Volume 3, Issue 1 (Continuously Updated 2020)
Func Disabil J 2020, 3(1): 185-192 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Lajevardi L, Taghizade G, Parnain Z. The Effect of Psychological Factors on Cognitive Functions in Stroke Patients With Chronic Fatigue. Func Disabil J 2020; 3 (1) :185-192
URL: http://fdj.iums.ac.ir/article-1-133-en.html
URL: http://fdj.iums.ac.ir/article-1-133-en.html
1- Department of Occupational Therapy, School of Rehabilitation Sciences, Iran's University of Medical Sciences, Tehran, Iran. , laleh23275@yahoo.com
2- Department of Occupational Therapy, School of Rehabilitation Sciences, Iran's University of Medical Sciences, Tehran, Iran.
2- Department of Occupational Therapy, School of Rehabilitation Sciences, Iran's University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 1064 kb]
(813 Downloads)
| Abstract (HTML) (2211 Views)
Full-Text: (1096 Views)
Introduction
Stroke or cerebrovascular accident results from the disruption of blood flow to brain cells and leads to the impairment of brain functions. Stroke is the second most common cause of death and physical and cognitive disabilities in adults [1].
Stroke is more common among the elderly, as one out of three old adults experiences strokes, dementia, or both. A total number of 15 million people worldwide have strokes each year, and about 30% of them suffer from stroke-related disabilities [2]. Besides functional and physical disabilities, stroke can lead to fatigue, cognitive impairment, and psychological disorders, such as anxiety, depression, and stress, which are often overlooked [3]. Chronic stroke-related cognitive impairments may affect various domains, such as attention, concentration, memory, social cognition, language, spatial orientation, perceptual skills, and higher-order executive functions. Also, the most common cognitive impairments include memory, orientation, language, attention problems, executive impairment (initiation inhibition and mental flexibility), and aphasia [4].
Moreover, chronic fatigue affects cognitive functions in patients with chronic stroke. Post-stroke chronic fatigue is described as a feeling of rapid tiredness and exhaustion, the lack of energy, and extreme effort aversion, which occur during physical or mental activities, do not improve with rest, and usually last for at least six months [5]. The common symptoms of chronic fatigue include weakness, muscle aches, poor memory, mental disorientation, insomnia, chest pain, confusion, night sweats, weight loss, and psychological problems, such as depression, irritability, anxiety, etc. Cognitive impairments associated with chronic fatigue affect memory, attention, information processing speed, and cognitive reaction time. Chronic fatigue can also affect the memorization and retrieval of general, occupational, or scientific information. Due to the high prevalence of cognitive problems in chronic fatigue patients, the authors found it crucially important to investigate factors affecting cognitive functions in chronic stroke patients with chronic fatigue [6, 7].
Depression and anxiety are the most common mood disorders in stroke survivors. Depression, anxiety, and stress may reflect a general psychological distress with exacerbating cognitive defect that often remains unknown and/or untreated. The prevalence of moderate to severe depression and anxiety in stroke survivors is 22.8% and 21.1%, respectively [8]. In patients with chronic stroke, depression is accompanied by symptoms, such as low energy; the feeling of tiredness; poor concentration and memory; indecisiveness; the constant feeling of sadness and uselessness; helplessness and frustration; changes in appetite; the loss of interest in appearance; and cognitive function impairments in attention, executive functioning, memory, and processing speed [9]. Depression and anxiety often occur simultaneously, however, depression is more severe, and depressed patients experience a higher level of functional and cognitive impairment. In patients with chronic stroke, cognitive factors, such as information processing speed and verbal memory are more related to mood disorders (e.g. depression and anxiety) than the level of physical independence [8]. Anxiety is characterized by excessive, persistent, and often unrealistic worries, which are common and very debilitating after a stroke and impair rehabilitation activities. Besides, anxiety disorders impair cognitive functions, such as perception, attention, memory, executive functions, working memory, and planning [10]. Also, stress results from the post-stroke physical, psychological, and social pressures. The cognitive effects of stress are among its major consequences. According to Lazarus and Folkman (1984), the major psychosocial aspect of stress is associated with its effect on memory and concentration, because stress often disrupts the functions of the mind by diverting attention [11].
Because of the high prevalence of chronic stroke worldwide and strong evidence on the significant impact of psychological factors on the cognitive functions of patients with other neurological diseases, this study aimed to investigate the role of psychological factors in the cognitive functions of chronic stroke patients with chronic fatigue.
2. Materials and Methods
This correlational study was conducted from May to September 2019. The researchers used non-probability sampling to enroll 85 patients who have chronic fatigue among the patients with chronic stroke visiting in the Rehabilitation Centers of Tehran. We enrolled patients who had been diagnosed (by a neurologist) with chronic stroke at least six months ago and had also developed chronic fatigue (Fatigue Severity Scale (FSS) scores ≥ 4). The exclusion criteria included other neurological disorders, such as Parkinson disease; orthopedic or rheumatologic disorders; and visuospatial neglect (i.e. score ≥ 44 on star cancellation test), based on the diagnosis of a neurologist and the medical records. Also, all participants signed a written consent form, and the protocol was approved by the Ethics Committee of Iran University of Medical Sciences (IR.IUMS.REC.1397.1262).
