthen the patient-provider interaction by establishing short- and long-term treatment goals such as independence, vocational training, a positive attitude, and counseling-spousal involvement, considering patients’ clinical and demographic variables. Working on the abovementioned issues can help SCI people in low- and middle-income countries become more integrated into their communities.
Ethical Considerations
Compliance with ethical guidelines
There was no use of human volunteers/animals during this research.
Funding
No funding has been availed for this study.
Authors' contributions
The datasets generated and analyzed during the current review study are available from the corresponding author upon reasonable request.
Conflict of interest
We certify that there is no actual or potential conflict of interest concerning this review.
Acknowledgments
References
Spinal Cord Injury (SCI) is an irreversible and potentially life-threatening health condition [1]. It has significant consequences at individual and social levels. The incidence of SCI was higher in low- and middle-income countries (8.72 per 100000 persons) compared with high-income countries (13.69 per 100000 persons). Road traffic accidents, followed by falls, were the most common mechanism of SCI worldwide [2]. SCI not only causes severe disability but also affects body organs resulting in various secondary complications, such as urinary tract infection, severe constipation, breathing difficulty, pressure sores, etc. These secondary complications are the major reasons for the high mortality rate [3, 4, 5]. The two most common clinical manifestations of spinal cord injury are paraplegia and quadriplegia [6]. SCI significantly impacts a person’s Quality of Life (QoL) which expresses physical, psychological, and social participation and functioning. In addition, work, leisure, and daily activities are adversely affected.
Despite the best efforts of medical treatment, SCI patients encounter various physical and mental challenges when they return home. In recent years, the healthcare model has shifted more towards patient-centered care [7]. This care helps improve the quality of life of people with such disabilities through a bio-psychosocial approach. Healthcare professionals aim to maximize functional independence, prevent secondary problems, improve physical functioning, and encourage community reintegration [8]. Even after discharge from the rehabilitation centers, SCI individuals face difficulty participating in the community due to accessibility, affordability, and acceptability issues. This study focuses on determining the issues influencing SCI patients’ engagement in community activities. These issues can be categorized as barriers or facilitators of community participation of people with SCI.
2. Materials and Methods
A systematic literature search was done in Scopus, PsycINFO, and PubMed databases for the relevant studies published from 2010 to 2020. This systematic review is based on PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The protocol was registered in the PROSPERO database (CRD42020206998). Figure 1 displays the consort flow diagram for the reviewed studies. The included articles were those published in the last 10 years (March 2010 to March 2020) conducting on SCI individuals diagnosed with a traumatic or non-traumatic injury, aged above 18 years, living in the community, and discharged from the hospital.
Other than original research, review articles should report the data for SCI from the Low- and middle-income countries (LMICs) [9] and be published in English. Furthermore, these studies aimed to assess the outcome of community reintegration in terms of community access, involvement, independence, and quality of life. Most of the criteria analyzed or measured in the studies were connected to work or employment, sports involvement, anxiety, stress, stigma, and accessibility. Articles were excluded if they did not assess the barriers or facilitators of SCI persons in the community and were not written in English.
Search strategy
The study aims to address the factors which affect the community integration of the SCI individuals in LMIC. The full search and article screening was performed independently by two authors (MM & RD) and compared for consensus.
A PRISMA guideline was followed in four phases: identification, screening, eligibility, and inclusion. Scopus, PsycINFO, and PubMed databases were used for the primary search of studies with the keywords of “spinal cord injury”, “tetraplegia”, “paraplegia”, and “challenges”. These keywords were cross-linked with “community reintegration”, “community participation”, “community access”, “psychological”, “social”, “cultural”, and “culture”. The keywords have been selected by identifying synonyms used by respective databases and Cochrane Library MeSH (Medical Subject Headings) terms contained in the title, abstract and subject descriptors. Boolean operators “AND” and “OR” were used in the literature search. An expanded search was conducted by reviewing citations and references from articles retrieved in the initial search. Duplicate citations were identified and removed through Salesforce Einstein analytics software or MS Excel, and the included abstracts were screened. Finally, the authors reviewed the full text of the articles for eligibility.
Quality assessment
In the present review, the difference in the philosophical origins and methodological approaches of qualitative and quantitative study designs required a specific tool for each type of approach. There is no single validated checklist for all types of qualitative studies [10], so the critical appraisal skills programme (CASP, 2018) 10-step assessment tool was selected. This tool has been previously well-evaluated [11, 12] and is relatively easy to use. The quality assessment for quantitative studies (effective public health practice project [EPHPP] -Thomas Tool, 2010) was used to guide the assessment of quantitative study quality. This tool is recommended for its versatility in application, and its content and construct validity has already been established [10].
