Volume 3, Issue 1 (Continuously Updated 2020)
Func Disabil J 2020, 3(1): 195-204 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Masoudi P, Mansour Sohani S, Amiri A. Evaluation of Hip Frontal Plane Flexibility and Strength in Male Sprinter Runners With Unilateral Patellofemoral Arthropathy: A Case-Control Study. Func Disabil J 2020; 3 (1) :195-204
URL: http://fdj.iums.ac.ir/article-1-147-en.html
URL: http://fdj.iums.ac.ir/article-1-147-en.html
1- Department of Physiotherapy, Iranian Center of Excellence in Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Physiotherapy, Iranian Center of Excellence in Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran. ,mansorsohani.s@iums.ac.ir
2- Department of Physiotherapy, Iranian Center of Excellence in Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 2006 kb]
(670 Downloads)
| Abstract (HTML) (2381 Views)
Full-Text: (1021 Views)
1. Introduction
Patellofemoral Pain Syndrome (PFPS) is an overuse syndrome usually characterized by an aching pain in the peripatellar area. The terminology PFPS has been used as the preferred term in recent years; however, it does not consider how non-painful joint conditions could be a precursor to pain development, does not include symptoms, such as crepitus, and may increase a focus on the ‘pain’ aspect of the condition. The alternative term, Patellofemoral Arthropathy (PFA), was proposed, which indicates that PFP may be a symptom of joint disease [1]. Physical activities, such as climbing stairs, squatting, jumping, running, and two or four kneeling positions for prolonged periods of time will deteriorate PFP. PFA is the most common knee disorder in runners [2, 3]. PFA has been reported as the cause of 20% to 40% of all visits to physical therapy and sport medicine clinics as a result of knee pain. PFA symptoms can lead to impairments during sport and functional and daily life activities. Various factors can lead to the development of PFA symptoms, which makes the diagnosis of the cause of symptoms and designing a rehabilitation program extremely difficult [4].
One etiological theory to PFA is that poor proximal neuromuscular control and/or weakness of the hip musculature may lead to poor control of frontal and transverse plane motions of the hip [5]. For example, excessive hip adduction, hip internal rotation, and the following knee abduction have been hypothesized to increase patellofemoral joint stress and affect the patellofemoral joint biomechanics. Furthermore, during weight-bearing activities, this situation has been proposed to increase the dynamic quadriceps angle, which finally results in intensified patella-femoral joint stress [5, 6]. Some investigations have demonstrated that females and males with PFA display altered knee joint kinematics in comparison with non-involved control participants. Particularly, symptomatic PFA patients exhibit increased frontal plane knee joint motion and knee joint loading during dynamic activities, such as running [7, 8, 9].
Thus, hip abductors strengthening is often advocated to improve hip mechanics to reduce the incidence of or symptoms related to PFA [10]. In addition to these findings, one study suggested that strengthening alone may be insufficient to alter abnormal movement patterns of the lower extremities during running [11]. Despite large and significant gains in the strength of hip abductors and hip external rotators following exercise protocols, no changes have been seen in abnormal hip mechanics during running. Accordingly, as suggested later, possibly additional therapeutic programs may be required, such as myofascial release, stretching, or neuromuscular retraining for hip strengthening to finally better manage such a syndrome [11, 12].
Hip adduction Range of Motion (ROM) has been suggested to be a predictor of pain and function in both males and females with PFA. It has been proposed that frontal plane motions of the hip and knee can raise the dynamic quadriceps angle during functional tasks. It has been reported that a 10° increase in the quadriceps angle can elevate patellofemoral stress by 45% [5, 6]. Task-dependent excessive functional limb Varus during running has been suggested as a possible reason for adductor overactivity and stiffness and the following abductor reciprocal inhibition [13]. It has also been reported that abductor muscles with the greatest hip abduction torque at the hip positioned at 10° adduction, along with the hip position during single-leg stance, will help provide adequate stability to the pelvis [14].
Then, any changes in this position following changes or imbalances in adductor/adductor length or strength may contribute to PFA. Therefore, two questions may raise: Are there any muscular strength and flexibility changes in frontal plane hip muscles in runners with PFA? What is the relationship between flexibility and strength? Accordingly, the aim of this study was to compare abduction, adduction, and abduction to adduction flexibility and strength ratio to clarify the role of muscular strength, flexibility, and balance in sprinter runners with unilateral PFA.
2. Materials and Methods
Design
A total of 38 semiprofessional male sprinter runners declaring unilateral pain (3 or more on the numerical analog scale) or showing positive patellar grind test result on just one side were compared assigned to the legs and the control group (20 matched controls) regarding frontal plane muscle strength and flexibility in this case-control study. They were recruited using the non-probability sampling method from Tehran and Shiraz running clubs from April 2018 to January 2020.
Participants
The participants with PFA were excluded from the study if they had the following exclusion criteria: 1) a history of hip, knee, or ankle surgery over the past 3 years; 2) patellar dislocation; 3) any deviation in the lumbar vertebra; 4) systemic arthritis, knee ligament or meniscal injury; 5) plica syndrome, Sinding-Larsen-Johansson disease, Osgood-Schlatter disease; 6) any neurological disease [15]; and 7) bilateral PFA. Because no similar ROM studies had been performed on the frontal plane, we selected 10 pilot participants with NAS Activity Scale (NAS) peripatellar pain score of 3 or more or showing unilateral positive patellar grind test result. Following data analysis, we used a rule of thumb method to determine the sample size, which was determined to be 38 cases based on ROM data [16].
We also had to choose 20 of 26 cases for the control group and we evaluated and matched them with 20 PFA cases because of the prevalence of COVID-19 and no chances of more evaluation because of physical distancing rules. The qualifying participants were first informed about the study purpose and the study protocol. First, the participants were given a page consisting of the Numeric Pain Rating Scale (NPRS), where an 11-point scale ranging from 0 to 10 was anchored on the left with the phrase ‘‘no pain’’ and on the right with the phrase ‘‘worst imaginable pain.’’ Patients rated their pain within the last 24 hours. Numeric pain scales have been shown to be reliable and valid [17, 18]. They were then given the Persian version of the Functional Index Questionnaire (FIQ) for further investigation and possible correlations with functional impairment after the study. This questionnaire has been confirmed to be valid and reliable in Iran [19].
Procedure
To perform the study, we followed two different procedures; the participant’s flexibility was assessed first, and then, they were assessed with strength in two trials, with 5 minutes of resting period between the trials based on the average of two trials for comparison [20]. Hip adductor and abductor muscle flexibility were implied from hip adduction and abduction ROM indirectly. Both active and passive ROM was used for comparison. Because of using 2D motion analysis as the flexibility measurement, we marked a rectangle surface on the ground with the height of 2 m and the width of 1.5 m via indicator markers. Also, we marked 3 parts of participants’ leg and pelvis to measure the ROM: 1) right anterior superior iliac spine 2) left anterior superior iliac spine 3) a relative point to the femoral lateral epicondyle (3 cm upper and in the middle of thigh diameter up to patella bone). The subjects’ head was in the middle of the upper marked line and the camera tripod in the middle of the lower one. The angle of the camera was 20 degrees toward the surface in relation to the horizontal plane with the film recorded with consistent camera features getting ready to record and upload the video to software (Figure 1).
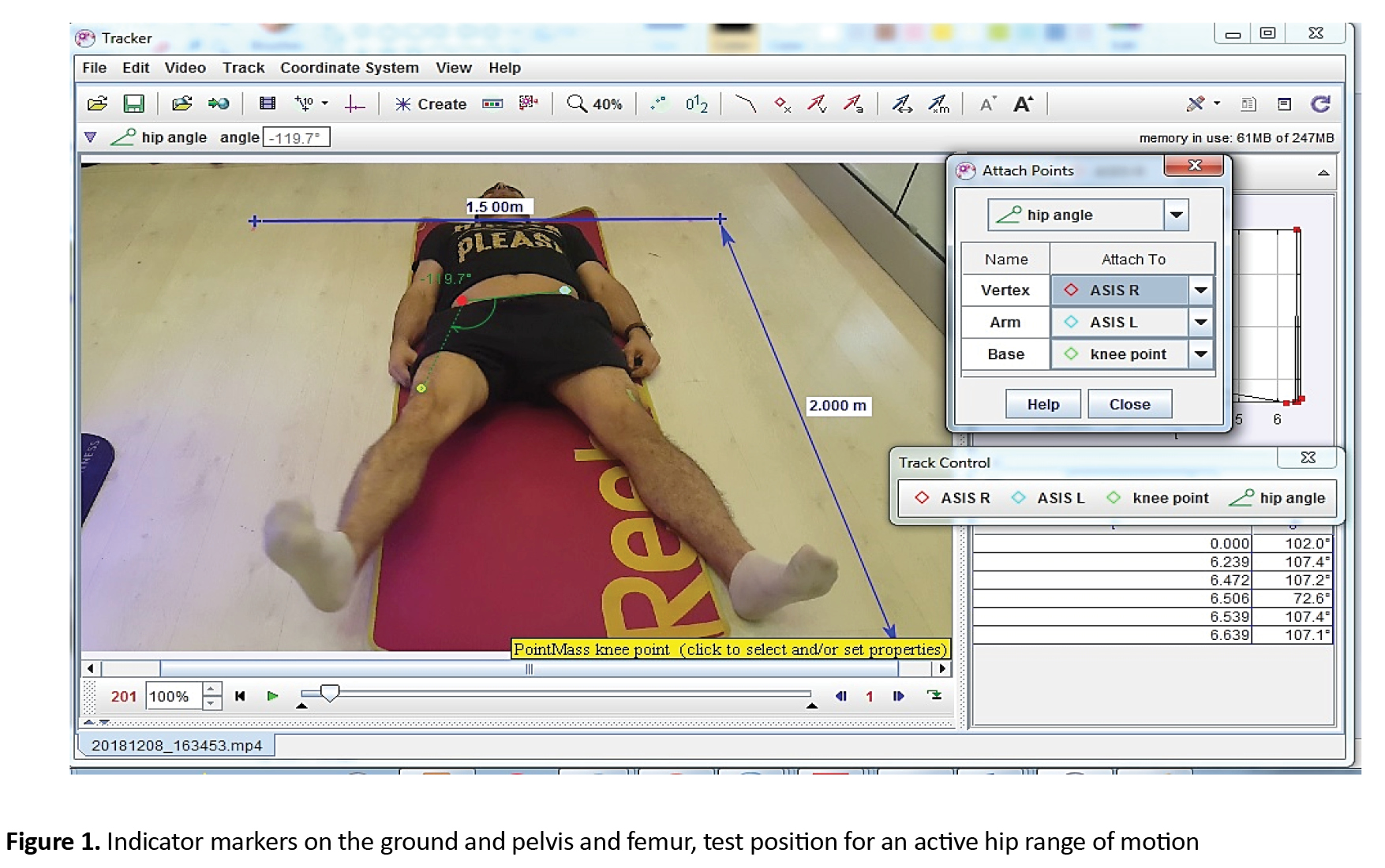
Once the filming project was done, we analyzed the films through 2D motion analysis software (Tracker 4.11 x Douglas Brown, Wolfgang Christian 2017). Cost-benefit and accessibility of 2D motion analysis have been already confirmed and it is a valid and reliable instrument in measuring joint ROM along with 3D motion analysis, which is too expensive and out of reach for sports studies, that are commonly performed outside the experimental parts [21, 22, 23, 24]. For analysis of the films, we chose 3 mass points and 1 protractor in the software environment. Then, we matched the marked points on the leg and pelvis to mass points in the software named R ASIS, L ASIS, and knee point and fixed them with vertex, arm, and base of the protractor to measure hip angles. Thereafter, we played the film and sought for ultimate pure hip adduction and abduction ROMs, free of additional rotational parts or pelvis movements. Next, we paused the film and noted the protractor’s number (in degrees) as hip ROM (Figure 1). All ROM data were normalized to the subject’s leg length to account for individual differences as we knew choosing mass points on the specific anatomical landmarks instead of the joint center may lead to adiposity influence on angles. Nevertheless, choosing a joint center will show variability in 2D motion analysis, as well [24].