A demographic questionnaire was used to record demographic and clinical information, such as age, gender, dominant hand, educational qualifications, the type of stroke, affected side, and the time passed from the stroke. Fatigue levels were measured using FSS, while the Mini-Mental State Examination (MMSE) and Montreal Cognitive Assessment (MoCA) were used to assess the cognitive functions of the participants. Also, the Beck Depression Inventory (BDI) and the Beck Anxiety Inventory (BAI) were used to measure depression and anxiety levels, respectively. The obtained data were analyzed in SPSS V. 22 using the Pearson correlation test, the Spearman correlation test, and multivariate regression.
Data collection method and tools
Patient demographics questionnaire: This form was given to the subjects to collect demographic data, such as age, gender, and education level.
Mini-Mental State Examination: This test was first published in 1975 by Folstein for assessing the cognitive status of the elderly. The MMSE examines orientation abilities; short-term memory; reading, writing, calculating, seeing, and drawing skills; and the ability to discover relations between objects or images. This test is performed and scored quickly, and can be carried out by any member of the rehabilitation team. The total score is 30, and a score of 23 or lower indicates cognitive impairment. The test has a suitable validity (the Cronbach alpha = 0.78) [12].
Montreal Cognitive Assessment: The MoCA is a screening tool for the assessment of mild cognitive impairment. Nasreddin et al. (2005) validated this tool and evaluated its reliability. This test assesses eight cognitive domains (short-term memory, visuospatial abilities, executive functions, attention, concentration, working memory, language, and orientation to time and place) in less than 15 minutes. The maximum score is 30 and higher scores indicate better cognitive functions. Also, one point is added to the total score of those with less than 12 years of education. The MoCA has a high test-retest reliability and a high sensitivity in diagnosing mild cognitive impairment (90%) and Alzheimer disease (100%) [13].
Beck Depression Inventory: The BDI is widely used to assess depression in normal people and those with mental health problems. It has been translated into Persian by Ghasemzadeh (2005). This 21-item inventory assesses the symptoms of inability, failure, guilt, irritability, sleep disturbance, and loss of appetite. The participants are asked to complete the inventory based on their condition over the past two weeks using a 4-point Likert scale scored from 0 to 3. The total score ranges from 0 to 63, and higher scores indicate more severe depression [14].
Beck Anxiety Inventory: This 21-item inventory assesses anxiety symptoms that are not associated with depression. The items are scored on a 4-point Likert scale from “not at all” (score 0) to “severe” (score 3). In total, 14 items represent physical symptoms (eg, hand tremors) and seven items represent thoughts or feelings (eg, the fear of death). The BAI scores range from 0 to 63, and higher scores indicate higher levels of anxiety [15].
Fatigue Severity Scale: This scale was developed by Krupp et al. (1989) to assess the severity of fatigue in people with multiple sclerosis and lupus. The psychometric properties of this 9-item scale have been confirmed. It is currently used to measure fatigue levels in patients with chronic diseases. The FSS items have been extracted from the 28 items of the fatigue questionnaire. Besides, the FSS scores range from 1 (completely disagree) to 7 (completely agree), and the scores of greater than four indicate chronic fatigue. The validity and reliability of the Persian version of this scale have been confirmed by Azimian et al. (2013) (the Cronbach alpha = 0.96) [16].
3. Results
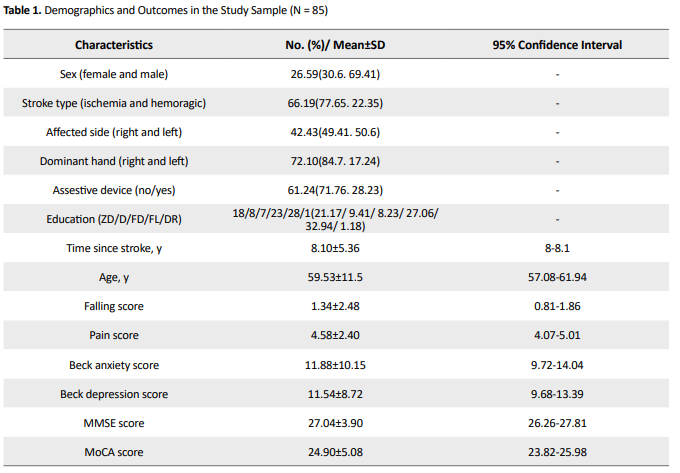
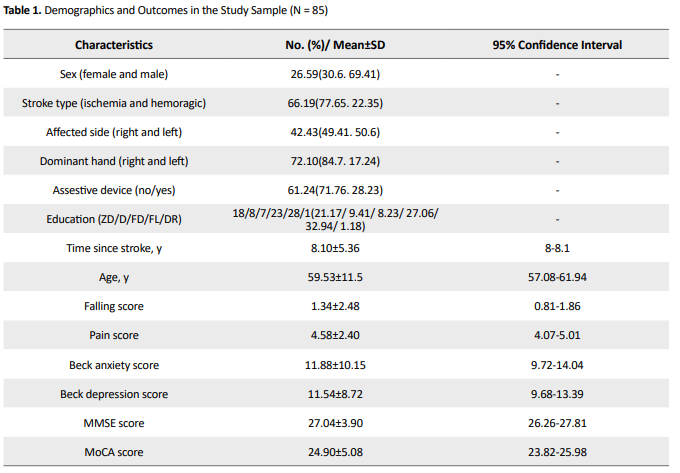
Out of 85 participants, 59 were male. The Mean±SD of participants’ age and time passed from the stroke were 59.52±11.5 years and 8.1±5.36 years, respectively. Table 1 presents the demographic and clinical characteristics of the participants. Based on the results, cognitive functions were not significantly correlated with gender, the type of stroke, affected side, dominant hand, the use of assistive devices, time passed from the stroke, age, the history of falls, and pain.
