Volume 3, Issue 1 (Continuously Updated 2020)
Func Disabil J 2020, 3(1): 131-140 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hassani Z, Mokhtarinia H R, Gabel C P. Rehabilitation Interventions for Gait Problems in Patients With Diabetic Peripheral Neuropathy: A Scoping Review. Func Disabil J 2020; 3 (1) :131-140
URL: http://fdj.iums.ac.ir/article-1-140-en.html
URL: http://fdj.iums.ac.ir/article-1-140-en.html
1- Department of Occupational Therapy, Semnan University of Medical Science, Semnan, Iran.
2- Department of Ergonomics, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,hrmokhtarinia@yahoo.com
3- Independent Research, Access Physiotherpay Coolum Beach Qld Australia.
2- Department of Ergonomics, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
3- Independent Research, Access Physiotherpay Coolum Beach Qld Australia.
Full-Text [PDF 1065 kb]
(611 Downloads)
| Abstract (HTML) (1713 Views)
Full-Text: (956 Views)
1. Introduction
Diabetic peripheral neuropathy (DPN) is considered as one of the associated complications of type 2 diabetes mellitus and has rapidly increased in developing countries [1, 2]. Its prevalence ranged from 13% to 68% in the diabetic population, in 2009 [3]. Some patients experience painful symptoms, while others may be asymptomatic [1]. The DPN affects the lower extremities (motor, sensory, and autonomic) nerves to variable degrees and it progresses gradually and symmetrically from distal to proximal [4,5,6]. The complications of DPN include the loss of vibration sense, reduced tactile sensitivity, proprioception deficiency, decreased muscle strength, and changes in balance and gait patterns [4,5,6,7].
Gait and balance disturbances are challenging conditions in the diabetic patient as they result in reduced performance. Previous research has reported changes in gait parameters, such as speed, step length, the number of steps per minute, articular position, and ground reaction forces in DPN patients, compared with healthy individuals [4,5,6,7,8]. As a result of these changes, patients adopt less demanding functional gait variations. In a closed-loop chain, less activity results in a reduced Range Of Motion (ROM), reduced muscle strength, and the deterioration of the gait biomechanics and balance [9, 10]. A consequence is the gradual adoption of a hip prominent strategy because of reduced ankle plantar flexor strength, which is known as a “slowness strategy” [11, 12].
The management of the diabetic patients’ symptoms follows various recommendations as presented within public health guidelines [13]. One of these is an exercise program involving a minimum of 30 minutes per day, six times per week, to maintain gait security and balance [13]. Additionally, some evidence indicates that both physiotherapy and exercise therapy positively affect muscle strength, proprioception improvement, and balance and gait recovery in peripheral neuropathy patients, including those with type 2 diabetes [14, 15]. A further consideration is the psychological and cognitive-behavioral factors involved in the management of diabetic patients, particularly those with gait alternations. Intervention provided by the therapists should encourage a reduction in fall risk and include treatment plans that consequently improve the performance and safety of patients’ gait. This will increase patients’ self-confidence to an acceptable level, where they can perform these gait patterns as an integral part of the activity of daily living [16]. The overall literary consensus is that rehabilitation interventions effectively improve gait performance in diabetic neuropathy patients [17, 18].
Scoping review is an increasingly recognized literature review methodology, especially in health-care studies. According to Mays et al. (2001), scoping studies allow a specific line of research to propose rapidly and strongly the key concepts underpinning a line of research for relevant literature, with broad questions that enable the findings to be summarized, and subsequently provide the existing knowledge gaps for future research [19, 20]. Later, in 2005, Arksey and O’Malley [19] developed a methodological framework that expanded the Mays et al. (2001) definition [20].
This study aimed to use such a scoping review to highlight the current knowledge gaps in the rehabilitation interventions for the gait problems of patients with DPN.
Evidence acquisition: This scoping review followed a recognized methodological framework [19] that includes five stages: 1. Identifying the research questions; 2. Identifying relevant studies; 3. Study selection; 4. Charting the data; and 5. Collating, summarizing, and reporting the results. Ethics committee approval is not required for the scoping review studies.
Identifying the research questions
To answer the research objective, the authors framed the research questions according to the PICO (T) elements of patient, intervention, outcome, comparison, and time. The PICO (T) approach is an evidence-based model that includes a process of creating a question, identifying its location, evaluating, and repeating as needed [21]. We identified the research question as “What are the effective rehabilitation interventions that improve the functional gait of patients with diabetic neuropathy?” Also, the study objectives were as follows:
● To identify existing rehabilitation interventions for DPN patients with gait problems,
● To identify the literature gaps in gait and balance rehabilitation especially for patients with diabetics neuropathy,
● And to illustrate an evidence map and provide an evidence database on the scoping review results.
Identifying relevant studies
We conducted a preliminary search in PubMed, ScienceDirect, OTseeker, the Cochrane library, and Google Scholar search engine. The Medical Subject Heading terms and keywords included “diabetic neuropathy” AND “rehabilitation” AND/OR “gait” OR “posture” OR “stability” OR “lower limb” OR “interventions” OR “physical therapy” OR “occupational therapy”. The search period was from 2001 till May 2020. We also searched each reference list from the relevant articles to identify any related articles, including potential grey literature.
Study selection (screening)
Two experts reviewed the results and screened them based on the following inclusion/exclusion criteria. The inclusion criteria for the title were the subject’s diagnosis with DPN and gait problems, with or without the implementation of rehabilitation interventions. Besides, the exclusion criteria were non-English articles, the unavailability of full text, and ineffective interventions. Then, the reviewers screened the relevancy of the selected papers.