The hip muscle strength was measured through a hand-held dynamometer (SF-500 push/pull force gauge; IMADA), which has been confirmed to be reliable when used by a single experienced tester [25, 26]. We measured force as opposed to torque as it is the standard measure commonly used in clinical practice. To accurately measure muscle force, we used a consistent and firm length strap at the end of the lower extremity preventing hip abduction identically for all participants and allowing abductors’ muscles to move in a more accurate kinesiology position according to their torque/hip angle curve as we knew measuring muscle strength at the end of abduction range will lead to muscle active insufficiency [14]. The participants were positioned on their sides and then asked to abduct their legs as far as the firm band allowed them. When the movement stopped, the dynamometer was placed on the lateral femoral epicondyle and they were asked to push as far as they could. Accordingly, the peak hip abduction isometric force (N) was measured. During the measurement, the dynamometer was placed between the legs on the medial femoral epicondyle with our hand and soft pad between the dynamometer and resting leg, and participants were asked to press toward the other leg as far as they could. The examiner did not try to overcome the subject’s effort (Figure 2).

These procedures were repeated two times with 5 minutes of resting based on the average for strength comparison. All strength data were normalized to body mass, which has been confirmed to be the best way to normalize strength in order to rule out any individual differences.
We used male samples only for two reasons: the first gender should be factored into analyses of allometric scaling as men have higher b-values than women for both force and torque [27]. Secondly, few studies have evaluated only a male sample.
Data analysis
We used the Kolmogorov-Smirnov test to check the differences in the baseline characteristics. The significance of the difference in abduction, adduction, and abduction to adduction ratio strength and flexibility between uninvolved and involved sides was determined using paired t-test and repeated measures ANOVA to compare with the control group. A correlation test was used to clarify the factors most relevant to dysfunction and pain, and also to distinguish any correlations between flexibility and strength. To determine the effect size, we used Cohen’s d, where a Cohen’s d 0/2 is a small effect, a Cohen’s d, 0.5 is a medium effect, and a 0.8 amount is considered a large effect [28]. The set of variables providing the best linear discrimination was selected. Statistical analyses were performed using SPSS v. 23 (SPSS Inc, Chicago, IL) and JASP 0.9.1 analysis software.
3. Results
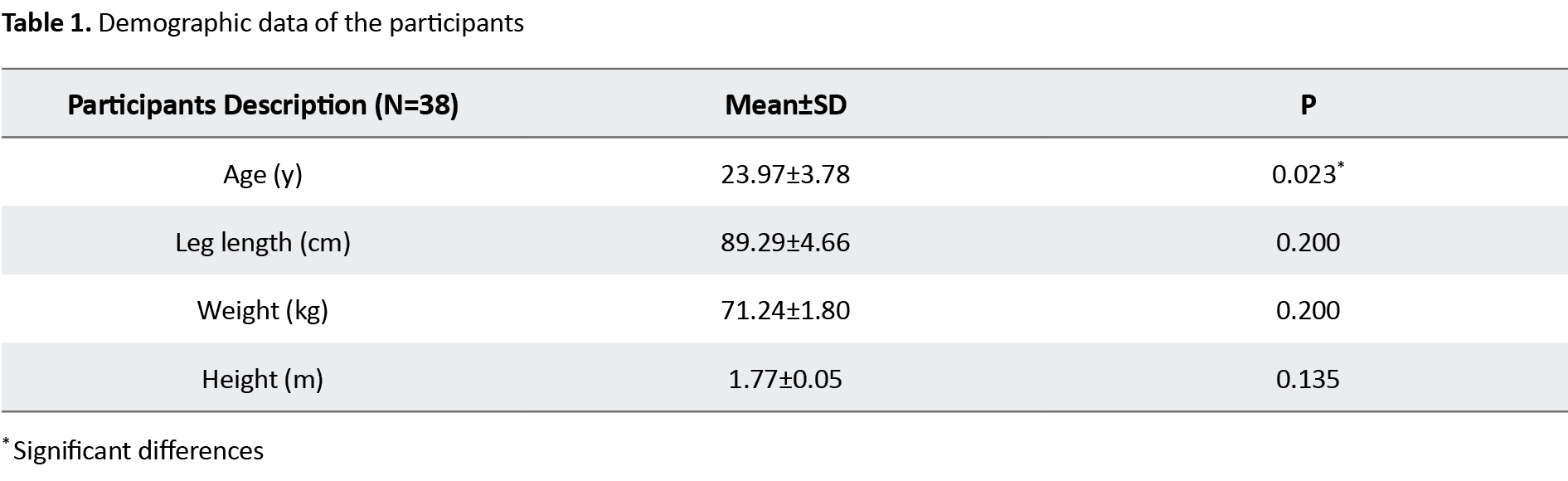
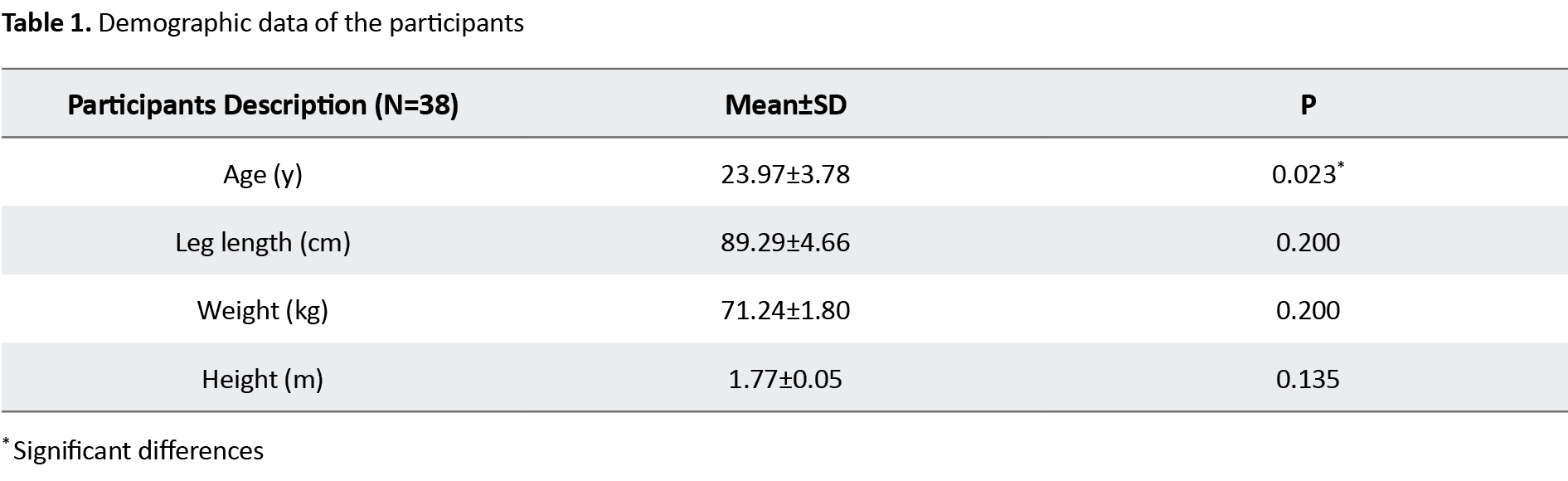
According to data analysis, the participants’ Mean±SD age was 23.46±4.01 years, height was 1.78±0.05 m, weight was 71.3±9.21 kg, Body Mass Index (BMI) was 22.45±2.30 kg/m2, and their leg length was 90.23±4.21 cm. Weight, leg length, height, and BMI had normal distributions (P>0.05), but a significant difference was seen for age between participants (P=0.023) (Table 1).