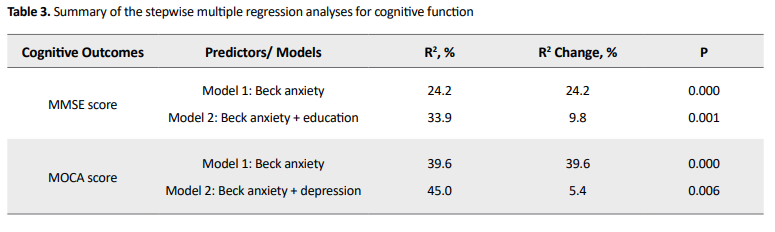
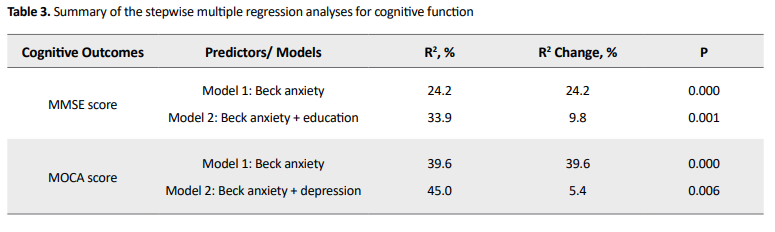
However, cognitive functions had significant correlations with the predictor variables of anxiety, depression, and education (Table 2).

According to the regression models, MMSE and MoCA explained up to 24.2% and 39.6% of the variance of cognitive functions, respectively. In all step-by-step models designed based on MMSE and MoCA tests, anxiety was the strongest predictor of cognitive functions. The second predictors of cognitive functions were education level in MMSE and depression in MoCA (Table 3).
4. Discussion
This study investigated the role of psychological factors in the cognitive functions of chronic stroke patients with chronic fatigue. Anxiety was the strongest predictor of cognitive functions and was followed by depression and educational qualifications. This finding highlights the specific role of psychological factors in improving the cognitive functions of chronic stroke patients with chronic fatigue.
Considering the high prevalence of cognitive and psychological impairments in patients with chronic stroke [17] and strong evidence on the significant impact of psychological factors on the cognitive functions of patients with other neurological diseases [8], this study investigated the effect of psychological factors on the cognitive functions of chronic stroke patients with chronic fatigue. Based on the findings, anxiety was the best predictor of cognitive functions in chronic stroke patients with chronic fatigue. Wie Li et al. (2019) found that anxiety is common in the acute and chronic stages of ischemic stroke with mild-to-moderate neurologic defects. They also found that anxiety can affect cognitive functions [18]. Anxiety disorders can also affect brain areas, such as the amygdala, hippocampus, limbic system, and the paraventricular nuclei of the hypothalamus through making neurochemical changes in neurotransmitters, such as GABA, adenosine, melatonin, glutamate, serotonin, and acetylcholine [19]. The chronic dysregulation of these neurotransmitters can damage the hippocampus, which plays a key role in memory and attention functions [20].
Depression was another important predictor of cognitive functions. Previous studies have extensively investigated the relationship between depression and cognitive functions. Using BAI and BDI, Maria et al. (2018) found that cognitive functions were strongly correlated with anxiety and depression in the acute stage of stroke and two months after the event [21]. Also, Luisa Terroni et al. (2012) conducted neuropsychological tests to assess the cognitive functions of stroke survivors three months after the event. They found that impairments in cognitive functions, such as orientation, language, executive/motor functions, memory, attention, and psychomotor speed were associated with depression. They also found that these impairments can last for a long time [22]. Moreover, Lena Rafsten et al. (2018) found that anxiety was highly related and comorbid with depression. Besides, anxiety could be one of the predictors of depression [23]. Ho-Yan Yvonne Chun et al. (2018) found that anxiety disorders and depression can be profoundly disabling and need to be considered as the important outcomes of stroke [24]. These factors affect dependence, quality of life, and social participation in patients with stroke. Thus, the management of anxiety could help prevent depression after stroke. Also, anxiety significantly influences the quality of daily life [25].
The level of education was strongly correlated with cognitive performance in patients with chronic stroke. De Ronchi et al. (2007) found that cognitive impairments were more prevalent in people with lower levels of education. Thus, these people are highly prone to dementia [26]. Furthermore, Mohd Faizal (2016) introduced poor education as a risk factor for cognitive problems, such as impaired concentration in stroke patients [17]. Stern (2012) found that patients with higher education levels might have better pre-stroke cognition, and therefore, show better post-stroke cognitive performance than patients with lower education, despite comparable stroke damage. In other words, in the case of higher reserve, the brain can simply tolerate more pathology before it reaches a critical threshold and the patient presents a cognitive deficit [27]. Brayne (2010) found that individuals with higher cognitive reserve may be more capable of recruiting alternative neural networks to maintain function [28]. In this regard, Stefener et al., (2011) found that patients with higher education levels usually have a healthier lifestyle and better compliance with vascular risk factor management, and cognitive reserve might interact with brain reserve [29].