Charting the data
“Charting” is the process of charting the key topics of information from the primary studies included in the final analysis. Charting results in a frame or picture of thems that are derived from the literature [19]. A copy of the defined articles was provided to the same two reviewers; they separately reviewed the articles and charted the data. The research team conducted the data abstraction for all articles and sorted the obtained data into four broad elements or themes (in a paired approach of two reviewers per article, with a decision provided by a third reviewer in case of a split decision). Preliminary data abstraction elements were as follows:
● Subject characteristics (the type of diabetes, age, and gender),
● Type of rehabilitation intervention (physical therapy, occupational therapy, etc),
● Timing of interventions,
● And the type of outcomes (e.g., physical, mental, functional, etc).
Collating, summarizing, and reporting the data
Considering the aims of a scoping review to overview and present a large amount of data with high attention in summarized format [19], we used maps and tables to summarize the results.
2. Results
Out of 87 papers identified in our search (electronic and hand-search), nine studies had met the inclusion criteria and were entered in this review (Figure 1).
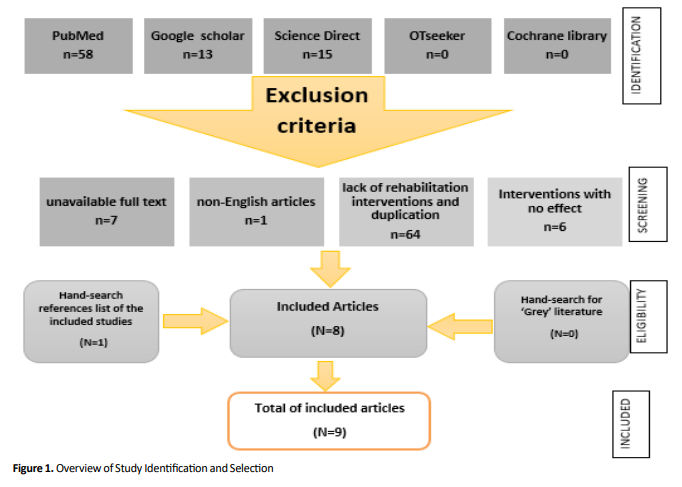
Table 1 summarizes the characteristics of the included studies. The selected studies were conducted across eight countries and published between 2001 and 2020.

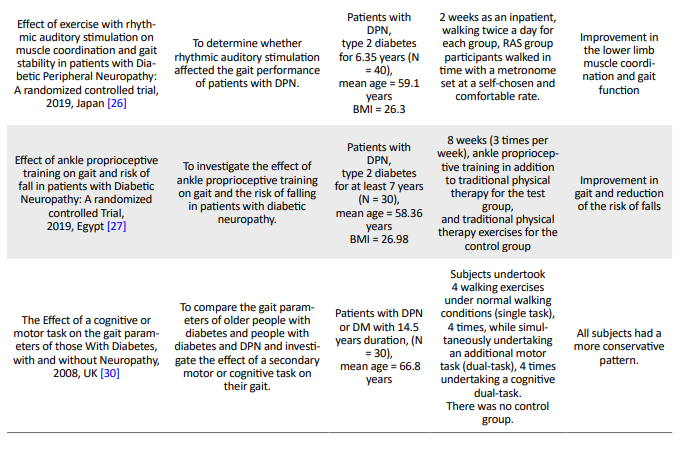
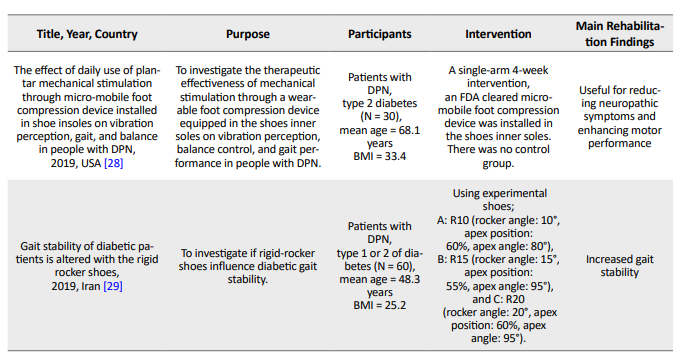
Six randomized control trials met our inclusion criteria [22-27]. Four studies examined patients with diabetes type 2 [24, 26-28], and three studies included both diabetes types 1 and 2 [23, 25, 29]. Also, the duration of the interventions ranged from 2 to 12 weeks. All studies examined a rehabilitation intervention, however, no comparative reports were presented about the two different rehabilitation interventions in patients. Paul et al. evaluated the effect of a cognitive-motor task on the gait variables of healthy and neuropathic subjects [30]. However, the studies significantly differed in terms of the intervention components, the difficulty of the rehabilitation program, the types of treatment providers, and the amount of details noticed in the study. Table 2 provides the results of the intervention components used in each study.