Data abstraction
The studies were grouped, described, and evaluated according to their methodological similarities. The qualitative and quantitative studies’ findings were dovetailed to enable interpretation of the findings into a coherent summary of the current evidence on the topic. It included SCI individual characteristics (sample size, age, gender, and injury details), authors details, study design, population, and outcomes of interest. Data were extracted from the studies focusing on the community integration, quality of life, work or employment, financial hardships, stigma, accessibility, optimism, and participation in leisure activities. The data were presented as the scale’s group mean, Standard Deviation (SD), and categories [13].
Data synthesis
Of the 26 studies eligible for review, six had qualitative designs (Arya et al., 2016; Akter et al., 2019; Dorjbal et al., 2020; Irshad et al., 2012; Øderud et al., 2014; Moshi et al., 2020) and 20 had quantitative designs (Ganesh et al., 2015; Busthomy Rofi’IAYA et al., 2019; Gautam et al., 2019; Bhattarai et al., 2020; Bhattarai et al., 2018; Bhattarai et al., 2017; Hossain et al., 2019; Kader et al., 2017; Adhikari et al., 2020; Darain et al., 2017; Scovil et al., 2012; Sekaran et al., 2010; Xue et al., 2016; Selvaraj et al., 2010; Kumar et al., 2016; Kalyani et al., 2014; Moshi H et al., 2020; Hossain et al., 2015; Atobatele et al., 2018; Gupta et al., 2011). The publication year ranged from 2010 to 2020. There were six articles from Nepal, five from India, four from Bangladesh, three from Sri Lanka, two from Pakistan, two from Tanzania, one from Nigeria, one from Indonesia, one from Zimbabwe, and one from Mongolia.
The qualitative studies were all community reintegration focused, involving specific barriers/challenges while participating in the community after SCI (Akter et al. 2019; Dorjbal et al. 2020), and factors that negatively affect the participation like gendered biases that was mentioned in Irshad et al. (2012) study. Similarly, Arya et al. (2016) and Moshi et al. (2020) mentioned the factors or coping strategies which positively affect the community participation of SCI individuals. A summary of the selected studies is presented in Table 1.
Of the quantitative studies, six had only focused on the factors which affect the community integration of SCI people (Adhikari et al., 2020; Darain et al., 2017; Kader et al., 2017; Selvaraj et al., 2010; Sekaran et al., 2010; Scovil et al., 2012). In contrast, the others discussed SCI people’s Quality of Life (QoL) and their resilience status. Two studies (Xue et al., 2016; Bhattarai et al., 2020; Selvaraj et al., 2010) focused on the facilitators which helped the SCI individuals cope with the challenges of participating in the community. A summary of the eligible studies is presented in Table 2.
3. Results
A total of 9020 articles were retrieved from the three different databases. Of those, 3722 duplicate articles were removed, and 5298 articles remained. After screening the titles and abstracts, 5186 articles were excluded, and 112 full-text articles were retrieved. An additional 86 articles were excluded because of having duplicate data; data population were not from LMIC, data included pediatric population, having included comorbidities, i.e., brain injury/dysfunction; no full-text in English; and lacking discussion of the challenges of community integration of SCI persons. In total, 26 articles (Figure 1) were included: 20 quantitative and 6 qualitative studies. A mixed-method study design was used for data synthesis. The data extracted from the studies were classified into six categories: environmental barriers, psychological barriers, cultural barriers, secondary health conditions, spirituality, and support from family or friends. These issues are all associated with the community reintegration of SCI individuals. The aim, method, and research design of all qualitative studies were clear (ranging from moderate to strong). Recruitment strategy, rigorous data analysis, and clear statement of findings were also appropriate (ranging from moderate to strong). Thus, all included studies were rated moderate to strong (Table 3).
.jpg)
Furthermore, as per the Thomas tool, the global rating of quantitative studies ranged from weak to moderate; 15(75%) quantitative studies were moderate, while 5 (25%) studies were considered weak due to various factors like no declaration of withdrawals, no blinding, or no confounders reported (Table 4).
.jpg)
The rating decreased due to the factors like no clinical trial in the selected 20 studies; most studies were questionnaire-based, without intervention.