Changes in the frontal and parietal neural circuits, thalamus, and basal ganglia may create a major pathway in the pathophysiology of mental fatigue and cognitive dysfunction in chronic fatigue. Consistent with cognitive function results, other studies have confirmed the potential role of the autonomic nervous system in the emergence of chronic fatigue symptoms. In another study, fatigue negatively affected personal performance and seemed to have some effects on memory [28]. Neurochemical mechanisms in chronic fatigue and anxiety disorders are associated with damages to the common areas of the brain, including the parietal lobe (which includes the hippocampus), and lead to cognitive impairments. Therefore, anxiety disorders double the possibility of impairing cognitive functions in stroke patients who have chronic fatigue [29].
The clinical outcome of this finding is that psychological factors, such as anxiety and depression in patients with chronic stroke and chronic fatigue can affect cognitive factors, including problems in focusing and attention, memory, difficulty in finding words, the reduced speed of information processing, mental exhaustion, and sluggishness. Therefore, the therapeutic role of psychological factors should be considered to improve cognitive factors in patients with chronic stroke and chronic fatigue.
Nevertheless, some limitations should be addressed by future research. A major limitation was the sample size. Future research should examine the generalizability of the findings on a larger sample and compare it with other inpatients. We recommend consulting with primary caregivers or family members about the behavior or emotions of individual patients at home; this is essential to understand the different emotions of patients with different post-stroke severity and provide the right support and care.
5. Conclusion
These findings confirm that clinicians should be trained to evaluate anxiety, depression, and fatigue as well as cognitive functioning and show that psychological symptoms, such as anxiety, depression, and fatigue are correlated with cognitive function. However, cognitive functioning plays an important role in predicting the outcomes of rehabilitation programs and the quality of life in stroke patients. If confirmed by future research, the results of this study could have implications in clinical practice. The assessment of both anxiety and depression plays an important role in the various stages of stroke. Moreover, clinicians should consider the need for psychological support for patients receiving rehabilitation services.
Ethical Considerations
Compliance with ethical guidelines
The ethics committee of Iran University of Medical Sciences confirmed the study (IR.IUMS.REC. 1398. 895). Also, all participants read the consent form and agreed to participate in the study.
Funding
This article is part of the MSc. thesis of the first author in the Department of Occupational Therapy, School of Rehabilitation Sciences, Iran University of Medical Sciences. Also, this study was supported by Iran University of Medical Sciences, Tehran.
Authors' contributions
Conceptualization, supervision: Laleh Lajevardi, Ghorban Taghizade; Methodology: Laleh Lajevardi, Zahra Parnian; Investigation, writing – review & editing: All authors; Writing – original draft: Laleh Lajevardi, Zahra Parnian; Funding acquisition, resources: Laleh Lajevardi, Zahra Parnian.
Conflict of interest
The authors declared no conflict of interest.
References
Stroke or cerebrovascular accident results from the disruption of blood flow to brain cells and leads to the impairment of brain functions. Stroke is the second most common cause of death and physical and cognitive disabilities in adults [1].
Stroke is more common among the elderly, as one out of three old adults experiences strokes, dementia, or both. A total number of 15 million people worldwide have strokes each year, and about 30% of them suffer from stroke-related disabilities [2]. Besides functional and physical disabilities, stroke can lead to fatigue, cognitive impairment, and psychological disorders, such as anxiety, depression, and stress, which are often overlooked [3]. Chronic stroke-related cognitive impairments may affect various domains, such as attention, concentration, memory, social cognition, language, spatial orientation, perceptual skills, and higher-order executive functions. Also, the most common cognitive impairments include memory, orientation, language, attention problems, executive impairment (initiation inhibition and mental flexibility), and aphasia [4].
Moreover, chronic fatigue affects cognitive functions in patients with chronic stroke. Post-stroke chronic fatigue is described as a feeling of rapid tiredness and exhaustion, the lack of energy, and extreme effort aversion, which occur during physical or mental activities, do not improve with rest, and usually last for at least six months [5]. The common symptoms of chronic fatigue include weakness, muscle aches, poor memory, mental disorientation, insomnia, chest pain, confusion, night sweats, weight loss, and psychological problems, such as depression, irritability, anxiety, etc. Cognitive impairments associated with chronic fatigue affect memory, attention, information processing speed, and cognitive reaction time. Chronic fatigue can also affect the memorization and retrieval of general, occupational, or scientific information. Due to the high prevalence of cognitive problems in chronic fatigue patients, the authors found it crucially important to investigate factors affecting cognitive functions in chronic stroke patients with chronic fatigue [6, 7].