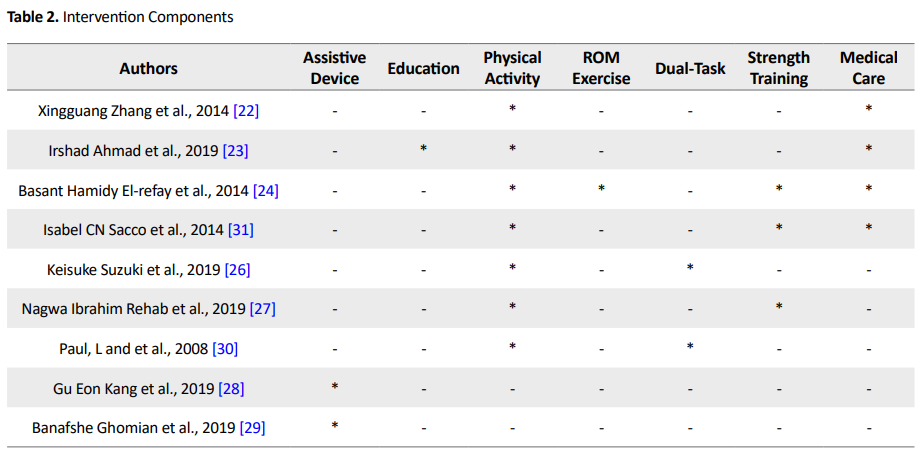
The frequent components of the rehabilitation interventions included exercise therapy and physical activity (n = 5) [22-25, 27], dual-task intervention (n = 2) [26, 30], and the use of assistive devices (n = 2) [28, 29]. A randomized control trial did not provide any information about the intervention providers [22]. In the remaining studies, the rehabilitation services were provided by physical therapists (n = 5), nurses (n = 1), a biomedical engineer (n = 1), and orthotics and prosthetics specialists (n = 1). Variable rehabilitation outcomes were obtained during the studies. The most frequently utilized outcomes included the assessment of changes in balance and stability [22, 30]; muscle strength [22]; proprioception [23]; function [23, 25-27]; gait parameters, such as speed, cadence, step time, and ankle joint ROM [24]; lower limb muscle coordination [26]; falls risk reduction [27]; conservative gait pattern [30]; and neuropathic symptoms [28].
3. Discussion
This study was conducted to present the rehabilitation interventions for gait problems in patients with DPN. The included studies considerably differed in terms of the measured indices, sample size, the method of implementation, etc. The studies provided preliminary support that rehabilitation interventions can improve gait parameters, balance, and function in people with DPN. The results of this scoping review fill an existing knowledge gap and provide findings for researchers, clinicians, and knowledge users concerned with diabetic rehabilitation. This scoping review also identified evidence on diabetic gait rehabilitation, however, related published studies were scarce in this regard. The reviewed studies presented different and scattered reports of rehabilitation interventions. Most of the research in rehabilitation programs was based on exercise therapy and physical activity; none considered the psychological and psychosocial aspects. Furthermore, the effectiveness of rehabilitation interventions on the activity of daily living was not investigated.
Over one-third of the papers discussed Impaired balance and decreased muscle strength as common problems in patients with diabetic neuropathy [4]. The majority of the included studies investigated the effect of interventions and gait training in chronic diabetic participants [2] and demonstrated positive findings. The results of this review also demonstrated that rehabilitation interventions play an effective role in improving balance and proprioception, increasing the coordination of the lower limb muscles, and improving muscle strength. These findings are consistent with the results of a previous study that reviewed rehabilitation interventions [32].
Moreover, diabetic ulcers in diabetic patients are a determinant factor in their gait disorders and must be considered in the management and prevention programs. The changes in plantar pressure distribution increase ulcer formation [33], however, this was only mentioned in two studies [22, 25]. Interestingly, a few interventions were performed by healthcare providers separately from the rehabilitation specialists, including nurses and biomedical engineers [28, 30].
Due to the variable characters of DPN patients and the negative effects gait can cause, rehabilitation specialists and researchers should consider several combined multidisciplinary aspects of interventions to attain the desired outcomes based on each patient’s profile. Every person with DPN and their health providers have their own set of needs, concerns, and preferences for managing their gait problems. Also, the personal and environmental factors should be considered during treatment decision-making [14].
To facilitate the descriptive comparisons between the studies with different designs, most of the interventions in this study were extracted from pre-post intervention studies and unique studies with specific outcome measurements. With this procedure, the results are at render of overestimating the effect of the intervention and bias; this can be considered as the weakness of this study. Consequently, these interventions must be interpreted cautiously. Furthermore, the majority of the included studies had relatively small sample sizes (N<40), which may have limited the power of their analysis and findings.
Strengths and limitations of this study
To the best of our knowledge, this is the first scoping review that identifies and summarizes the available literature on rehabilitation and intervention characteristics for gait problems in patients with DPN.
Despite intending to do a comprehensive search and finding grey literature sources, there is the possibility of missing some related studies. We did our best to consider the most important results in the literature. However, due to the limited word number, it was impossible to provide a detailed discussion considering all aspects of rehabilitation interventions effects, such as participation, objective, benefits, user satisfaction, and barriers to adoption and use. This review excluded non-English studies that may lead to incomplete data composition.
Implications for future research
Our review did not find any evidence on the best rehabilitation practice for DPN patients with gait abnormalities. Based on this scoping review, the priorities and inquiries for future research should be considered as follows:
● Evaluating rehabilitation interventions for DPN patients with gait problems in all countries;
● Identifying the limitations and barriers in performing rehabilitation interventions for DPN patients;
● Performing a systematic review of rehabilitation interventions for patients with DPN and gait problems;
● And the investigation of rehabilitation interventions that aim to resolve activity restriction and participation barriers, not only impairments, in this population.