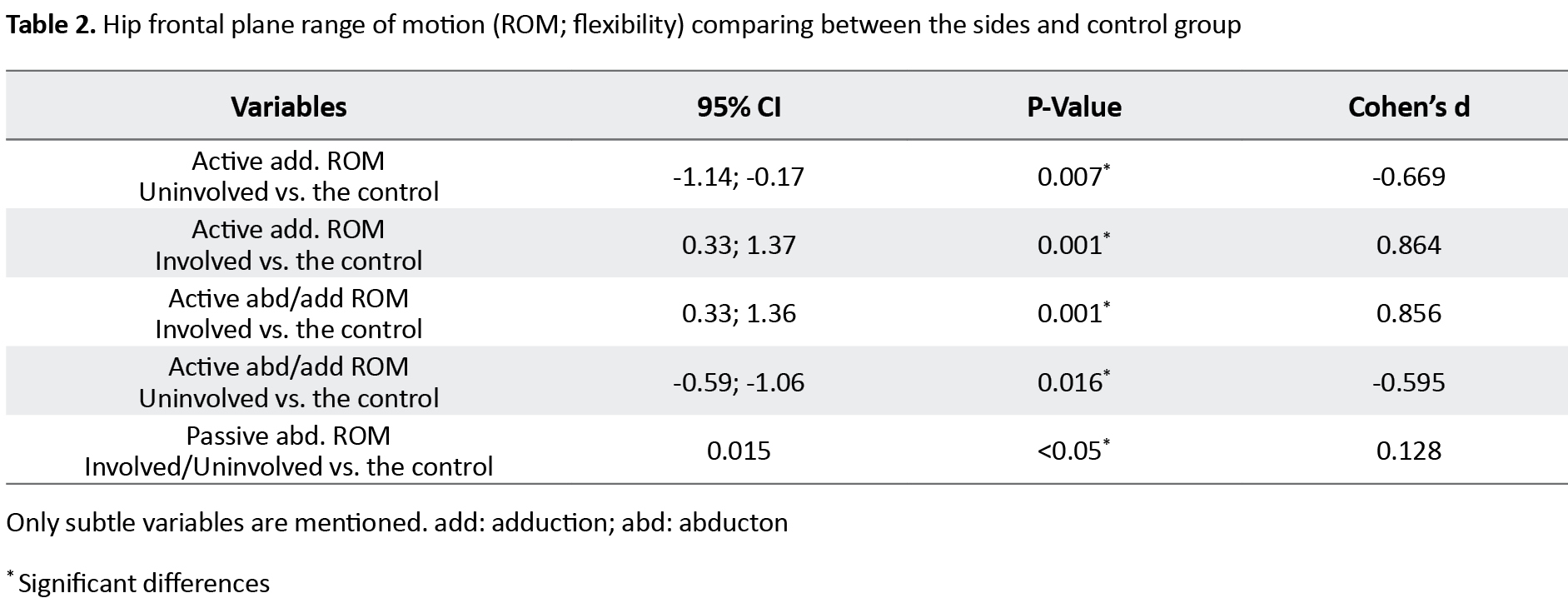
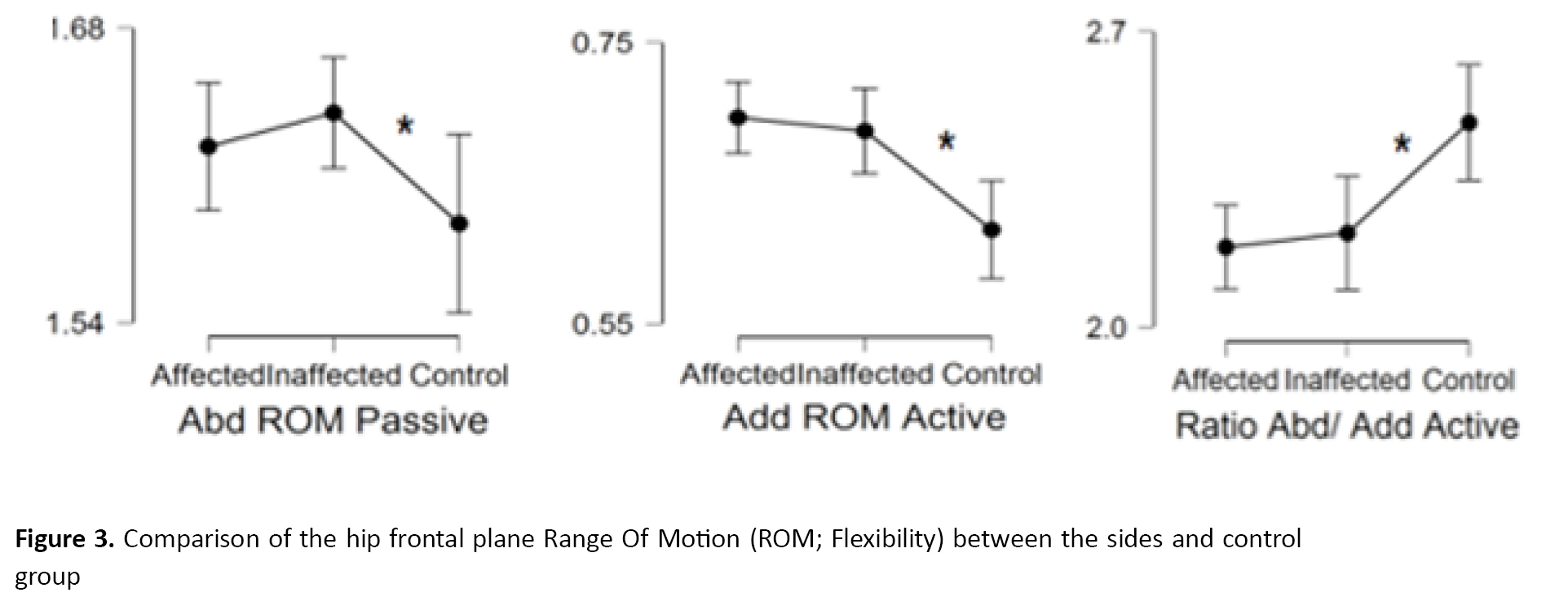
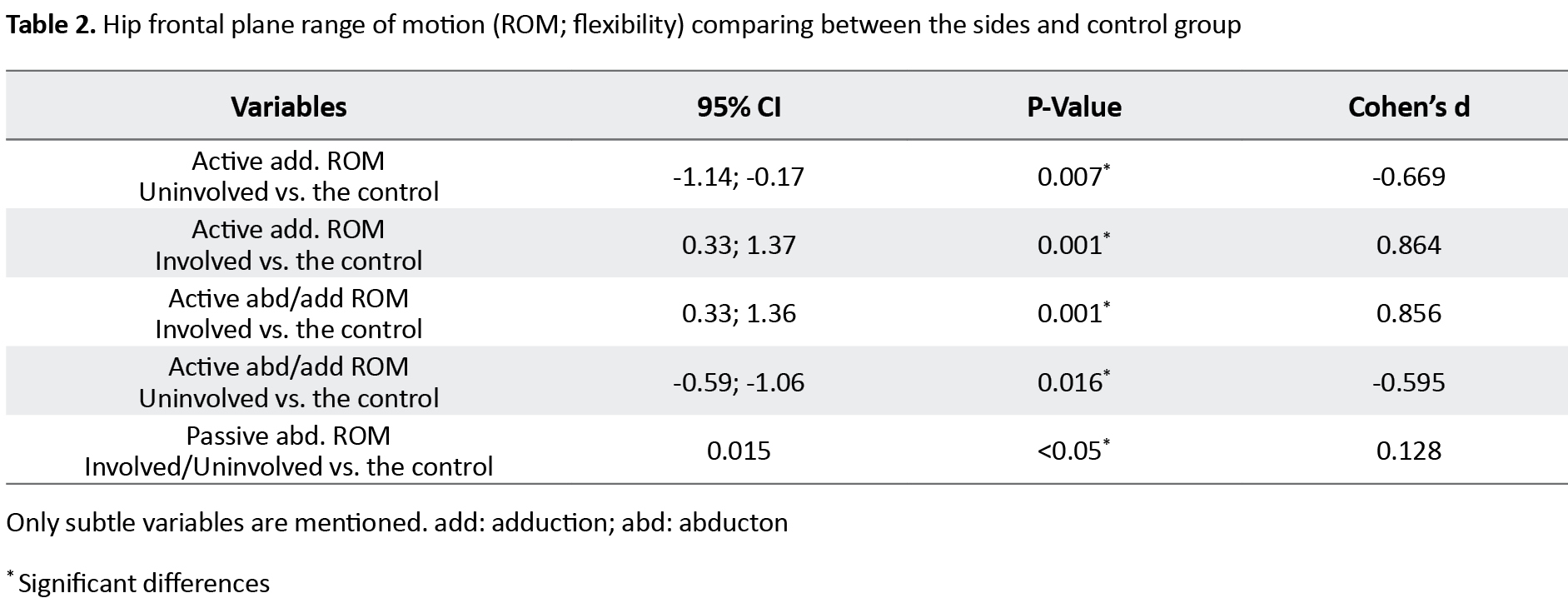
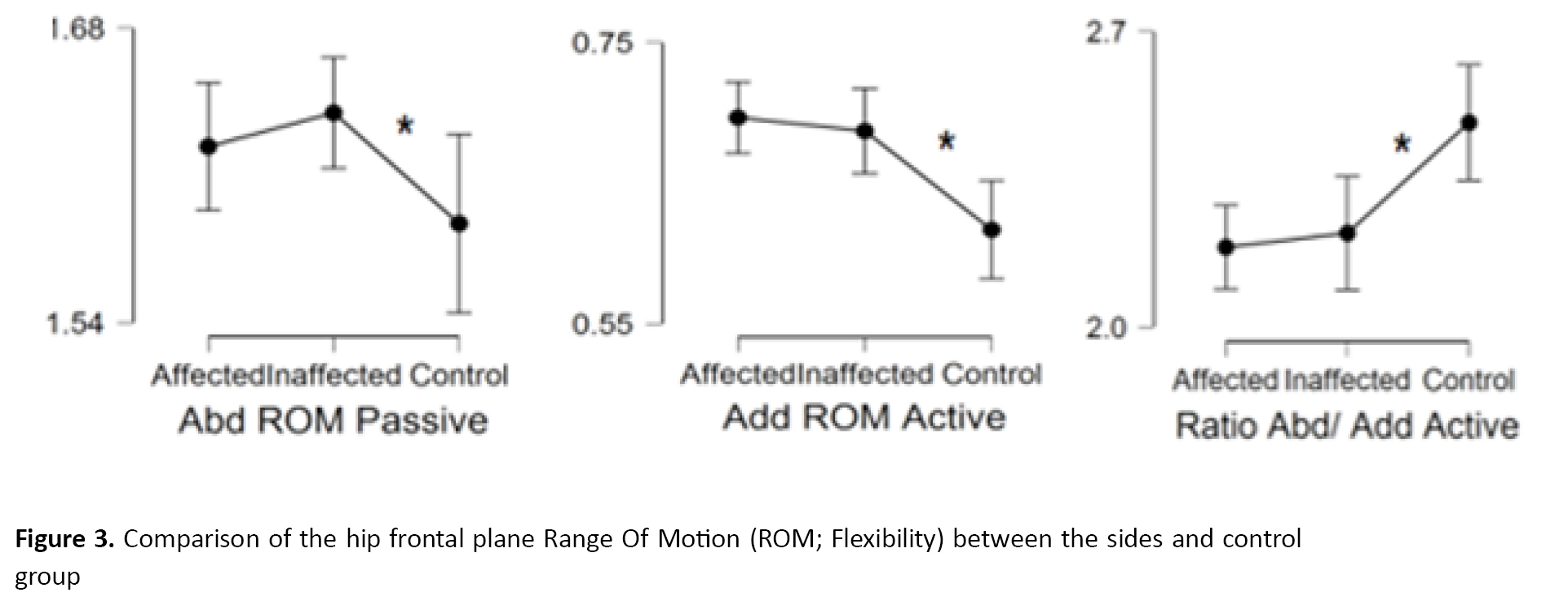
No differences were found in the active or passive abduction and adduction ROM between either side (P>0.005) but passive abduction and active adduction ROM were significantly greater in the control group (P<0.001) (Tables 2, 3) (Figure 3, 4, 5).