Depression and anxiety are the most common mood disorders in stroke survivors. Depression, anxiety, and stress may reflect a general psychological distress with exacerbating cognitive defect that often remains unknown and/or untreated. The prevalence of moderate to severe depression and anxiety in stroke survivors is 22.8% and 21.1%, respectively [8]. In patients with chronic stroke, depression is accompanied by symptoms, such as low energy; the feeling of tiredness; poor concentration and memory; indecisiveness; the constant feeling of sadness and uselessness; helplessness and frustration; changes in appetite; the loss of interest in appearance; and cognitive function impairments in attention, executive functioning, memory, and processing speed [9]. Depression and anxiety often occur simultaneously, however, depression is more severe, and depressed patients experience a higher level of functional and cognitive impairment. In patients with chronic stroke, cognitive factors, such as information processing speed and verbal memory are more related to mood disorders (e.g. depression and anxiety) than the level of physical independence [8]. Anxiety is characterized by excessive, persistent, and often unrealistic worries, which are common and very debilitating after a stroke and impair rehabilitation activities. Besides, anxiety disorders impair cognitive functions, such as perception, attention, memory, executive functions, working memory, and planning [10]. Also, stress results from the post-stroke physical, psychological, and social pressures. The cognitive effects of stress are among its major consequences. According to Lazarus and Folkman (1984), the major psychosocial aspect of stress is associated with its effect on memory and concentration, because stress often disrupts the functions of the mind by diverting attention [11].
Because of the high prevalence of chronic stroke worldwide and strong evidence on the significant impact of psychological factors on the cognitive functions of patients with other neurological diseases, this study aimed to investigate the role of psychological factors in the cognitive functions of chronic stroke patients with chronic fatigue.
2. Materials and Methods
This correlational study was conducted from May to September 2019. The researchers used non-probability sampling to enroll 85 patients who have chronic fatigue among the patients with chronic stroke visiting in the Rehabilitation Centers of Tehran. We enrolled patients who had been diagnosed (by a neurologist) with chronic stroke at least six months ago and had also developed chronic fatigue (Fatigue Severity Scale (FSS) scores ≥ 4). The exclusion criteria included other neurological disorders, such as Parkinson disease; orthopedic or rheumatologic disorders; and visuospatial neglect (i.e. score ≥ 44 on star cancellation test), based on the diagnosis of a neurologist and the medical records. Also, all participants signed a written consent form, and the protocol was approved by the Ethics Committee of Iran University of Medical Sciences (IR.IUMS.REC.1397.1262).
A demographic questionnaire was used to record demographic and clinical information, such as age, gender, dominant hand, educational qualifications, the type of stroke, affected side, and the time passed from the stroke. Fatigue levels were measured using FSS, while the Mini-Mental State Examination (MMSE) and Montreal Cognitive Assessment (MoCA) were used to assess the cognitive functions of the participants. Also, the Beck Depression Inventory (BDI) and the Beck Anxiety Inventory (BAI) were used to measure depression and anxiety levels, respectively. The obtained data were analyzed in SPSS V. 22 using the Pearson correlation test, the Spearman correlation test, and multivariate regression.
Data collection method and tools
Patient demographics questionnaire: This form was given to the subjects to collect demographic data, such as age, gender, and education level.
Mini-Mental State Examination: This test was first published in 1975 by Folstein for assessing the cognitive status of the elderly. The MMSE examines orientation abilities; short-term memory; reading, writing, calculating, seeing, and drawing skills; and the ability to discover relations between objects or images. This test is performed and scored quickly, and can be carried out by any member of the rehabilitation team. The total score is 30, and a score of 23 or lower indicates cognitive impairment. The test has a suitable validity (the Cronbach alpha = 0.78) [12].
Montreal Cognitive Assessment: The MoCA is a screening tool for the assessment of mild cognitive impairment. Nasreddin et al. (2005) validated this tool and evaluated its reliability. This test assesses eight cognitive domains (short-term memory, visuospatial abilities, executive functions, attention, concentration, working memory, language, and orientation to time and place) in less than 15 minutes. The maximum score is 30 and higher scores indicate better cognitive functions. Also, one point is added to the total score of those with less than 12 years of education. The MoCA has a high test-retest reliability and a high sensitivity in diagnosing mild cognitive impairment (90%) and Alzheimer disease (100%) [13].
Beck Depression Inventory: The BDI is widely used to assess depression in normal people and those with mental health problems. It has been translated into Persian by Ghasemzadeh (2005). This 21-item inventory assesses the symptoms of inability, failure, guilt, irritability, sleep disturbance, and loss of appetite. The participants are asked to complete the inventory based on their condition over the past two weeks using a 4-point Likert scale scored from 0 to 3. The total score ranges from 0 to 63, and higher scores indicate more severe depression [14].
Beck Anxiety Inventory: This 21-item inventory assesses anxiety symptoms that are not associated with depression. The items are scored on a 4-point Likert scale from “not at all” (score 0) to “severe” (score 3). In total, 14 items represent physical symptoms (eg, hand tremors) and seven items represent thoughts or feelings (eg, the fear of death). The BAI scores range from 0 to 63, and higher scores indicate higher levels of anxiety [15].