The total number of participants in the 26 studies was 2492. The maximum number of participants involved in a study was 350, and the lowest number in a study was 10. Of 2492 SCI participants, 1916 (76.8%) were males, and 486 (19.5%) were females. According to the literature, males were more affected by spinal cord injuries than females due to violence, reckless driving, participation in sports, etc. Epidemiological factors of SCI in India are different from Western countries [14]. The mean age in most of the studies ranges from 30 to 40 years. Most studies have mentioned socio-demographic data, i.e., 980 participants (39.3%) reported being married, 508 (20.3%) were single, and the marital status of 12 (0.48%) was not reported. Also, 555 participants (22.2%) reported primary or low education, whereas 685 (27.4%) fell in the category of secondary or higher education. Similarly, 35.2% of SCI individuals (in the selected studies) were unemployed, and only 29.9% were employed, except for one study [14], where 0.01% of participants were reported as retired or veterans at the time of data collection. Overall, there were only 10 quantitative studies that included all demographic information. The studies were conducted in different LMICs, including Nepal, India, Bangladesh, Sri Lanka, Pakistan, Tanzania, Nigeria, Indonesia, Zimbabwe, and Mongolia.
Categories in the studies reviewed
Environmental barriers
Eleven studies reported several environmental issues, including poor access to the physical environment, inappropriate wheelchairs, inadequate healthcare and rehabilitation services, no access to the medicines and healthcare, limited financial resources, and government policies which are considered challenges for SCI individuals to reintegrate into the community [15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25]. Living in rural areas is one of the significant barriers for people with SCI; the same was reported in a study conducted on 73 SCI participants in the rural areas of Kashmir and Pakistan, where the author addressed the earthquake reconstruction and rehabilitation as an unrealistic and poorly thought-out program. Participants in the study stated that they turned down the idea since it was difficult for them to leave their homes to do any work because there was no road accessible [26]. In addition, the literature supports that the current healthcare system in Mongolia is inadequate for the SCI population due to a lack of knowledge and well-trained rehabilitation experts [24]. Even secondary health issues arose due to a lack of competent and skilled care [24]. In addition, policy barriers, as well as the disability legislation, were reported in two studies [21, 24]. The Craig handicap assessment and reporting technique short form (CHART-SF) was chosen as the assessment tool in a quantitative study. The lowest average score was related to policy barriers because the majority of the participants were unaware of the government’s policies. Although most government programs encourage community reintegration, they have proven to be practically ineffective [21, 24].
Psychological barriers
Five studies [15, 27, 28, 29, 30] reported psychological barriers. The study participants reported their injuries as a life-altering event that brought them depression, anxiety, shock, failure, dependency, and hopelessness. A study on psychosocial factors among the Nepalese SCI population revealed that resilience was linked to demographic parameters such as gender, employment, and living place. As a result, interventions or rehabilitation should be targeted at specific psychosocial and demographic characteristics to increase community involvement among people with SCI [29]. The prevalence of depressed mood among individuals with traumatic SCI and the burden of caregiving among caregivers was high [27].
Another study conducted on Sri Lankan population used descriptive thematic analysis to illuminate psychological barriers. Participants in the study shared their feelings about how SCI has damaged their relationships. They rely entirely on their spouse like a child and cannot spend much time with their family. They were depressed as a result of these circumstances [31]. Female participants frequently mentioned broken family ties, although the nature of these breakups was different. Female participants expressed dissatisfaction with their inability to participate in family activities as they did before. Young adults, on the other hand, felt gloomy because they could not follow their careers as they desired before the injury. All preceding observations can be expressed as feelings of loneliness, hopelessness, and emptiness in the SCI individuals. Participants feel guilty about not being able to help or support their families. These feelings affect their quality of life and become barriers to participation in the community.
Cultural barriers
Two studies discussed the factors which comprise the cultural barriers: negligence, discrimination, stigma, negative attitude from the society and family members, acceptance, and gendered biases [24, 26]. The negative attitude of society and families toward SCI individuals after their injury was reported in a study conducted on the Mongolian population [24]. The findings of the study reported discrimination in the families (e.g., not being accepted by the girlfriend’s family), at work (e.g., not being hired because the recruiter did not feel they were capable of performing the job or being paid less), and in society (e.g., people believe that persons with disabilities are paying for previous bad deeds). In addition, the issue of gender biases was reported in a study conducted in six villages of Bagh District, Kashmir, and Pakistan; the findings revealed that the women were socially, emotionally, and financially isolated. In contrast, men received full social and emotional support from their families and friends. SCI women have a high degree of anxiety, depression, a sense of helplessness, and a cynical view of life due to the gendered biases and the concept of remarriages [26].