Additionally, larger sample sizes and detailed methods are required for evaluating the effectiveness of rehabilitation interventions in DPN to further strengthen the findings for or against the various modalities adoption and utilization for gait rehabilitation. Unfortunately, it is unclear whether these types of rehabilitation interventions would be applied, effective, or cost-effective in different settings (e.g. inpatient, outpatient, community, or home). These are also important questions to be explored in future studies.
4. Conclusion
A variety of studies with different rehabilitation interventions and outcome measurements have been conducted on gait abnormalities in DPN patients. The effectiveness of these rehabilitation programs in the improvement of gait abnormalities is sparse and inconclusive. It appears that more trials with appropriate control and detailed descriptions of rehabilitation interventions are needed to determine the most relevant interventions for this patient group.
Ethical Considerations
Compliance with ethical guidelines
This is an scoping review and for such manuscript there is no need to Ethical code.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization, supervision: Hamidreza Mokhtarinia, Charl Philip Gabel; Methodology: Chals Philip Gabel; Investigation, writing – review & editing: All authors; Writing – original draft: Zahra Hasani.
Conflict of interest
The authors declare no competing interests.
References
Diabetic peripheral neuropathy (DPN) is considered as one of the associated complications of type 2 diabetes mellitus and has rapidly increased in developing countries [1, 2]. Its prevalence ranged from 13% to 68% in the diabetic population, in 2009 [3]. Some patients experience painful symptoms, while others may be asymptomatic [1]. The DPN affects the lower extremities (motor, sensory, and autonomic) nerves to variable degrees and it progresses gradually and symmetrically from distal to proximal [4,5,6]. The complications of DPN include the loss of vibration sense, reduced tactile sensitivity, proprioception deficiency, decreased muscle strength, and changes in balance and gait patterns [4,5,6,7].
Gait and balance disturbances are challenging conditions in the diabetic patient as they result in reduced performance. Previous research has reported changes in gait parameters, such as speed, step length, the number of steps per minute, articular position, and ground reaction forces in DPN patients, compared with healthy individuals [4,5,6,7,8]. As a result of these changes, patients adopt less demanding functional gait variations. In a closed-loop chain, less activity results in a reduced Range Of Motion (ROM), reduced muscle strength, and the deterioration of the gait biomechanics and balance [9, 10]. A consequence is the gradual adoption of a hip prominent strategy because of reduced ankle plantar flexor strength, which is known as a “slowness strategy” [11, 12].
The management of the diabetic patients’ symptoms follows various recommendations as presented within public health guidelines [13]. One of these is an exercise program involving a minimum of 30 minutes per day, six times per week, to maintain gait security and balance [13]. Additionally, some evidence indicates that both physiotherapy and exercise therapy positively affect muscle strength, proprioception improvement, and balance and gait recovery in peripheral neuropathy patients, including those with type 2 diabetes [14, 15]. A further consideration is the psychological and cognitive-behavioral factors involved in the management of diabetic patients, particularly those with gait alternations. Intervention provided by the therapists should encourage a reduction in fall risk and include treatment plans that consequently improve the performance and safety of patients’ gait. This will increase patients’ self-confidence to an acceptable level, where they can perform these gait patterns as an integral part of the activity of daily living [16]. The overall literary consensus is that rehabilitation interventions effectively improve gait performance in diabetic neuropathy patients [17, 18].
Scoping review is an increasingly recognized literature review methodology, especially in health-care studies. According to Mays et al. (2001), scoping studies allow a specific line of research to propose rapidly and strongly the key concepts underpinning a line of research for relevant literature, with broad questions that enable the findings to be summarized, and subsequently provide the existing knowledge gaps for future research [19, 20]. Later, in 2005, Arksey and O’Malley [19] developed a methodological framework that expanded the Mays et al. (2001) definition [20].
This study aimed to use such a scoping review to highlight the current knowledge gaps in the rehabilitation interventions for the gait problems of patients with DPN.
Evidence acquisition: This scoping review followed a recognized methodological framework [19] that includes five stages: 1. Identifying the research questions; 2. Identifying relevant studies; 3. Study selection; 4. Charting the data; and 5. Collating, summarizing, and reporting the results. Ethics committee approval is not required for the scoping review studies.
Identifying the research questions
To answer the research objective, the authors framed the research questions according to the PICO (T) elements of patient, intervention, outcome, comparison, and time. The PICO (T) approach is an evidence-based model that includes a process of creating a question, identifying its location, evaluating, and repeating as needed [21]. We identified the research question as “What are the effective rehabilitation interventions that improve the functional gait of patients with diabetic neuropathy?” Also, the study objectives were as follows:
● To identify existing rehabilitation interventions for DPN patients with gait problems,
● To identify the literature gaps in gait and balance rehabilitation especially for patients with diabetics neuropathy,
● And to illustrate an evidence map and provide an evidence database on the scoping review results.
Identifying relevant studies
We conducted a preliminary search in PubMed, ScienceDirect, OTseeker, the Cochrane library, and Google Scholar search engine. The Medical Subject Heading terms and keywords included “diabetic neuropathy” AND “rehabilitation” AND/OR “gait” OR “posture” OR “stability” OR “lower limb” OR “interventions” OR “physical therapy” OR “occupational therapy”. The search period was from 2001 till May 2020. We also searched each reference list from the relevant articles to identify any related articles, including potential grey literature.
Study selection (screening)
Two experts reviewed the results and screened them based on the following inclusion/exclusion criteria. The inclusion criteria for the title were the subject’s diagnosis with DPN and gait problems, with or without the implementation of rehabilitation interventions. Besides, the exclusion criteria were non-English articles, the unavailability of full text, and ineffective interventions. Then, the reviewers screened the relevancy of the selected papers.