Fatigue Severity Scale: This scale was developed by Krupp et al. (1989) to assess the severity of fatigue in people with multiple sclerosis and lupus. The psychometric properties of this 9-item scale have been confirmed. It is currently used to measure fatigue levels in patients with chronic diseases. The FSS items have been extracted from the 28 items of the fatigue questionnaire. Besides, the FSS scores range from 1 (completely disagree) to 7 (completely agree), and the scores of greater than four indicate chronic fatigue. The validity and reliability of the Persian version of this scale have been confirmed by Azimian et al. (2013) (the Cronbach alpha = 0.96) [16].
3. Results
Out of 85 participants, 59 were male. The Mean±SD of participants’ age and time passed from the stroke were 59.52±11.5 years and 8.1±5.36 years, respectively. Table 1 presents the demographic and clinical characteristics of the participants. Based on the results, cognitive functions were not significantly correlated with gender, the type of stroke, affected side, dominant hand, the use of assistive devices, time passed from the stroke, age, the history of falls, and pain.
However, cognitive functions had significant correlations with the predictor variables of anxiety, depression, and education (Table 2).

According to the regression models, MMSE and MoCA explained up to 24.2% and 39.6% of the variance of cognitive functions, respectively. In all step-by-step models designed based on MMSE and MoCA tests, anxiety was the strongest predictor of cognitive functions. The second predictors of cognitive functions were education level in MMSE and depression in MoCA (Table 3).
4. Discussion
This study investigated the role of psychological factors in the cognitive functions of chronic stroke patients with chronic fatigue. Anxiety was the strongest predictor of cognitive functions and was followed by depression and educational qualifications. This finding highlights the specific role of psychological factors in improving the cognitive functions of chronic stroke patients with chronic fatigue.
Considering the high prevalence of cognitive and psychological impairments in patients with chronic stroke [17] and strong evidence on the significant impact of psychological factors on the cognitive functions of patients with other neurological diseases [8], this study investigated the effect of psychological factors on the cognitive functions of chronic stroke patients with chronic fatigue. Based on the findings, anxiety was the best predictor of cognitive functions in chronic stroke patients with chronic fatigue. Wie Li et al. (2019) found that anxiety is common in the acute and chronic stages of ischemic stroke with mild-to-moderate neurologic defects. They also found that anxiety can affect cognitive functions [18]. Anxiety disorders can also affect brain areas, such as the amygdala, hippocampus, limbic system, and the paraventricular nuclei of the hypothalamus through making neurochemical changes in neurotransmitters, such as GABA, adenosine, melatonin, glutamate, serotonin, and acetylcholine [19]. The chronic dysregulation of these neurotransmitters can damage the hippocampus, which plays a key role in memory and attention functions [20].
Depression was another important predictor of cognitive functions. Previous studies have extensively investigated the relationship between depression and cognitive functions. Using BAI and BDI, Maria et al. (2018) found that cognitive functions were strongly correlated with anxiety and depression in the acute stage of stroke and two months after the event [21]. Also, Luisa Terroni et al. (2012) conducted neuropsychological tests to assess the cognitive functions of stroke survivors three months after the event. They found that impairments in cognitive functions, such as orientation, language, executive/motor functions, memory, attention, and psychomotor speed were associated with depression. They also found that these impairments can last for a long time [22]. Moreover, Lena Rafsten et al. (2018) found that anxiety was highly related and comorbid with depression. Besides, anxiety could be one of the predictors of depression [23]. Ho-Yan Yvonne Chun et al. (2018) found that anxiety disorders and depression can be profoundly disabling and need to be considered as the important outcomes of stroke [24]. These factors affect dependence, quality of life, and social participation in patients with stroke. Thus, the management of anxiety could help prevent depression after stroke. Also, anxiety significantly influences the quality of daily life [25].
The level of education was strongly correlated with cognitive performance in patients with chronic stroke. De Ronchi et al. (2007) found that cognitive impairments were more prevalent in people with lower levels of education. Thus, these people are highly prone to dementia [26]. Furthermore, Mohd Faizal (2016) introduced poor education as a risk factor for cognitive problems, such as impaired concentration in stroke patients [17]. Stern (2012) found that patients with higher education levels might have better pre-stroke cognition, and therefore, show better post-stroke cognitive performance than patients with lower education, despite comparable stroke damage. In other words, in the case of higher reserve, the brain can simply tolerate more pathology before it reaches a critical threshold and the patient presents a cognitive deficit [27]. Brayne (2010) found that individuals with higher cognitive reserve may be more capable of recruiting alternative neural networks to maintain function [28]. In this regard, Stefener et al., (2011) found that patients with higher education levels usually have a healthier lifestyle and better compliance with vascular risk factor management, and cognitive reserve might interact with brain reserve [29].
Changes in the frontal and parietal neural circuits, thalamus, and basal ganglia may create a major pathway in the pathophysiology of mental fatigue and cognitive dysfunction in chronic fatigue. Consistent with cognitive function results, other studies have confirmed the potential role of the autonomic nervous system in the emergence of chronic fatigue symptoms. In another study, fatigue negatively affected personal performance and seemed to have some effects on memory [28]. Neurochemical mechanisms in chronic fatigue and anxiety disorders are associated with damages to the common areas of the brain, including the parietal lobe (which includes the hippocampus), and lead to cognitive impairments. Therefore, anxiety disorders double the possibility of impairing cognitive functions in stroke patients who have chronic fatigue [29].