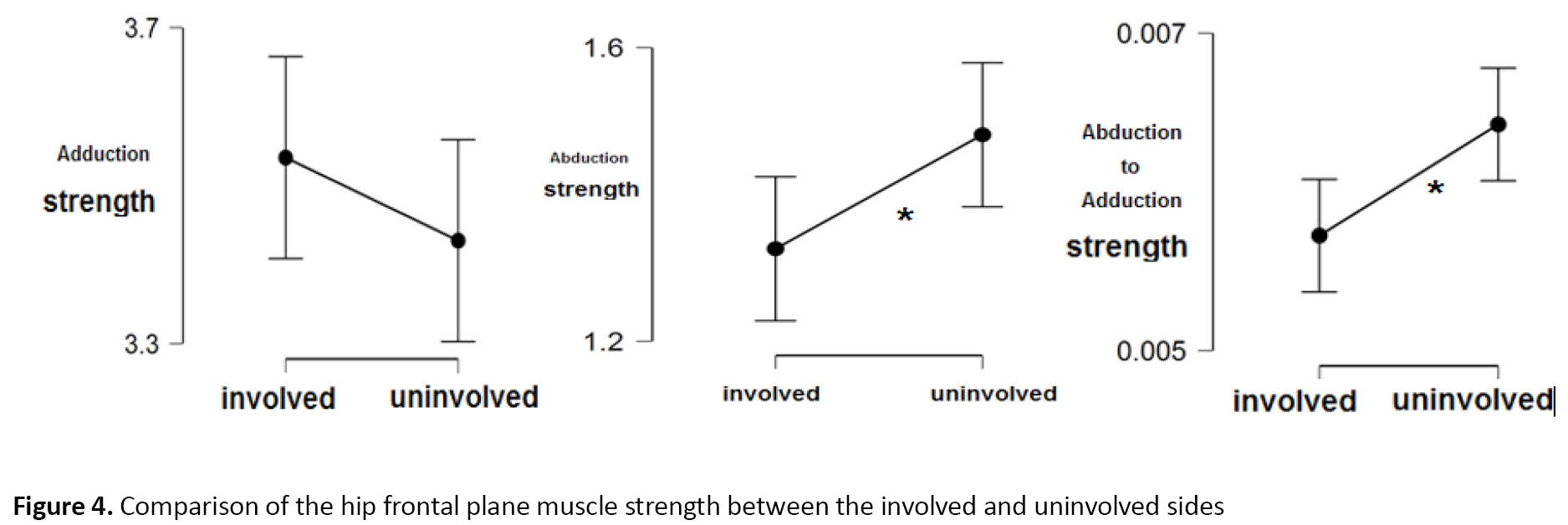
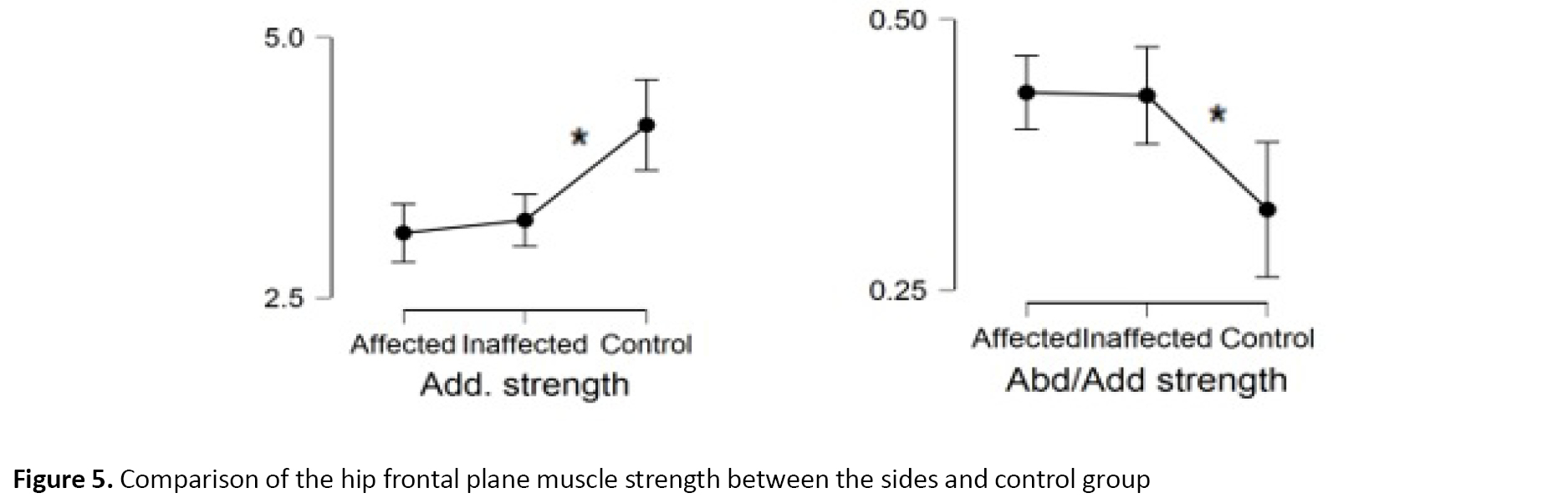
There was a significant difference between the involved and uninvolved sides in mean abduction and abduction to adduction ratio in the first and second trials (P=0.029, d=-0.368, 95%CI=-0.69, -0.03) (P=0.008, d=-0.459, 95%CI=-0.79, -0.12), showing a lower strength for the involved side (Table 3).
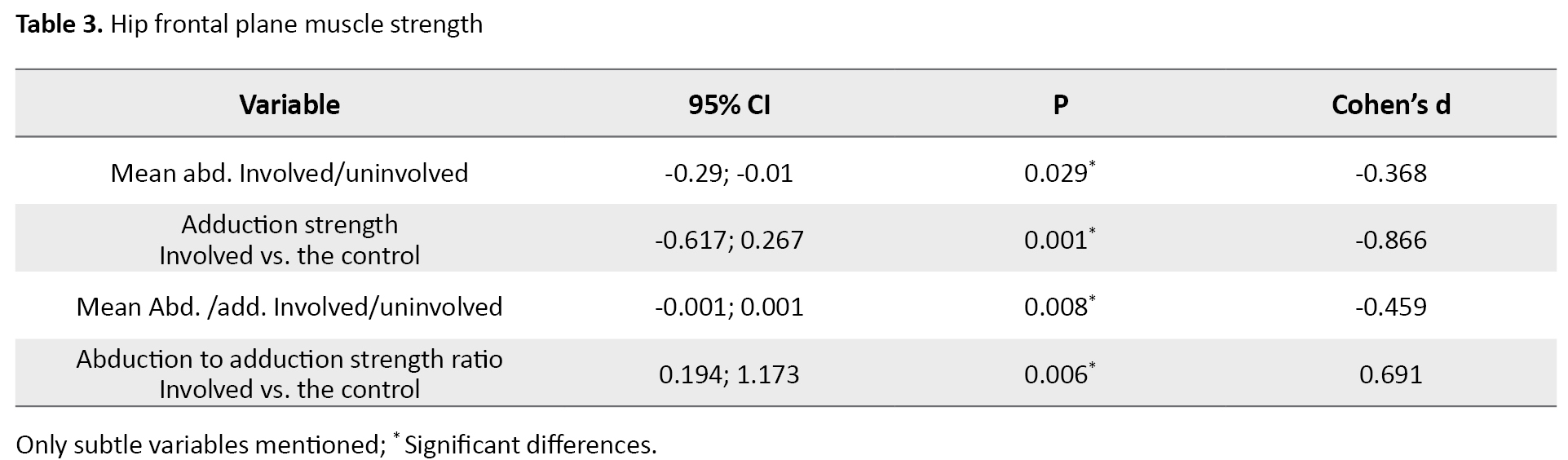
Adduction and abduction to adduction strength ratio were significantly different comparing both sides in the control group because the control group showed much greater adduction and lower abduction to adduction ratio (P<0.001, F=2.792, F=8.979) (Table 3). There was no significant difference between the sides in the first and second trials in the mean adduction strength (P=0.247, 95%CI= -0.13, 0.51) and no abduction strength differences were found between sides and the control group (P>0.005).