Charting the data
“Charting” is the process of charting the key topics of information from the primary studies included in the final analysis. Charting results in a frame or picture of thems that are derived from the literature [19]. A copy of the defined articles was provided to the same two reviewers; they separately reviewed the articles and charted the data. The research team conducted the data abstraction for all articles and sorted the obtained data into four broad elements or themes (in a paired approach of two reviewers per article, with a decision provided by a third reviewer in case of a split decision). Preliminary data abstraction elements were as follows:
● Subject characteristics (the type of diabetes, age, and gender),
● Type of rehabilitation intervention (physical therapy, occupational therapy, etc),
● Timing of interventions,
● And the type of outcomes (e.g., physical, mental, functional, etc).
Collating, summarizing, and reporting the data
Considering the aims of a scoping review to overview and present a large amount of data with high attention in summarized format [19], we used maps and tables to summarize the results.
2. Results
Out of 87 papers identified in our search (electronic and hand-search), nine studies had met the inclusion criteria and were entered in this review (Figure 1).
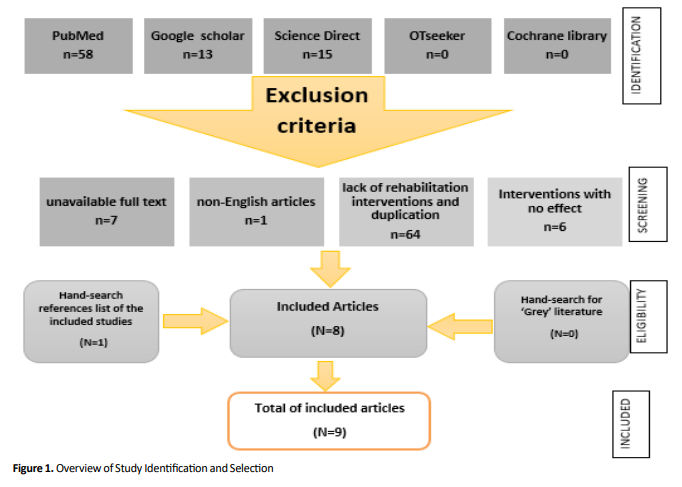
Table 1 summarizes the characteristics of the included studies. The selected studies were conducted across eight countries and published between 2001 and 2020.

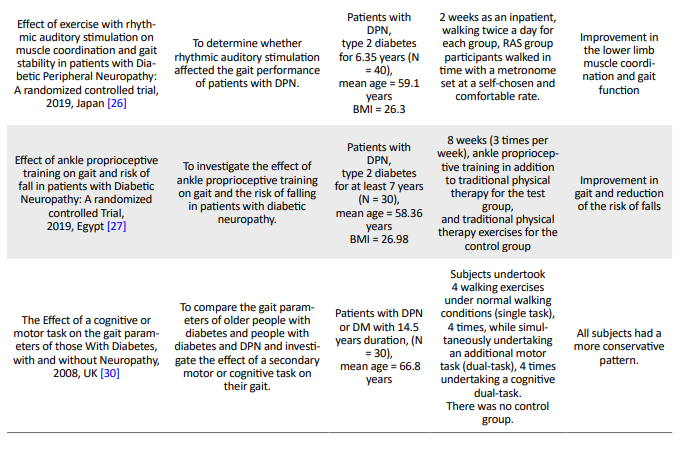
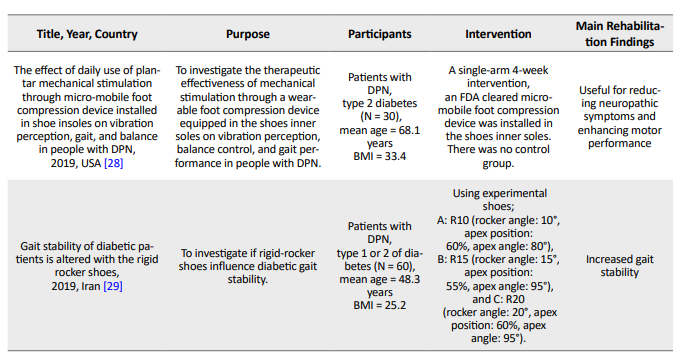
Six randomized control trials met our inclusion criteria [22-27]. Four studies examined patients with diabetes type 2 [24, 26-28], and three studies included both diabetes types 1 and 2 [23, 25, 29]. Also, the duration of the interventions ranged from 2 to 12 weeks. All studies examined a rehabilitation intervention, however, no comparative reports were presented about the two different rehabilitation interventions in patients. Paul et al. evaluated the effect of a cognitive-motor task on the gait variables of healthy and neuropathic subjects [30]. However, the studies significantly differed in terms of the intervention components, the difficulty of the rehabilitation program, the types of treatment providers, and the amount of details noticed in the study. Table 2 provides the results of the intervention components used in each study.