Secondary health conditions
Four quantitative [19, 20, 23, 32] and one qualitative [33] studies reported several secondary health complications, including the high occurrence of pressure sores, urinary tract infections, pain, neurogenic bladder, spasticity, contracture, tightness, and sleep problems, which were considered key factors for reducing the mobility and community participation in individuals with SCI. The spinal cord injuries secondary conditions scale (SCI-SCS) is a standardized and validated 16-item questionnaire used in a study to measure secondary complications, such as pressure ulcers, respiratory problems, postural hypotension, spasticity, and pain [19]. According to published studies, pressure ulcers are prevalent in people with SCI who live in LMICs [19, 34, 35]. Pressure ulcers are expected to be preventable with simple, low-cost methods, such as regular position changes and the use of cushions on wheelchairs [36]. These factors suggest that measures to prevent pressure ulcers should be prioritized in LMICs to increase the survival of spinal cord injury individuals after discharge from the hospital.
Facilitators
Five studies [30, 31, 37, 38, 39] revealed the characteristics that help people favorably manage SCI. Religious practice was the most common method for dealing with chronic problems. Generally, SCI participants relied on spiritual practices for comfort, consolation, and inner calm, especially during tough times. Some believed that religious figures were also responsible for or assisted in improving their physical conditions. SCI prompted not only religious yearning but also religious intensification in study participants. Karma also strongly impacted individuals’ attitudes and psychological health [31]. A study in Nepal reported that positive assets, such as self-efficacy, resilience, and social support, contribute considerably to health and buffer against adverse outcomes [15]. Subject wellbeing was found to have significant solid relationships with age, self-efficacy, and social support. For further validation of these findings, longitudinal and or experimental research is obligatory [15]. Moreover, a greater emphasis should be put on family involvement in SCI rehabilitation for social integration [38]. This issue had been proven statistically in a study where the Craig Handicap Assessment and Reporting Technique (CHART) scale was used to measure social integration after SCI [38].
4. Discussion
Overall findings of the review showed the diverse experience of 2692 SCI participants in 26 studies (qualitative and quantitative) that elucidate the barriers and facilitators of the SCI people’s reintegration into the community in low- and middle-income countries. This systematic review yielded enormous evidence reporting that physical environmental factors (such as access to public places, public transport, financial constraints, and unemployment) are the major hindrances for the SCI people to reintegrate into the community. Dorjbal et al. used an explorative qualitative study design with semi-structured interviews to study the lived experience of individuals with SCI in Mongolia. The study’s findings helped describe environmental barriers that impacted the development of secondary health conditions, limited activities, and participation in almost all areas of life. It has been seen that people with SCI often use healthcare services as compared to people without disabilities due to their secondary complications such as sepsis, pressure ulcers, and urinary tract infection [33, 40], and this condition impacts their quality of life [41, 42]. Hossain et al. (2016) conducted a mixed retrospective-prospective cohort design to determine survival after SCI in LMICs like Bangladesh. Findings of the study supported that cushions on wheelchairs and foam overlays on beds would help prevent the deaths amongst SCI individuals due to sepsis and pressure ulcers [19].
Furthermore, the present study observed the interrelationship between the barriers. If a person gets an appropriate healthcare facility, including appropriate wheelchairs, roads, and transportation for mobility, he or she is unlikely to bother about cultural and psychological issues. Environmental constraints mainly cause discrimination and a lack of confidence in SCI patients, leaving them completely reliant on their caregivers [24, 43]. A cross-sectional study was conducted by Muller et al. (2015). Their conclusion supported that those SCI individuals with better social support took lower scores in depression and higher scores in QoL [44].
Further, the United Nations stressed the significance of accessibility for individuals with physical disabilities to engage in community activities and considered the physical environmental barriers such as homes and public spaces, as well as public transit around the world [45, 46]. Due to limited transportation, mobility, and social impediments in LMICs, reintegration into society is a major challenge for SCI individuals. On the contrary, developed countries have shown a better quality of life than LMICs in terms of medical management, rate of morbidity/mortality, access to the physical environment, proper equipment, and so on [46]. People with SCI face various social hurdles, including low patient and family education, friend and family relationships, financial restrictions, unemployment, and social prejudices. The identified barriers regarding patient and family education during this review were further supported by studies that proved that enough knowledge and training skills were very useful to adjust to SCI [47]. Whereas unemployment and lack of vocational training after SCI are the substantial roadblocks that place a financial burden on the SCI individuals and their families [29, 48].