The clinical outcome of this finding is that psychological factors, such as anxiety and depression in patients with chronic stroke and chronic fatigue can affect cognitive factors, including problems in focusing and attention, memory, difficulty in finding words, the reduced speed of information processing, mental exhaustion, and sluggishness. Therefore, the therapeutic role of psychological factors should be considered to improve cognitive factors in patients with chronic stroke and chronic fatigue.
Nevertheless, some limitations should be addressed by future research. A major limitation was the sample size. Future research should examine the generalizability of the findings on a larger sample and compare it with other inpatients. We recommend consulting with primary caregivers or family members about the behavior or emotions of individual patients at home; this is essential to understand the different emotions of patients with different post-stroke severity and provide the right support and care.
5. Conclusion
These findings confirm that clinicians should be trained to evaluate anxiety, depression, and fatigue as well as cognitive functioning and show that psychological symptoms, such as anxiety, depression, and fatigue are correlated with cognitive function. However, cognitive functioning plays an important role in predicting the outcomes of rehabilitation programs and the quality of life in stroke patients. If confirmed by future research, the results of this study could have implications in clinical practice. The assessment of both anxiety and depression plays an important role in the various stages of stroke. Moreover, clinicians should consider the need for psychological support for patients receiving rehabilitation services.
Ethical Considerations
Compliance with ethical guidelines
The ethics committee of Iran University of Medical Sciences confirmed the study (IR.IUMS.REC. 1398. 895). Also, all participants read the consent form and agreed to participate in the study.
Funding
This article is part of the MSc. thesis of the first author in the Department of Occupational Therapy, School of Rehabilitation Sciences, Iran University of Medical Sciences. Also, this study was supported by Iran University of Medical Sciences, Tehran.
Authors' contributions
Conceptualization, supervision: Laleh Lajevardi, Ghorban Taghizade; Methodology: Laleh Lajevardi, Zahra Parnian; Investigation, writing – review & editing: All authors; Writing – original draft: Laleh Lajevardi, Zahra Parnian; Funding acquisition, resources: Laleh Lajevardi, Zahra Parnian.
Conflict of interest
The authors declared no conflict of interest.
References
- Strong K, Mathers C, Bonita R. Preventing stroke: Saving lives around the world. Lancet Neurol. 2007; 6(2):182-7. [DOI:10.1016/S1474-4422(07)70031-5]
- World Health Organization. The atlas of heart disease and stroke / Judith Mackay and George Mensah ; with Shanthi Mendis and Kurt Greenland [Internet]. 2004 [Updated 2004]. Available from: https://apps.who.int/iris/handle/10665/43007
- Mukherjee D, Levin RL, Heller W. The cognitive, emotional, and social sequelae of stroke: Psychological and ethical concerns in post-stroke adaptation. Top Stroke Rehabil. 2006; 13(4):26-35. [DOI:10.1310/tsr1304-26] [PMID]
- Meyer JS, Xu G, Thornby J, Chowdhury MH, Quach M. Is mild cognitive impairment prodromal for vascular dementia like Alzheimer’s disease? Stroke. 2002; 33(8):1981-5. [DOI:10.1161/01.STR.0000024432.34557.10] [PMID]
- staub F, Bogousslavsky J. Fatigue after stroke: A major but neglected issue. Cerebrovasc Dis. 2001; 12(2):75-81. [DOI:10.1159/000047685] [PMID]
- Cockshell SJ, Mathias JL. Cognitive functioning in chronic fatigue syndrome: A meta-analysis. Psychol Med. 2010; 40(8):1253-67.[DOI:10.1017/S0033291709992054] [PMID]
- Shanks L, Jason LA, Evans M, Brown A. Cognitive impairments associated with CFS and POTS. Front Physiol. 2013; 4:113. [DOI:10.3389/fphys.2013.00113] [PMID] [PMCID]
- Barker-Collo SL. Depression and anxiety 3 months post stroke: Prevalence and correlates. Arch Clin Neuropsychol. 2007; 22(4):519-31. [DOI:10.1016/j.acn.2007.03.002] [PMID]
- Perini G, Cotta Ramusino M, Sinforiani E, Bernini S, Petrachi R, Costa A. Cognitive impairment in depression: Recent advances and novel treatments. Neuropsychiatr Dis Treat. 2019; 15:1249. [DOI:10.2147/NDT.S199746] [PMID] [PMCID]
- Robinson OJ, Vytal K, Cornwell BR, Grillon C. The impact of anxiety upon cognition: Perspectives from human threat of shock studies. Front Hum Neurosci. 2013; 7:203. [DOI:10.3389/fnhum.2013.00203] [PMID] [PMCID]