Furthermore, the closest variables to FIQ scores based on the correlation test were uninvolved adductor strength (r=0.367, r=0.332, P=0.024, P=0.042), followed by active and passive adduction ROM (r=-0.446, r=-0.359, P=0.003, P=0.027). The closest variables to NAS scores were active and passive adduction ROM (r=0.415, r=0.326, P=0.010, P=0.046). Finally, no correlations were found between flexibility and strength (P>0.005).
4. Discussion
Our results suggested that there are no differences in active and passive ROM between involved and uninvolved leg while comparing the sides to the control group showed lesser adductor muscle flexibility (less passive adduction ROM in the control group) and more active adduction ROM, showing possible more reciprocal inhibition in the control group and possible neuromuscular impairment in participants with unilateral PFA causing more adduction ROM, which may lead to inappropriate stresses on the patellofemoral joint. We should also mention that the uninvolved side hip active and passive adduction ROM was significantly correlated with function and pain. A recent study measuring length, using gravity and standard goniometry has compared Tensor Fasciae Latae / Iliotibial Band length in the frontal plane and reported that TFL/ITB length was not different between the PFA and control groups, while some have insisted on the role of ITB tightness [20, 29, 30]. Considering strength, the control group had stronger adductors with less adduction ROM and it seems that adductors are programmed to perform in a precise ROM with maximal efficacy producing maximal frontal plane stability by keeping the best force/length position of abductors. This makes the pelvis stable in the frontal plane, while on the involved side, muscular imbalance (weaker adductors and less active abductors), exceeded by more adduction ROM position following less reciprocal inhibition by abductors that may lead to more adduction position compared with the uninvolved side and control group during the stance phase of gait or running. It can biomechanically lead to knee excessive valgus motion and changes in patellofemoral joint stress resulting in PFA. This, in turn, may adversely position the gluteus medius in an improper force/length position. As we know, the gluteus medius has the most effective force/length position in 10 degrees of adduction, which leads to the production of less pelvis frontal plane stabilization [16]. All these may suggest that adductor muscle strength and adduction ROM may represent a firm muscle strength and ROM range, which will help abductor muscles to perform in the most efficient way providing stabilization to the pelvis and femur as it is demanded in high-intensity activities, such as running. Any variations in this situation may lead to changes in most efficient abductors’ torque/ROM proportion causing the following abductors and biomechanical changes, which may be associated with PFA. We should mention that all the interpretations comparing sides may be a delusion as pain can alter strength bilaterally but comparing with the control group gives us some firm approval.
According to the results, the most related variables to FIQ scores were adductor muscles strength of the uninvolved side and the control group with a positive correlation and active/passive hip adduction ROM of the uninvolved side with a negative correlation. The most related variables to NAS scores were active and passive hip adduction ROM of the uninvolved side with a positive correlation. It is really difficult to interpret these correlations, but one possible explanation is that we may have a precise abduction to adduction ROM and strength interaction, whereas changing this interaction will lead to muscular imbalance and biomechanical changes. Increasing or decreasing hip adduction strength will have an initial positive effect on the function with the probable explanation of preparing a more proper hip abduction torque/length position. However, excessive increase or decrease in hip adduction strength will adversely affect the functions. It will lead to biomechanical changes and an increase in patellofemoral joint stress and patellofemoral pain arthropathy as well as functional impairments. Therefore, the function can be linked to adductor muscle strength through this chain mechanism. Nevertheless, further prospective investigations may be required to confirm the theory. Based on our results, the uninvolved hip adduction ROM was negatively correlated with FIQ scores and positively with NAS scores; increase hip adduction motion will lead to enhanced knee valgus motion and increased patellofemoral stress and PFA. Therefore, an increase in hip adduction motion of the normal uninvolved side will lead to functional impairments (lower FIQ scores) and intensified pain (greater NAS scores). Our results seem to be consistent with two articles, which suggested that hip adduction ROM may be used as a predictor of pain and function in subjects with PFA [5, 6].
Based on the results, it can be concluded that in addition to abductor strength, it is important to consider abductor to adductor strength and flexibility interaction, because there is a reasonable relationship between the involved side hip abductor and adductor muscles compared with uninvolved side and control group mentioned in the discussion, suggesting muscular impaired interaction affecting unilateral PFA. Thus, in sprinter runners with unilateral PFA, not only abductor strength but also adductor strength and abduction to adduction ratio should be considered separately on both sides to reach a precise evaluation helping design a better physical therapy plan. We should mention that this study is a preliminary step to gather evidence about muscular impaired interaction, which may affect PFA; thus, further prospective studies using different tools and methods may be needed to confirm the role of impaired muscular interaction in sprinter runners with unilateral PFA.
Ethical Considerations
Compliance with ethical guidelines
The protocol was approved by Ethics Committee of Iran University of Medical Sciences (Code: 1397.435).
Funding
This study was founded by Iran University of Medical Sciences. The paper was extracted from the MSc. thesis of the first author at the Department of Physiotherapy, Faculty of Rehabilitation, Iran University of Medical Sciences.
Authors' contributions
Conceptualization, supervision: Soheil Mansour Sohani; Methodology: Ali Amiri; Experiment, writing – original draft: Pezhman Masoudi; Investigation, writing – review & editing, funding acquisition, resources: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
Patellofemoral Pain Syndrome (PFPS) is an overuse syndrome usually characterized by an aching pain in the peripatellar area. The terminology PFPS has been used as the preferred term in recent years; however, it does not consider how non-painful joint conditions could be a precursor to pain development, does not include symptoms, such as crepitus, and may increase a focus on the ‘pain’ aspect of the condition. The alternative term, Patellofemoral Arthropathy (PFA), was proposed, which indicates that PFP may be a symptom of joint disease [1]. Physical activities, such as climbing stairs, squatting, jumping, running, and two or four kneeling positions for prolonged periods of time will deteriorate PFP. PFA is the most common knee disorder in runners [2, 3]. PFA has been reported as the cause of 20% to 40% of all visits to physical therapy and sport medicine clinics as a result of knee pain. PFA symptoms can lead to impairments during sport and functional and daily life activities. Various factors can lead to the development of PFA symptoms, which makes the diagnosis of the cause of symptoms and designing a rehabilitation program extremely difficult [4].
One etiological theory to PFA is that poor proximal neuromuscular control and/or weakness of the hip musculature may lead to poor control of frontal and transverse plane motions of the hip [5]. For example, excessive hip adduction, hip internal rotation, and the following knee abduction have been hypothesized to increase patellofemoral joint stress and affect the patellofemoral joint biomechanics. Furthermore, during weight-bearing activities, this situation has been proposed to increase the dynamic quadriceps angle, which finally results in intensified patella-femoral joint stress [5, 6]. Some investigations have demonstrated that females and males with PFA display altered knee joint kinematics in comparison with non-involved control participants. Particularly, symptomatic PFA patients exhibit increased frontal plane knee joint motion and knee joint loading during dynamic activities, such as running [7, 8, 9].
Thus, hip abductors strengthening is often advocated to improve hip mechanics to reduce the incidence of or symptoms related to PFA [10]. In addition to these findings, one study suggested that strengthening alone may be insufficient to alter abnormal movement patterns of the lower extremities during running [11]. Despite large and significant gains in the strength of hip abductors and hip external rotators following exercise protocols, no changes have been seen in abnormal hip mechanics during running. Accordingly, as suggested later, possibly additional therapeutic programs may be required, such as myofascial release, stretching, or neuromuscular retraining for hip strengthening to finally better manage such a syndrome [11, 12].
Hip adduction Range of Motion (ROM) has been suggested to be a predictor of pain and function in both males and females with PFA. It has been proposed that frontal plane motions of the hip and knee can raise the dynamic quadriceps angle during functional tasks. It has been reported that a 10° increase in the quadriceps angle can elevate patellofemoral stress by 45% [5, 6]. Task-dependent excessive functional limb Varus during running has been suggested as a possible reason for adductor overactivity and stiffness and the following abductor reciprocal inhibition [13]. It has also been reported that abductor muscles with the greatest hip abduction torque at the hip positioned at 10° adduction, along with the hip position during single-leg stance, will help provide adequate stability to the pelvis [14].
Then, any changes in this position following changes or imbalances in adductor/adductor length or strength may contribute to PFA. Therefore, two questions may raise: Are there any muscular strength and flexibility changes in frontal plane hip muscles in runners with PFA? What is the relationship between flexibility and strength? Accordingly, the aim of this study was to compare abduction, adduction, and abduction to adduction flexibility and strength ratio to clarify the role of muscular strength, flexibility, and balance in sprinter runners with unilateral PFA.
2. Materials and Methods
Design
A total of 38 semiprofessional male sprinter runners declaring unilateral pain (3 or more on the numerical analog scale) or showing positive patellar grind test result on just one side were compared assigned to the legs and the control group (20 matched controls) regarding frontal plane muscle strength and flexibility in this case-control study. They were recruited using the non-probability sampling method from Tehran and Shiraz running clubs from April 2018 to January 2020.
Participants
The participants with PFA were excluded from the study if they had the following exclusion criteria: 1) a history of hip, knee, or ankle surgery over the past 3 years; 2) patellar dislocation; 3) any deviation in the lumbar vertebra; 4) systemic arthritis, knee ligament or meniscal injury; 5) plica syndrome, Sinding-Larsen-Johansson disease, Osgood-Schlatter disease; 6) any neurological disease [15]; and 7) bilateral PFA. Because no similar ROM studies had been performed on the frontal plane, we selected 10 pilot participants with NAS Activity Scale (NAS) peripatellar pain score of 3 or more or showing unilateral positive patellar grind test result. Following data analysis, we used a rule of thumb method to determine the sample size, which was determined to be 38 cases based on ROM data [16].