As per WHO factsheets, the global unemployment rate is more than 60% amongst the SCI population [49]. Published studies indicate that employment rates in low-resource countries range from 7% to 41% [18, 48]. Unemployment and low income may result in financial difficulties, an important factor affecting the QoL of people with SCI [16]. Financial hardships may also be associated with emotional problems. Studies indicate that unemployment rates are 10 times higher among SCI patients compared with the general population [20, 21, 50, 51]. Access to the place of work, employer attitudes, and patients’ beliefs in their abilities may influence the decision to resume employment after SCI. Singh R et al. (2007) found that employment status was associated with a higher QoL among those with SCI living in India [41]. Moreover, government policies, particularly social policies, significantly impact the participation of SCI people with physical disabilities [21, 26]. Social support, education level, financial standing, job security, and involvement in social and recreational activities have all been identified as factors that may affect a person’s ability to adjust to SCI.
The present systematic review also highlighted the facilitators that help SCI individuals overcome the hurdles mentioned above and help them participate in the community. A cross-sectional questionnaire-based study was conducted on the Sri Lankan population by Xue S et al. (2016). The study’s findings emphasized the need for rehabilitative programming to support patients’ spirituality/religiosity activities and mental wellbeing [37]. The most frequent approach for dealing with personal concerns was a religious practice. A similar study based on a focus group research design examined the coping mechanism after SCI. The findings suggested that spiritual practices provided solace, consolation, and inner quiet to participants, especially during difficult times, helping them participate in community activities well [31]. Social support provides a fundamental role in both depression and adjustment of SCI individuals. Persons who enjoy more social support recognize them as the reason behind the improvement in their condition. They are less emotionally distressed and report better life satisfaction and quality of life [38].
5. Conclusion
In conclusion, environmental, psychological, cultural, and health-related issues hamper SCI individuals from participating in the community. The majority of studies highlight specific key difficulties associated with these hurdles, such as acceptability, affordability, and accessibility, which include social/self/family acceptance, financial restrictions, lack of employment, and access to places, toilets, and residences. Furthermore, research has revealed that coping strategies such as spirituality/religiosity and family/friends support are essential for SCI people to reintegrate into the community fully. Individuals with SCI and their families should be an integral part of the rehabilitation team, as this will help them comprehend the effects of the injury and decrease the psychological burden. Healthcare professionals could strengthen the patient-provider interaction by establishing short- and long-term treatment goals such as independence, vocational training, a positive attitude, and counseling-spousal involvement, considering patients’ clinical and demographic variables. Working on the abovementioned issues can help SCI people in low- and middle-income countries become more integrated into their communities.
Ethical Considerations
Compliance with ethical guidelines
There was no use of human volunteers/animals during this research.
Funding
No funding has been availed for this study.
Authors' contributions
The datasets generated and analyzed during the current review study are available from the corresponding author upon reasonable request.
Conflict of interest
We certify that there is no actual or potential conflict of interest concerning this review.
Acknowledgments
References