- Oei NY, Everaerd WT, Elzinga BM, van Well S, Bermond B. Psychosocial stress impairs working memory at high loads: An association with cortisol levels and memory retrieval. Stress. 2006; 9(3):133-41. [DOI:10.1080/10253890600965773] [PMID]
- Foroughan M, Jafari Z, Shirinbayan P, Ghaem Magham Farahni Z, Rahgozar M.[ Standardization of mini-mental state examination among Iranian elderly in Tehran (Persian)]. Cogn Sci. 2008; 10(2):29-37. http://icssjournal.ir/article-1-422-fa.html
- Duro D, Simões MR, Ponciano E, Santana I. Validation studies of the Portuguese experimental version of the Montreal Cognitive Assessment (MoCA): Confirmatory factor analysis. J Neurol. 2010; 257(5):728-34. [DOI:10.1007/s00415-009-5399-5] [PMID]
- Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a Persian‐language version of the Beck Depression Inventory‐Second edition: BDI‐II‐PERSIAN. Depress Aanxiety. 2005; 21(4):185-92. [DOI:10.1002/da.20070] [PMID]
- Mohd Zulkifly MF, Ghazali SE, Che Din N, Singh DK, Subramaniam P. A review of risk factors for cognitive impairment in stroke survivors. Sci World J. 2016; 2016:3456943. [DOI:10.1155/2016/3456943] [PMID] [PMCID]
- Li W, Xiao WM, Chen YK, Qu JF, Liu YL, Fang XW, et al. Anxiety in patients with acute ischemic stroke: Risk factors and effects on functional status. Front Psychiatry. 2019; 10:257. [DOI:10.3389/fpsyt.2019.00257] [PMID] [PMCID]
- Kaur R, Shri R. Role of the genus cinnamomum in the management of neurodegenerative diseases: Outcomes and shortcomings. Indian J Pharm Sci. 2018; 80(6):984-95. [DOI:10.4172/pharmaceutical-sciences.1000448]
- Ryder KA, Gontkovsky ST, McSwan KL, Scott JG, Bharucha KJ, Beatty WW. Cognitive function in Parkinson’s disease: Association with anxiety but not depression. Aging Neuropsychol Cogn. 2002; 9(2):77-84. [DOI:10.1076/anec.9.2.77.9543]
- Quattropani MC, Geraci A, Lenzo V, Delle Chiaie R, Filastro A. Post-Stroke anxiety and depression: Relationships to cognitive rehabilitation outcome. Clin Neuropsychy J Treat Eval. 2018; 15(1):12-8. https://www.clinicalneuropsychiatry.org/download/post-stroke-anxiety-and-depression-relationships-to-cognitive-rehabilitation-outcome/
- Terroni L, Sobreiro MFM, Conforto AB, Adda CC, Guajardo VD, de Lucia MCS, et al. Association among depression, cognitive impairment and executive dysfunction after stroke. Dement Neuropsychol. 2012; 6(3):152-7. [DOI:10.1590/S1980-57642012DN06030007] [PMID] [PMCID]
- Rafsten L, Danielsson A, Sunnerhagen KS. Anxiety after stroke: A systematic review and meta-analysis. J Rehabil Med. 2018; 50(9):769-78. [DOI:10.2340/16501977-2384] [PMID]
- Chun HY, Whiteley WN, Dennis MS, Mead GE, Carson AJ. Anxiety after stroke: The importance of subtyping. Stroke. 2018; 49(3):556-64. [DOI:10.1161/STROKEAHA.117.020078] [PMID] [PMCID]
- Stein MB, Sareen J. Clinical Practice. Generalized anxiety disorder. N Engl J Med. 2015; 373(21):2059-68. [DOI:10.1056/NEJMcp1502514] [PMID]
- De Ronchi D, Palmer K, Pioggiosi P, Atti AR, Berardi D, Ferrari B, et al. The combined effect of age, education, and stroke on dementia and cognitive impairment no dementia in the elderly. Dement Geriatr Cogn Disord. 2007; 24(4):266-73. [DOI:10.1159/000107102] [PMID]
- Stern Y. Cognitive reserve in ageing and Alzheimer’s disease. Lancet Neurol. 2012; 11(11):1006-12. [DOI:10.1016/S1474-4422(12)70191-6]
- EClipSE Collaborative Members, Brayne C, Ince PG, Keage HA, McKeith IG, Matthews FE, et al. Education, the brain and dementia: Neuroprotection or compensation? Brain. 2010; 133(Pt 8):2210-6.[DOI:10.1093/brain/awq185] [PMID]
- Steffener J, Reuben A, Rakitin BC, Stern Y. Supporting performance in the face of age-related neural changes: Testing mechanistic roles of cognitive reserve. Brain Imaging Behav. 2011; 5(3):212-21. [DOI:10.1007/s11682-011-9125-4] [PMID] [PMCID]
- DeLuca J, Johnson SK, Ellis SP, Natelson BH. Cognitive functioning is impaired in patients with chronic fatigue syndrome devoid of psychiatric disease. J Neurol Neurosurg Psychiatry. 1997; 62(2):151-5. [DOI:10.1136/jnnp.62.2.151] [PMID] [PMCID]
- Kessels RP, Eikelboom WS, Schaapsmeerders P, Maaijwee NA, Arntz RM, van Dijk EJ, et al. Effect of formal education on vascular cognitive impairment after stroke: A meta-analysis and study in young-stroke patients. J Int Neuropsychol Soc. 2017; 23(3):223-38. [DOI:10.1017/S1355617716001016] [PMID]
Type of Study: Research |
Subject:
Physiotherapy
Received: 2020/09/27 | Accepted: 2021/11/10 | Published: 2020/12/29
Received: 2020/09/27 | Accepted: 2021/11/10 | Published: 2020/12/29