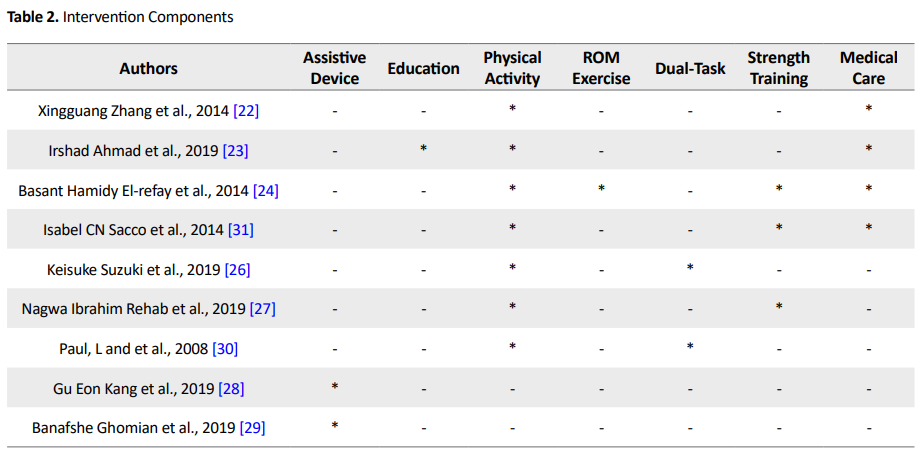
The frequent components of the rehabilitation interventions included exercise therapy and physical activity (n = 5) [22-25, 27], dual-task intervention (n = 2) [26, 30], and the use of assistive devices (n = 2) [28, 29]. A randomized control trial did not provide any information about the intervention providers [22]. In the remaining studies, the rehabilitation services were provided by physical therapists (n = 5), nurses (n = 1), a biomedical engineer (n = 1), and orthotics and prosthetics specialists (n = 1). Variable rehabilitation outcomes were obtained during the studies. The most frequently utilized outcomes included the assessment of changes in balance and stability [22, 30]; muscle strength [22]; proprioception [23]; function [23, 25-27]; gait parameters, such as speed, cadence, step time, and ankle joint ROM [24]; lower limb muscle coordination [26]; falls risk reduction [27]; conservative gait pattern [30]; and neuropathic symptoms [28].
3. Discussion
This study was conducted to present the rehabilitation interventions for gait problems in patients with DPN. The included studies considerably differed in terms of the measured indices, sample size, the method of implementation, etc. The studies provided preliminary support that rehabilitation interventions can improve gait parameters, balance, and function in people with DPN. The results of this scoping review fill an existing knowledge gap and provide findings for researchers, clinicians, and knowledge users concerned with diabetic rehabilitation. This scoping review also identified evidence on diabetic gait rehabilitation, however, related published studies were scarce in this regard. The reviewed studies presented different and scattered reports of rehabilitation interventions. Most of the research in rehabilitation programs was based on exercise therapy and physical activity; none considered the psychological and psychosocial aspects. Furthermore, the effectiveness of rehabilitation interventions on the activity of daily living was not investigated.
Over one-third of the papers discussed Impaired balance and decreased muscle strength as common problems in patients with diabetic neuropathy [4]. The majority of the included studies investigated the effect of interventions and gait training in chronic diabetic participants [2] and demonstrated positive findings. The results of this review also demonstrated that rehabilitation interventions play an effective role in improving balance and proprioception, increasing the coordination of the lower limb muscles, and improving muscle strength. These findings are consistent with the results of a previous study that reviewed rehabilitation interventions [32].
Moreover, diabetic ulcers in diabetic patients are a determinant factor in their gait disorders and must be considered in the management and prevention programs. The changes in plantar pressure distribution increase ulcer formation [33], however, this was only mentioned in two studies [22, 25]. Interestingly, a few interventions were performed by healthcare providers separately from the rehabilitation specialists, including nurses and biomedical engineers [28, 30].
Due to the variable characters of DPN patients and the negative effects gait can cause, rehabilitation specialists and researchers should consider several combined multidisciplinary aspects of interventions to attain the desired outcomes based on each patient’s profile. Every person with DPN and their health providers have their own set of needs, concerns, and preferences for managing their gait problems. Also, the personal and environmental factors should be considered during treatment decision-making [14].
To facilitate the descriptive comparisons between the studies with different designs, most of the interventions in this study were extracted from pre-post intervention studies and unique studies with specific outcome measurements. With this procedure, the results are at render of overestimating the effect of the intervention and bias; this can be considered as the weakness of this study. Consequently, these interventions must be interpreted cautiously. Furthermore, the majority of the included studies had relatively small sample sizes (N<40), which may have limited the power of their analysis and findings.
Strengths and limitations of this study
To the best of our knowledge, this is the first scoping review that identifies and summarizes the available literature on rehabilitation and intervention characteristics for gait problems in patients with DPN.
Despite intending to do a comprehensive search and finding grey literature sources, there is the possibility of missing some related studies. We did our best to consider the most important results in the literature. However, due to the limited word number, it was impossible to provide a detailed discussion considering all aspects of rehabilitation interventions effects, such as participation, objective, benefits, user satisfaction, and barriers to adoption and use. This review excluded non-English studies that may lead to incomplete data composition.
Implications for future research
Our review did not find any evidence on the best rehabilitation practice for DPN patients with gait abnormalities. Based on this scoping review, the priorities and inquiries for future research should be considered as follows:
● Evaluating rehabilitation interventions for DPN patients with gait problems in all countries;
● Identifying the limitations and barriers in performing rehabilitation interventions for DPN patients;
● Performing a systematic review of rehabilitation interventions for patients with DPN and gait problems;
● And the investigation of rehabilitation interventions that aim to resolve activity restriction and participation barriers, not only impairments, in this population.
Additionally, larger sample sizes and detailed methods are required for evaluating the effectiveness of rehabilitation interventions in DPN to further strengthen the findings for or against the various modalities adoption and utilization for gait rehabilitation. Unfortunately, it is unclear whether these types of rehabilitation interventions would be applied, effective, or cost-effective in different settings (e.g. inpatient, outpatient, community, or home). These are also important questions to be explored in future studies.