- Burns AS, O’Connell C. The challenge of spinal cord injury care in the developing world. The Journal of Spinal Cord Medicine. 2012;35(1):3-8. [DOI:10.1179/2045772311Y.0000000043] [PMID] [PMCID]
- Kumar R, Lim J, Mekary RA, Rattani A, Dewan MC, Sharif SY, et al. Traumatic spinal injury: Global epidemiology and worldwide volume. World Neurosurg. 2018; 113:e345-63. [DOI:10.1016/j.wneu.2018.02.033] [PMID]
- Arsh A, Darain H, Haq ZU, Zeb A, Ali I, Ilyas SM. Epidemiology of spinal cord injuries due to bomb blast attacks, managed at paraplegic centre peshawar, pakistan: a nine years retrospective study. Khyber Medical University Journal. 2017; 9(2).55-9. https://www.kmuj.kmu.edu.pk/article/view/16814
- Chiu WT, Lin HC, Lam C, Chu SF, Chiang YH, Tsai SH. Epidemiology of traumatic spinal cord injury: Comparisons between developed and developing countries. Asia-Pacific Journal of Public Health. 2010; 22(1):9-18. [DOI:10.1177/1010539509355470] [PMID]
- Devivo MJ. Epidemiology of traumatic spinal cord injury: Trends and future implications. Spinal Cord. 2012; 50(5):365-72. [DOI:10.1038/sc.2011.178] [PMID]
- Simpson LA, Eng JJ, Hsieh JTC, Wolfe DL. The health and life priorities of individuals with spinal cord injury: A systematic review. Journal of Neurotrauma. 2012; 29(8):1548-55. [DOI:10.1089/neu.2011.2226] [PMID] [PMCID]
- Lines LM, Lepore M. Patient-centered, person-centered, and person-directed care. Medical Care. 2015; 53(7):561-3. [DOI:10.1097/MLR.0000000000000387] [PMID]
- Linnenluecke MK, McKnight B. Community resilience to natural disasters: the role of disaster entrepreneurship. Journal of Enterprising Communities. 2017; 11(1):166-85. [DOI:10.1108/JEC-01-2015-0005]
- The World Bank. Lower middle income [Internet] 2021. [Cited 10 Nov 2021]. Available from: https://data.worldbank.org/country/XN
- Jackson N, Waters E. Criteria for the systematic review of health promotion and public health interventions. Health Promotion International. 2005; 20(4):367-74. [DOI:10.1093/heapro/dai022] [PMID]
- Odell M, Victor C, Oliver D. Nurses’ role in detecting deterioration in ward patients: Systematic literature review. Journal of Advanced Nursing. 2009; 65(10):1992-2006. [DOI:10.1111/j.1365-2648.2009.05109.x] [PMID]
- Dixon-Woods M, Sutton A, Shaw R, Miller T, Smith J, Young B, Bonas S, Booth A, Jones D. Appraising qualitative research for inclusion in systematic reviews: a quantitative and qualitative comparison of three methods. Journal of Health Services Research & Policy. 2007; 12(1):42-7. [DOI:10.1258/135581907779497486] [PMID]
- Braun V, Clarke V, Braun V, Clarke V. Applied qualitative research in psychology. Applied Qualitative Research in Psychology. 2006; 3(2):77-101. https://www.research.manchester.ac.uk/portal/en/publications/applied-qualitative-research-in-psychology(469b4d19-ed03-47fa-8e28-1f57f66fc2ca).html
- Kumar N, Gupta B. Effect of spinal cord injury on quality of life of affected soldiers in India: a cross-sectional study. Asian Spine Journal. 2016; 10(2):267. [DOI:10.4184/asj.2016.10.2.267] [PMID] [PMCID]
- Bhattarai M, Jin Y, Smedema SM, Cadel KR, Baniya M. The relationships among self‐efficacy, social support, resilience, and subjective well‐being in persons with spinal cord injuries. Journal of Advanced Nursing. 2021; 77(1):221-30. [DOI:10.1111/jan.14573] [PMID]
- Ganesh S, Mishra C. Physical activity and quality of life among adults with paraplegia in Odisha, India. Sultan Qaboos University Medical Journal. 2016; 16(1):e54. [DOI:10.18295/squmj.2016.16.01.010] [PMID] [PMCID]
- Kader M, Perera NK, Sohrab Hossain M, Islam R. Socio-demographic and injury-related factors contributing to activity limitations and participation restrictions in people with spinal cord injury in Bangladesh. Spinal Cord. 2018; 56(3):239-46. [DOI:10.1038/s41393-017-0001-y] [PMID]
- Gupta N, Solomon J, Raja K. Employment after paraplegia in India: A postal survey. Spinal Cord. 2011; 49(7):806-11. [DOI:10.1038/sc.2011.1] [PMID]
- Hossain MS, Rahman MA, Herbert RD, Quadir MM, Bowden JL, Harvey LA. Two-year survival following discharge from hospital after spinal cord injury in Bangladesh. Spinal Cord. 2016; 54(2):132-6. [DOI:10.1038/sc.2015.92] [PMID]