We also had to choose 20 of 26 cases for the control group and we evaluated and matched them with 20 PFA cases because of the prevalence of COVID-19 and no chances of more evaluation because of physical distancing rules. The qualifying participants were first informed about the study purpose and the study protocol. First, the participants were given a page consisting of the Numeric Pain Rating Scale (NPRS), where an 11-point scale ranging from 0 to 10 was anchored on the left with the phrase ‘‘no pain’’ and on the right with the phrase ‘‘worst imaginable pain.’’ Patients rated their pain within the last 24 hours. Numeric pain scales have been shown to be reliable and valid [17, 18]. They were then given the Persian version of the Functional Index Questionnaire (FIQ) for further investigation and possible correlations with functional impairment after the study. This questionnaire has been confirmed to be valid and reliable in Iran [19].
Procedure
To perform the study, we followed two different procedures; the participant’s flexibility was assessed first, and then, they were assessed with strength in two trials, with 5 minutes of resting period between the trials based on the average of two trials for comparison [20]. Hip adductor and abductor muscle flexibility were implied from hip adduction and abduction ROM indirectly. Both active and passive ROM was used for comparison. Because of using 2D motion analysis as the flexibility measurement, we marked a rectangle surface on the ground with the height of 2 m and the width of 1.5 m via indicator markers. Also, we marked 3 parts of participants’ leg and pelvis to measure the ROM: 1) right anterior superior iliac spine 2) left anterior superior iliac spine 3) a relative point to the femoral lateral epicondyle (3 cm upper and in the middle of thigh diameter up to patella bone). The subjects’ head was in the middle of the upper marked line and the camera tripod in the middle of the lower one. The angle of the camera was 20 degrees toward the surface in relation to the horizontal plane with the film recorded with consistent camera features getting ready to record and upload the video to software (Figure 1).
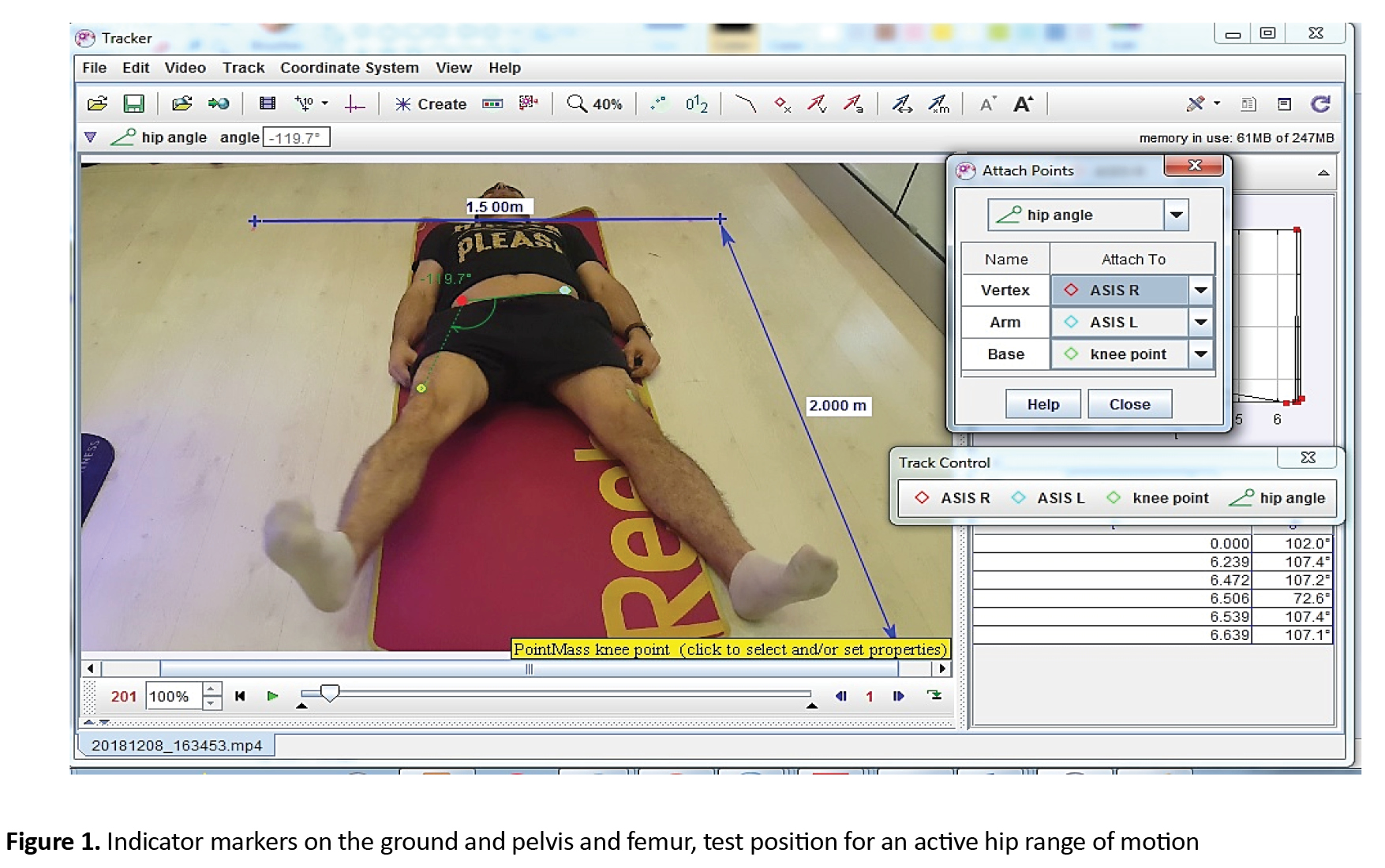
Once the filming project was done, we analyzed the films through 2D motion analysis software (Tracker 4.11 x Douglas Brown, Wolfgang Christian 2017). Cost-benefit and accessibility of 2D motion analysis have been already confirmed and it is a valid and reliable instrument in measuring joint ROM along with 3D motion analysis, which is too expensive and out of reach for sports studies, that are commonly performed outside the experimental parts [21, 22, 23, 24]. For analysis of the films, we chose 3 mass points and 1 protractor in the software environment. Then, we matched the marked points on the leg and pelvis to mass points in the software named R ASIS, L ASIS, and knee point and fixed them with vertex, arm, and base of the protractor to measure hip angles. Thereafter, we played the film and sought for ultimate pure hip adduction and abduction ROMs, free of additional rotational parts or pelvis movements. Next, we paused the film and noted the protractor’s number (in degrees) as hip ROM (Figure 1). All ROM data were normalized to the subject’s leg length to account for individual differences as we knew choosing mass points on the specific anatomical landmarks instead of the joint center may lead to adiposity influence on angles. Nevertheless, choosing a joint center will show variability in 2D motion analysis, as well [24].
The hip muscle strength was measured through a hand-held dynamometer (SF-500 push/pull force gauge; IMADA), which has been confirmed to be reliable when used by a single experienced tester [25, 26]. We measured force as opposed to torque as it is the standard measure commonly used in clinical practice. To accurately measure muscle force, we used a consistent and firm length strap at the end of the lower extremity preventing hip abduction identically for all participants and allowing abductors’ muscles to move in a more accurate kinesiology position according to their torque/hip angle curve as we knew measuring muscle strength at the end of abduction range will lead to muscle active insufficiency [14]. The participants were positioned on their sides and then asked to abduct their legs as far as the firm band allowed them. When the movement stopped, the dynamometer was placed on the lateral femoral epicondyle and they were asked to push as far as they could. Accordingly, the peak hip abduction isometric force (N) was measured. During the measurement, the dynamometer was placed between the legs on the medial femoral epicondyle with our hand and soft pad between the dynamometer and resting leg, and participants were asked to press toward the other leg as far as they could. The examiner did not try to overcome the subject’s effort (Figure 2).

These procedures were repeated two times with 5 minutes of resting based on the average for strength comparison. All strength data were normalized to body mass, which has been confirmed to be the best way to normalize strength in order to rule out any individual differences.
We used male samples only for two reasons: the first gender should be factored into analyses of allometric scaling as men have higher b-values than women for both force and torque [27]. Secondly, few studies have evaluated only a male sample.
Data analysis
We used the Kolmogorov-Smirnov test to check the differences in the baseline characteristics. The significance of the difference in abduction, adduction, and abduction to adduction ratio strength and flexibility between uninvolved and involved sides was determined using paired t-test and repeated measures ANOVA to compare with the control group. A correlation test was used to clarify the factors most relevant to dysfunction and pain, and also to distinguish any correlations between flexibility and strength. To determine the effect size, we used Cohen’s d, where a Cohen’s d 0/2 is a small effect, a Cohen’s d, 0.5 is a medium effect, and a 0.8 amount is considered a large effect [28]. The set of variables providing the best linear discrimination was selected. Statistical analyses were performed using SPSS v. 23 (SPSS Inc, Chicago, IL) and JASP 0.9.1 analysis software.
3. Results
According to data analysis, the participants’ Mean±SD age was 23.46±4.01 years, height was 1.78±0.05 m, weight was 71.3±9.21 kg, Body Mass Index (BMI) was 22.45±2.30 kg/m2, and their leg length was 90.23±4.21 cm. Weight, leg length, height, and BMI had normal distributions (P>0.05), but a significant difference was seen for age between participants (P=0.023) (Table 1).
No differences were found in the active or passive abduction and adduction ROM between either side (P>0.005) but passive abduction and active adduction ROM were significantly greater in the control group (P<0.001) (Tables 2, 3) (Figure 3, 4, 5).