4. Conclusion
A variety of studies with different rehabilitation interventions and outcome measurements have been conducted on gait abnormalities in DPN patients. The effectiveness of these rehabilitation programs in the improvement of gait abnormalities is sparse and inconclusive. It appears that more trials with appropriate control and detailed descriptions of rehabilitation interventions are needed to determine the most relevant interventions for this patient group.
Ethical Considerations
Compliance with ethical guidelines
This is an scoping review and for such manuscript there is no need to Ethical code.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization, supervision: Hamidreza Mokhtarinia, Charl Philip Gabel; Methodology: Chals Philip Gabel; Investigation, writing – review & editing: All authors; Writing – original draft: Zahra Hasani.
Conflict of interest
The authors declare no competing interests.
References
- Jember G, Melsew YA, Fisseha B, Sany K, Gelaw AY, Janakiraman B. Peripheral Sensory Neuropathy and associated factors among adult diabetes mellitus patients in Bahr Dar, Ethiopia. J Diabetes Metabo Disord. 2017; 16(1):16. [DOI:10.1186/s40200-017-0295-5] [PMID] [PMCID]
- Brown SJ, Handsaker JC, Maganaris CN, Bowling FL, Boulton AJ, Reeves ND. Altered joint moment strategy during stair walking in diabetes patients with and without peripheral neuropathy. Gait Posture. 2016; 46:188-93. [DOI:10.1016/j.gaitpost.2016.03.007] [PMID]
- van Dieren S, Beulens JW, van der Schouw YT, Grobbee DE, Neal B. The global burden of diabetes and its complications: An emerging pandemic. Eur J Cardiovasc Prev Rehabil. 2010; 17(suppl 1):s3-8. [DOI:10.1097/01.hjr.0000368191.86614.5a] [PMID]
- Menz HB, Lord SR, St George R, Fitzpatrick RC. Walking stability and sensorimotor function in older people with diabetic peripheral neuropathy. Arch Phys Med Rehabil. 2004; 85(2):245-52. [DOI:10.1016/j.apmr.2003.06.015] [PMID]
- Leinninger GM, Vincent AM, Feldman EL. The role of growth factors in diabetic peripheral neuropathy. J Peripher Nerv Syst. 2004; 9(1):26-53. [DOI:10.1111/j.1085-9489.2004.09105.x] [PMID]
- Wong MC, Chung JW, Wong TK. Effects of treatments for symptoms of painful diabetic neuropathy: Systematic review. BMJ. 2007; 335(7610):87. [DOI:10.1136/bmj.39213.565972.AE] [PMID] [PMCID]
- Boulton AJ, Vinik AI, Arezzo JC, Bril V, Feldman EL, Freeman R, et al. Diabetic neuropathies: A statement by the American Diabetes Association. Diabetes Care. 2005; 28(4):956-62. [DOI:10.2337/diacare.28.4.956] [PMID]
- Katoulis EC, Ebdon-Parry M, Lanshammar H, Vileikyte L, Kulkarni J, Boulton AJ. Gait abnormalities in diabetic neuropathy. Diabetes Care. 1997; 20(12):1904-7. [DOI:10.2337/diacare.20.12.1904] [PMID]
- Fernando M, Crowther R, Lazzarini P, Sangla K, Cunningham M, Buttner P, et al. Biomechanical characteristics of peripheral diabetic neuropathy: A systematic review and meta-analysis of findings from the gait cycle, muscle activity and dynamic barefoot plantar pressure. Clin Biomech. 2013; 28(8):831-45. [DOI:10.1016/j.clinbiomech.2013.08.004] [PMID]
- Andersen H. Motor dysfunction in diabetes. Diabetes Metab Res Rev. 2012; 28(Suppl 1):89-92. [DOI:10.1002/dmrr.2257] [PMID]
- Yavuzer G, Yetkin I, Toruner FB, Koca N, Bolukbas N. Gait deviations of patients with diabetes mellitus:Looking beyond peripheral neuropathy. Eura Medicophys. 2006; 42(2):127-33. [PMID]
- Meier MR, Desrosiers J, Bourassa P, Blaszczyk J. Effect of type II diabetic peripheral neuropathy on gait termination in the elderly. Diabetologia. 2001; 44(5):585-92. [DOI:10.1007/s001250051664] [PMID]
- Allet L, Armand S, Golay A, Monnin D, de Bie RA, de Bruin ED.Gait characteristics of diabetic patients: A systematic review. Diabetes Metab Res Rev. 2008; 24(3):173-91. [DOI:10.1002/dmrr.809] [PMID]
- White CM, Pritchard J, Turner‐Stokes L. Exercise for people with peripheral neuropathy. Cochrane Database Syst Rev. 2004; (4):CD003904. [DOI:10.1002/14651858.CD003904.pub2] [PMID]
- Allet L, Armand S, De Bie R, Golay A, Monnin D, Aminian K, et al. The gait and balance of patients with diabetes can be improved: A randomised controlled trial. Diabetologia. 2010; 53(3):458-66. [DOI:10.1007/s00125-009-1592-4] [PMID] [PMCID]
- Allet L, Armand S, de Bie RA, Golay A, Pataky Z, Aminian K, et al. Clinical factors associated with gait alterations in diabetic patients. Diabet Med. 2009; 26(10):1003-9. [DOI:10.1111/j.1464-5491.2009.02811.x] [PMID]