- Scovil CY, Ranabhat MK, Craighead IB, Wee J. Follow-up study of spinal cord injured patients after discharge from inpatient rehabilitation in Nepal in 2007. Spinal Cord. 2012; 50(3):232-7.[DOI:10.1038/sc.2011.119] [PMID]
- Sekaran P, Vijayakumari F, Hariharan R, Zachariah K, Joseph SE, Senthil Kumar RK. Community reintegration of spinal cord-injured patients in rural south India. Spinal Cord. 2010; 48(8):628-32. [DOI:10.1038/sc.2010.6] [PMID]
- Kalyani HH, Dassanayake S, Senarath U. Effects of paraplegia on quality of life and family economy among patients with spinal cord injuries in selected hospitals of Sri Lanka. Spinal Cord. 2015; 53(6):446-50. [DOI:10.1038/sc.2014.183] [PMID]
- Hossain MS, Islam M, Rahman M, Glinsky JV, Herbert RD, Ducharme S, et al. Health status, quality of life and socioeconomic situation of people with spinal cord injuries six years after discharge from a hospital in Bangladesh. Spinal Cord. 2019; 57(8):652-61. [DOI:10.1038/s41393-019-0261-9] [PMID]
- Dorjbal D, Prodinger B, Zanini C, Avirmed B, Stucki G, Rubinelli S. Living with spinal cord injury in Mongolia: A qualitative study on perceived environmental barriers. The Journal of Spinal Cord Medicine. 2020; 43(4):518-31. [DOI:10.1080/10790268.2019.1565707] [PMID] [PMCID]
- Moshi H, Sundelin G, Sahlen KG, Sörlin A. Quality of life of persons with traumatic spinal cord injury in rural Kilimanjaro, Tanzania: a community survey. Disability and rehabilitation. 2021; 43(20):2838-45. [DOI:10.1080/09638288.2020.1718780] [PMID]
- Irshad H, Mumtaz Z, Levay A. Long‐term gendered consequences of permanent disabilities caused by the 2005 Pakistan earthquake. Disasters. 2012; 36(3):452-64. [DOI:10.1111/j.1467-7717.2011.01265.x] [PMID]
- Adhikari SP, Gurung G, Khadka B, Rana C. Factors influencing depression in individuals with traumatic spinal cord injury and caregivers’ perceived burden in a low-income country: A cross-sectional study. Spinal Cord. 2020; 58(10):1112-8. [DOI:10.1038/s41393-020-0451-5] [PMID]
- Atobatele KO, Olaleye OA, Fatoye FA, Hamzat TK. Relationships between community reintegration and clinical and psychosocial attributes in individuals with spinal cord injury in a Nigerian City. Topics in Spinal Cord Injury Rehabilitation. 2018; 24(4):306-14. [DOI:10.1310/sci16-00055] [PMID] [PMCID]
- Bhattarai M, Maneewat K, Sae-Sia W. Psychosocial factors affecting resilience in Nepalese individuals with earthquake-related spinal cord injury: a cross-sectional study. BMC Psychiatry. 2018; 18(1):1-8. [DOI:10.1186/s12888-018-1640-z] [PMID] [PMCID]
- Bhattarai M, Maneewat K, Sae-Sia W. Determinants of resilience among people who sustained spinal cord injury from the 2015 earthquake in Nepal. Spinal Cord. 2018; 56(1):78-83. [DOI:10.1038/sc.2017.93] [PMID]
- Arya S, Xue S, Embuldeniya A, Narammalage H, da Silva T, Williams S, Ravindran A. Coping strategies used by traumatic spinal cord injury patients in Sri Lanka: A focus group study. Disability and Rehabilitation. 2016; 38(20):2008-15. [DOI:10.3109/09638288.2015.1111433] [PMID]
- Darain H, Ullah I, Dildar M, Ibrar M. Long-Term Challenges to Patients with Spinal Cord Injuries. Physikalische Medizin, Rehabilitationsmedizin, Kurortmedizin. 2017; 27(3):160-3. [DOI:10.1055/s-0043-104053]
- Øderud T. Surviving spinal cord injury in low income countries. African Journal of Disability. 2014; 3(2):1-9. [DOI:10.4102/ajod.v3i2.80] [PMID] [PMCID]
- Levy LF, Makarawo S, Madzivire D, Bhebhe E, Verbeek N, Parry O. Problems, struggles and some success with spinal cord injury in Zimbabwe. Spinal Cord. 1998; 36(3):213-8. [DOI:10.1038/sj.sc.3100574] [PMID]
- Zakrasek EC, Creasey G, Crew JD. Pressure ulcers in people with spinal cord injury in developing nations. Spinal Cord. 2015; 53(1):7-13. [DOI:10.1038/sc.2014.179] [PMID]
- National Pressure Ulcer Advisory Panel European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Quick Reference Guide. Clinical Practice Guideline [Internet]. 2014. 1-75. Available from: https://www.epuap.org/wp-content/uploads/2016/10/quick-reference-guide-digital-npuap-epuap-pppia-jan2016.pdf