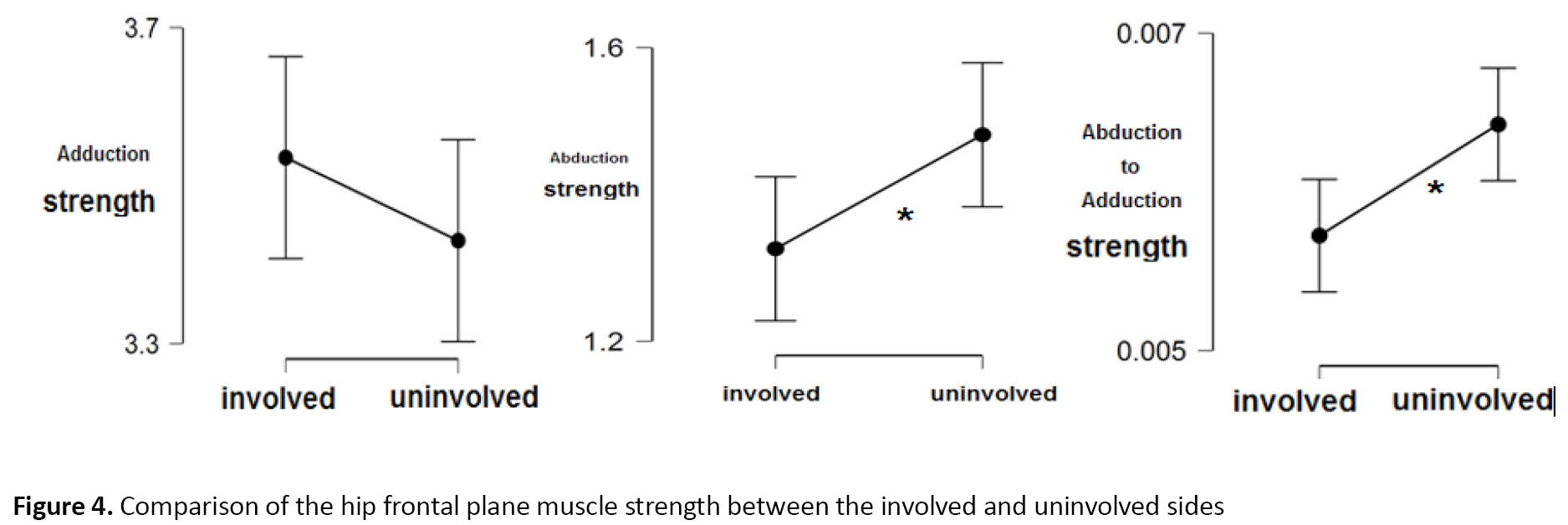
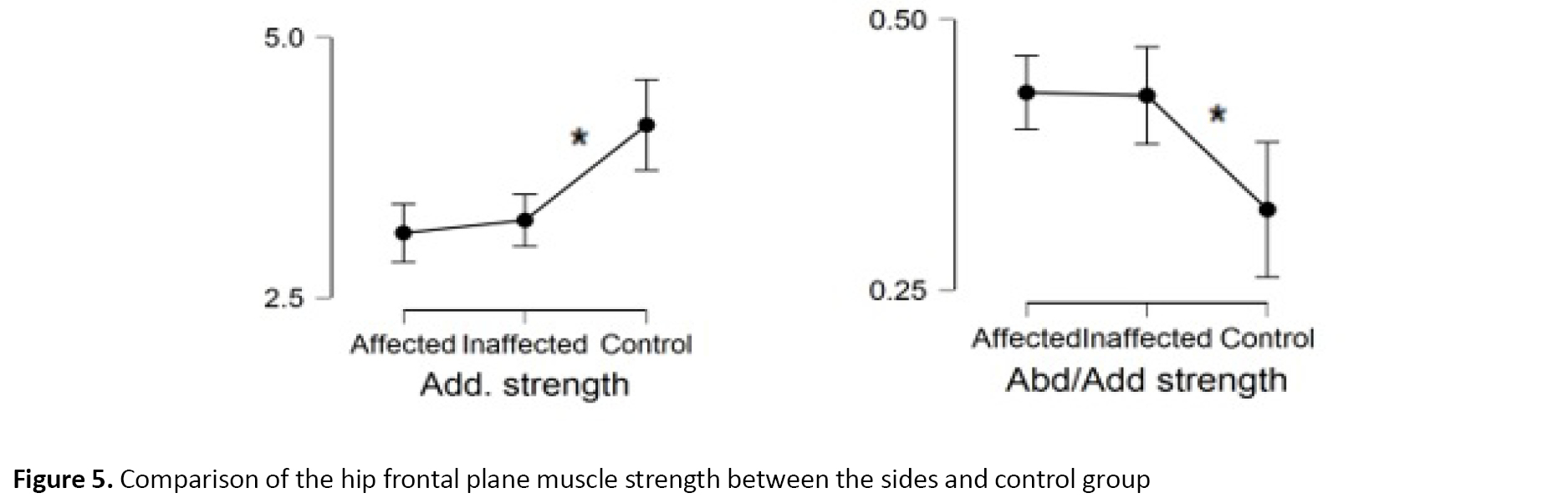
There was a significant difference between the involved and uninvolved sides in mean abduction and abduction to adduction ratio in the first and second trials (P=0.029, d=-0.368, 95%CI=-0.69, -0.03) (P=0.008, d=-0.459, 95%CI=-0.79, -0.12), showing a lower strength for the involved side (Table 3).
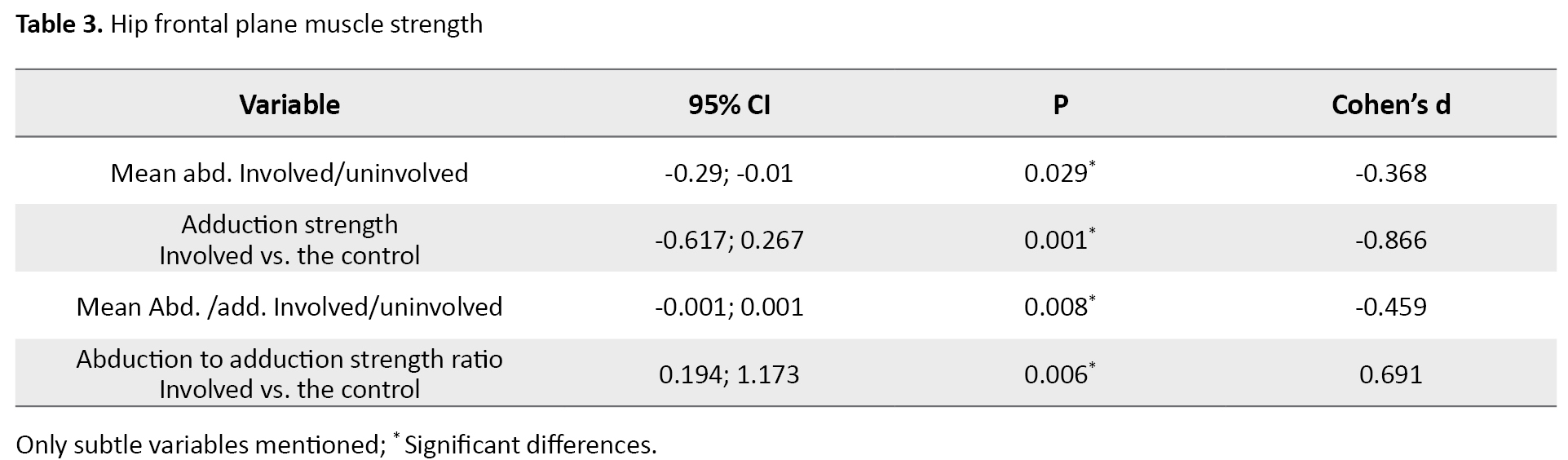
Adduction and abduction to adduction strength ratio were significantly different comparing both sides in the control group because the control group showed much greater adduction and lower abduction to adduction ratio (P<0.001, F=2.792, F=8.979) (Table 3). There was no significant difference between the sides in the first and second trials in the mean adduction strength (P=0.247, 95%CI= -0.13, 0.51) and no abduction strength differences were found between sides and the control group (P>0.005).
Furthermore, the closest variables to FIQ scores based on the correlation test were uninvolved adductor strength (r=0.367, r=0.332, P=0.024, P=0.042), followed by active and passive adduction ROM (r=-0.446, r=-0.359, P=0.003, P=0.027). The closest variables to NAS scores were active and passive adduction ROM (r=0.415, r=0.326, P=0.010, P=0.046). Finally, no correlations were found between flexibility and strength (P>0.005).
4. Discussion
Our results suggested that there are no differences in active and passive ROM between involved and uninvolved leg while comparing the sides to the control group showed lesser adductor muscle flexibility (less passive adduction ROM in the control group) and more active adduction ROM, showing possible more reciprocal inhibition in the control group and possible neuromuscular impairment in participants with unilateral PFA causing more adduction ROM, which may lead to inappropriate stresses on the patellofemoral joint. We should also mention that the uninvolved side hip active and passive adduction ROM was significantly correlated with function and pain. A recent study measuring length, using gravity and standard goniometry has compared Tensor Fasciae Latae / Iliotibial Band length in the frontal plane and reported that TFL/ITB length was not different between the PFA and control groups, while some have insisted on the role of ITB tightness [20, 29, 30]. Considering strength, the control group had stronger adductors with less adduction ROM and it seems that adductors are programmed to perform in a precise ROM with maximal efficacy producing maximal frontal plane stability by keeping the best force/length position of abductors. This makes the pelvis stable in the frontal plane, while on the involved side, muscular imbalance (weaker adductors and less active abductors), exceeded by more adduction ROM position following less reciprocal inhibition by abductors that may lead to more adduction position compared with the uninvolved side and control group during the stance phase of gait or running. It can biomechanically lead to knee excessive valgus motion and changes in patellofemoral joint stress resulting in PFA. This, in turn, may adversely position the gluteus medius in an improper force/length position. As we know, the gluteus medius has the most effective force/length position in 10 degrees of adduction, which leads to the production of less pelvis frontal plane stabilization [16]. All these may suggest that adductor muscle strength and adduction ROM may represent a firm muscle strength and ROM range, which will help abductor muscles to perform in the most efficient way providing stabilization to the pelvis and femur as it is demanded in high-intensity activities, such as running. Any variations in this situation may lead to changes in most efficient abductors’ torque/ROM proportion causing the following abductors and biomechanical changes, which may be associated with PFA. We should mention that all the interpretations comparing sides may be a delusion as pain can alter strength bilaterally but comparing with the control group gives us some firm approval.