- Alam U, Riley DR, Jugdey RS, Azmi S, Rajbhandari S, D'Août K, et al. Diabetic neuropathy and gait: A review. Diabetes Ther. 2017; 8(6):1253-64. [DOI:10.1007/s13300-017-0295-y] [PMID] [PMCID]
- Mustapa A, Justine M, Mohd Mustafah N, Jamil N, Manaf H. Postural control and gait performance in the diabetic peripheral neuropathy: A systematic review. Biomed Res Int. 2016; 2016:9305025[DOI:10.1155/2016/9305025] [PMID] [PMCID]
- Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol. 2005; 8(1):19-32. [DOI:10.1080/1364557032000119616]
- Mays N, Roberts E, Popay J. Synthesising research evidence. Fulop N, editor. Studying the organisation and delivery of health services: Research methods. London and New York: Psychology Press; 2001. https://books.google.com/books?hl=en&lr=&id=6n6BAgAAQBAJ&oi=fnd&pg=PA188&dq
- Riva JJ, Malik KM, Burnie SJ, Endicott AR, Busse JW. What is your research question? An introduction to the PICOT format for clinicians. J Can ChiroprAssoc. 2012; 56(3):167-71. [PMID] [PMCID]
- Zhang X, Zhang Y, Gao X, Wu J, Jiao X, Zhao J, et al. Investigating the role of backward walking therapy in alleviating plantar pressure of patients with diabetic peripheral neuropathy. Arch Phys Med Rehabil. 2014; 95(5):832-9. [DOI:10.1016/j.apmr.2014.01.003] [PMID]
- Ahmad I, Verma S, Noohu MM, Shareef MY, Hussain ME. Sensorimotor and gait training improves proprioception, nerve function, and muscular activation in patients with diabetic peripheral neuropathy: A randomized control trial. J Musculoskelet Neuronal Interact. 2020; 20(2):234-48. [PMID] [PMCID]
- El-refay BH, Ali OI. Efficacy of exercise rehabilitation program in improving gait of diabetic neuropathy patients. The Medical Journal of Cairo University. 2014; 82(2):22532. https://scholar.cu.edu.eg/sites/default/files/olfatibrahim/files/efficacy_of_exercise_rehabilitation_program_in_improving_gait_of_diabetic_neuropathy_patients_.pdf
- Sartor CD, Hasue RH, Cacciari LP, Butugan MK, Watari R, Pássaro AC, et al. Effects of strengthening, stretching and functional training on foot function in patients with diabetic neuropathy: Results of a randomized controlled trial. BMC Musculoskeletal Disord. 2014; 15:137. [DOI:10.1186/1471-2474-15-137] [PMID] [PMCID]
- Suzuki K, Niitsu M, Kamo T, Otake S, Nishida Y. Effect of exercise with rhythmic auditory stimulation on muscle coordination and gait stability in patients with diabetic peripheral neuropathy: A randomized controlled trial. Open J Ther Rehabil. 2019; 7(03):79. [DOI:10.4236/ojtr.2019.73005]
- Rehab NI, Saleh MSM. Effect of ankle proprioceptive training on gait and risk of fall in patients with diabetic neuropathy: A randomized controlled trial. Int J Diabetes Res. 2019; 2(1):40-5. http://www.ghrnet.org/index.php/ijdr/article/view/2564/2892
- Kang GE, Zahiri M, Lepow B, Saleem N, Najafi B. The effect of daily use of plantar mechanical stimulation through micro-mobile foot compression device installed in shoe insoles on vibration perception, gait, and balance in people with diabetic peripheral neuropathy. J Diabetes Sci Technol. 2019; 13(5):847-56. [DOI:10.1177/1932296819839703] [PMID] [PMCID]
- Ghomian B, Naemi R, Mehdizadeh S, Jafari H, Ebrahimi Takamjani I, Aghili R, et al. Gait stability of diabetic patients is altered with the rigid rocker shoes. Clin Biomech. 2019; 69:197-204. [DOI:10.1016/j.clinbiomech.2019.06.015] [PMID]
- Paul L, Ellis BM, Leese GP, McFadyen AK, McMurray B. The effect of a cognitive or motor task on gait parameters of diabetic patients, with and without neuropathy. Diabet Med. 2009; 26(3):234-9. [DOI:10.1111/j.1464-5491.2008.02655.x] [PMID]
- Ortiz-Piña M, Salas-Fariña Z, Mora-Traverso M, Martín-Martín L, Galiano-Castillo N, García-Montes I, et al. A home-based tele-rehabilitation protocol for patients with hip fracture called @ctivehip. Res Nurs Health. 2019; 42(1):29-38. [DOI:10.1002/nur.21922] [PMID]
- Morrison S, Colberg SR, Mariano M, Parson HK, Vinik AI. Balance training reduces falls risk in older individuals with type 2 diabetes. Diabetes Care. 2010; 33(4):748-50. [DOI:10.2337/dc09-1699] [PMID] [PMCID]
- Van Deursen R. Mechanical loading and off-loading of the plantar surface of the diabetic foot. Clin Infect Dis. 2004; 39(Supplement 2):S87-91. [DOI:10.1086/383268] [PMID]
Type of Study: Review Article |
Subject:
Physiotherapy
Received: 2020/11/1 | Accepted: 2020/12/20 | Published: 2020/12/3
Received: 2020/11/1 | Accepted: 2020/12/20 | Published: 2020/12/3