- Xue S, Arya S, Embuldeniya A, Narammalage H, da Silva T, Williams S, Ravindran A. Perceived functional impairment and spirituality/religiosity as predictors of depression in a Sri Lankan spinal cord injury patient population. Spinal Cord. 2016; 54(12):1158-63. [DOI:10.1038/sc.2016.56] [PMID]
- Samuelkamaleshkumar S, Radhika S, Cherian B, Elango A, Winrose W, Suhany BT, Prakash MH. Community reintegration in rehabilitated South Indian persons with spinal cord injury. Archives of Physical Medicine and Rehabilitation. 2010; 91(7):1117-21.[DOI:10.1016/j.apmr.2010.04.005] [PMID]
- Moshi H, Sundelin G, Sahlen KG, Sörlin A. Quality of life of persons with traumatic spinal cord injury in rural Kilimanjaro, Tanzania: a community survey. Disability and Rehabilitation. 2021; 43(20):2838-45. [DOI:10.1080/09638288.2020.1718780] [PMID]
- Ronca E, Scheel-Sailer A, Koch HG, Gemperli A. Health care utilization in persons with spinal cord injury: part 2—determinants, geographic variation and comparison with the general population. Spinal Cord. 2017; 55(9):828-33. [DOI:10.1038/sc.2017.44] [PMID]
- Singh R, Dhankar SS, Rohilla R. Quality of life of people with spinal cord injury in Northern India. International Journal of Rehabilitation Research. 2008; 31(3):247-51. [DOI:10.1097/MRR.0b013e3282fb7d25] [PMID]
- Jensen MP, Truitt AR, Schomer KG, Yorkston KM, Baylor C, Molton IR. Frequency and age effects of secondary health conditions in individuals with spinal cord injury: a scoping review. Spinal Cord. 2013; 51(12):882-92. [DOI:10.1038/sc.2013.112] [PMID]
- Hammel J, Magasi S, Heinemann A, Gray DB, Stark S, Kisala P, et al. Environmental barriers and supports to everyday participation: a qualitative insider perspective from people with disabilities. Archives of Physical Medicine and Rehabilitation. 2015; 96(4):578-88. [DOI:10.1016/j.apmr.2014.12.008] [PMID]
- Müller R, Peter C, Cieza A, Post MW, Van Leeuwen CM, Werner CS, et al. Social skills: a resource for more social support, lower depression levels, higher quality of life, and participation in individuals with spinal cord injury?. Archives of Physical Medicine and Rehabilitation. 2015; 96(3):447-55. [DOI:10.1016/j.apmr.2014.09.006] [PMID]
- Whiteneck GG, Harrison-Felix CL, Mellick DC, Brooks CA, Charlifue SB, Gerhart KA. Quantifying environmental factors: A measure of physical, attitudinal, service, productivity, and policy barriers. Archives of Physical Medicine and Rehabilitation. 2004; 85(8):1324-35. [DOI:10.1016/j.apmr.2003.09.027] [PMID]
- Hill H. Disability and accessibility in the library and information science literature: A content analysis. Library & Information Science Research. 2013; 35(2):137-42. [DOI:10.1016/j.lisr.2012.11.002]
- Chhabra HS, Bhalla AM. Influence of socio-economic status on access to different components of SCI management across Indian population. Spinal Cord. 2015; 53(11):816-20. [DOI:10.1038/sc.2015.80] [PMID]
- Dijkers MP. Quality of life of individuals with spinal cord injury: a review of conceptualization, measurement, and research findings. Journal of rehabilitation research and development. 2005; 42(3):87. [DOI:10.1682/JRRD.2004.08.0100] [PMID]
- World Health Organization. Spinal cord injury [Internet] 2013. [Last Updated 19 November 2013]. Available from: https://www.who.int/news-room/fact-sheets/detail/spinal-cord-injury
- Carpenter C, Forwell SJ, Jongbloed LE, Backman CL. Community Participation After Spinal Cord Injury. Archives of Physical Medicine and Rehabilitation. 2007; 88(4):427-33. [DOI:10.1016/j.apmr.2006.12.043] [PMID]
- Babamohamadi H, Negarandeh R, Dehghan-Nayeri N. Barriers to and facilitators of coping with spinal cord injury for Iranian patients: A qualitative study. Nursing & Health Sciences. 2011; 13(2):207-15. [DOI:10.1111/j.1442-2018.2011.00602.x] [PMID]
Type of Study: Review Article |
Subject:
Physiotherapy
Received: 2022/03/3 | Accepted: 2022/04/10 | Published: 2022/02/3
Received: 2022/03/3 | Accepted: 2022/04/10 | Published: 2022/02/3
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







.jpg)