According to the results, the most related variables to FIQ scores were adductor muscles strength of the uninvolved side and the control group with a positive correlation and active/passive hip adduction ROM of the uninvolved side with a negative correlation. The most related variables to NAS scores were active and passive hip adduction ROM of the uninvolved side with a positive correlation. It is really difficult to interpret these correlations, but one possible explanation is that we may have a precise abduction to adduction ROM and strength interaction, whereas changing this interaction will lead to muscular imbalance and biomechanical changes. Increasing or decreasing hip adduction strength will have an initial positive effect on the function with the probable explanation of preparing a more proper hip abduction torque/length position. However, excessive increase or decrease in hip adduction strength will adversely affect the functions. It will lead to biomechanical changes and an increase in patellofemoral joint stress and patellofemoral pain arthropathy as well as functional impairments. Therefore, the function can be linked to adductor muscle strength through this chain mechanism. Nevertheless, further prospective investigations may be required to confirm the theory. Based on our results, the uninvolved hip adduction ROM was negatively correlated with FIQ scores and positively with NAS scores; increase hip adduction motion will lead to enhanced knee valgus motion and increased patellofemoral stress and PFA. Therefore, an increase in hip adduction motion of the normal uninvolved side will lead to functional impairments (lower FIQ scores) and intensified pain (greater NAS scores). Our results seem to be consistent with two articles, which suggested that hip adduction ROM may be used as a predictor of pain and function in subjects with PFA [5, 6].
Based on the results, it can be concluded that in addition to abductor strength, it is important to consider abductor to adductor strength and flexibility interaction, because there is a reasonable relationship between the involved side hip abductor and adductor muscles compared with uninvolved side and control group mentioned in the discussion, suggesting muscular impaired interaction affecting unilateral PFA. Thus, in sprinter runners with unilateral PFA, not only abductor strength but also adductor strength and abduction to adduction ratio should be considered separately on both sides to reach a precise evaluation helping design a better physical therapy plan. We should mention that this study is a preliminary step to gather evidence about muscular impaired interaction, which may affect PFA; thus, further prospective studies using different tools and methods may be needed to confirm the role of impaired muscular interaction in sprinter runners with unilateral PFA.
Ethical Considerations
Compliance with ethical guidelines
The protocol was approved by Ethics Committee of Iran University of Medical Sciences (Code: 1397.435).
Funding
This study was founded by Iran University of Medical Sciences. The paper was extracted from the MSc. thesis of the first author at the Department of Physiotherapy, Faculty of Rehabilitation, Iran University of Medical Sciences.
Authors' contributions
Conceptualization, supervision: Soheil Mansour Sohani; Methodology: Ali Amiri; Experiment, writing – original draft: Pezhman Masoudi; Investigation, writing – review & editing, funding acquisition, resources: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
- Crossley KM, van Middelkoop M, Callaghan MJ, Collins NJ, Rathleff MS, Barton CJ. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 2: Recommended physical interventions (exercise, taping, bracing, foot orthoses and combined interventions). Br J Sports Med. 2016; 50(14):844-52. [DOI:10.1136/bjsports-2016-096268] [PMID] [PMCID]
- Devereaux MD, Lachmann SM. Patello-femoral arthralgia in athletes attending a Sports Injury Clinic. Br J Sports Med. 1984; 18(1):18-21. [DOI:10.1136/bjsm.18.1.18] [PMID] [PMCID]
- Earl JE, Hoch AZ. A proximal strengthening program improves pain, function, and biomechanics in women with patellofemoral pain syndrome. Am J Sports Med. 2011; 39(1):154-63. [DOI:10.1177/0363546510379967] [PMID]
- Blond L, Hansen L. Patellofemoral pain syndrome in athletes: a 5.7-year retrospective follow-up study of 250 athletes. Acta Orthop Belg. 1998; 64(4):393-400. https://www.researchgate.net/publication/262495851_Subjective_Sleep_Quality_in_Iranian_Patients_with_Spinal_Cord_Injury_Results_of_Pittsburgh_Sleep_Quality_Index_in_a_Referral_Center
- Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: A theoretical perspective. J Orthop Sports Phys Ther. 2003; 33(11):639-46. [DOI:10.2519/jospt.2003.33.11.639] [PMID]
- Powers CM. The influence of abnormal hip mechanics on knee injury: A biomechanical perspective. J Orthop Sports Phys Ther. 2010; 40(2):42-51. [DOI:10.2519/jospt.2010.3337] [PMID]
- Nakagawa TH, Serrão FV, Maciel CD, Powers CM. Hip and knee kinematics are associated with pain and self-reported functional status in males and females with patellofemoral pain. Int J Sports Med. 2013;34(11):997-1002. [DOI:10.1055/s-0033-1334966] [PMID]
- Willson JD, Davis IS. Utility of the frontal plane projection angle in females with patellofemoral pain. J Orthop Sports Phys Ther. 2008; 38(10):606-15. [DOI:10.2519/jospt.2008.2706] [PMID]
- Nakagawa TH, Moriya ÉT, Maciel CD, Serrão AF. Frontal plane biomechanics in males and females with and without patellofemoral pain. Med Sci Sports Exerc. 2012; 44(9):1747-55. [DOI:10.1249/MSS.0b013e318256903a] [PMID]
- Myer GD, Chu DA, Brent JL, Hewett TE. Trunk and hip control neuromuscular training for the prevention of knee joint injury. Clin Sports Med. 2008; 27(3):425-48. [DOI:10.1016/j.csm.2008.02.006] [PMID] [PMCID]
- Willy RW, Davis IS. The effect of a hip-strengthening program on mechanics during running and during a single-leg squat. J Orthop Sports Phys Ther. 2011; 41(9):625-32. [DOI:10.2519/jospt.2011.3470] [PMID]
- Mullaney MJ, Fukunaga T. Current concepts and treatment of patellofemoral compressive issues.Int J Sports Phys Ther. 2016; 11(6):891-902. [PMID]
- Magee DJ, Zachazewski JE, Quillen WS, Manske RC. Athletic and Sport Issues in Musculoskeletal Rehabilitation-E-Book. Amesterdam: Elsevier Health Sciences; 2010. https://books.google.nl/books?hl=en&lr=&id=3qF8q8VLWF8C&oi=fnd&pg=PP1&dq
- Neumann DA. Kinesiology of the hip: A focus on muscular actions. J Orthop Sports Phys Ther. 2010; 40(2):82-94. [DOI:10.2519/jospt.2010.3025] [PMID]
- Thomeé R, Augustsson J, Karlsson J. Patellofemoral pain syndrome: A review of current issues. Sports Med. 1999; 28(4):245-62. [DOI:10.2165/00007256-199928040-00003] [PMID]
- Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharm Stat. 2005; 4(4):287-91. [DOI:10.1002/pst.185]
- Katz J, Melzack R. Measurement of pain. Surg Clin North Am. 1999; 79(2):231-52. [DOI:10.1016/S0039-6109(05)70381-9]
- Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain. 1994; 58(3):387-92. [DOI:10.1016/0304-3959(94)90133-3]
- Negahban H, Pouretezad M, Sohani SM, Mazaheri M, Salavati M, Mohammadi F. Validation of the Persian version of Functional Index Questionnaire (FIQ) and Modified FIQ in patients with patellofemoral pain syndrome. Physiother Theory Pract. 2013; 29(7):521-30. [DOI:10.3109/09593985.2012.761308] [PMID]
- Piva SR, Goodnite EA, Childs JD. Strength around the hip and flexibility of soft tissues in individuals with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2005; 35(12):793-801. [DOI:10.2519/jospt.2005.35.12.793] [PMID]
- Hewett TE, Myer GD, Ford KR, Heidt RS Jr, Colosimo AJ, McLean SG, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am J Sports. 2005; 33(4):492-501. [DOI:10.1177/0363546504269591] [PMID]
- McLean SG, Walker K, Ford KR, Myer GD, Hewett TE, van den Bogert AJ. Evaluation of a two dimensional analysis method as a screening and evaluation tool for anterior cruciate ligament injury. Br J Sports Med. 2005; 39(6):355-62. [DOI:10.1136/bjsm.2005.018598] [PMID] [PMCID]
- Yazdifar M, Yazdifar MR, Mahmud J, Esat I, Chizari M. Evaluating the hip range of motion using the goniometer and video tracking methods. Procedia Eng. 2013; 68:77-82. [DOI:10.1016/j.proeng.2013.12.150]
- Holden S, Boreham C, Doherty C, Delahunt E. Two-dimensional knee valgus displacement as a predictor of patellofemoral pain in adolescent females. Scand J Med Sci Sports. 2017; 27(2):188-94. [DOI:10.1111/sms.12633] [PMID]
- Bohannon RW. Test-retest reliability of hand-held dynamometry during a single session of strength assessment. Phys Ther. 1986; 66(2):206-9. [DOI:10.1093/ptj/66.2.206]
- Thorborg K, Petersen J, Magnusson SP, Hölmich P. Clinical assessment of hip strength using a hand-held dynamometer is reliable. Scand J Med Sci Sports. 2010; 20(3):493-501. [DOI:10.1111/j.1600-0838.2009.00958.x] [PMID]
- Bazett-Jones DM, Cobb SC, Joshi MN, Cashin SE, Earl JE. Normalizing hip muscle strength: establishing body-size-independent measurements. Arch Phys Med Rehabil. 2011; 92(1):76-82. [DOI:10.1016/j.apmr.2010.08.020] [PMID]
- Rice ME, Harris GT. Comparing effect sizes in follow-up studies: ROC Area, Cohen’s d, and r. Law Hum Behav. 2005; 29(5):615-20. [DOI:10.1007/s10979-005-6832-7] [PMID]
- Smith AD, Stroud L, McQueen C. Flexibility and anterior knee pain in adolescent elite figure skaters. J Pediatr Orthop. 1991; 11(1):77-82. [DOI:10.1097/01241398-199101000-00015] [PMID]
- Hudson Z, Darthuy E. Iliotibial band tightness and patellofemoral pain syndrome: A case-control study. Man Ther. 2009; 14(2):147-51. [DOI:10.1016/j.math.2007.12.009]
Type of Study: Research |
Subject:
Physiotherapy
Received: 2020/10/16 | Accepted: 2020/12/1 | Published: 2020/12/30
Received: 2020/10/16 | Accepted: 2020/12/1 | Published: 2020/12/30